Abstract
Background:
Palms and soles are the readily visible areas of the body that are affected in various dermatoses. This may have considerable concern to the patient and can cause diagnostic dilemma. Moreover, palmoplantar dermatoses also limit our day to day activities with a significant impact on quality of life.
Aim:
To study the clinical profile of patients suffering from palmoplantar dermatoses at a tertiary care centre.
Patients and Methods:
A prospective observational study was carried out from June 2014 to May 2015 in the Department of Dermatology, Venerology and Leprosy at a rural tertiary care centre after taking approval from the institutional ethical committee. In total, 202 cases were enrolled. The study was analyzed using Chi-square test.
Results:
A total of 202 patients were enrolled, among which 53.46% were males. The most common age group affected was 17–40 years (42.57%). Duration of less than 1 month was seen in 31.7% cases whereas 29.7% showed seasonal variation. The most common chief complaint was itching (69.8%). Palmoplantar psoriasis was the most common dermatosis with 28.22% cases, followed by keratinizing disorders with 26.72% cases. Palms were involved in 66.34% cases, soles in 69.30%, and both palms and soles in 37.12% cases. Other body parts were involved in 15.34% of the cases. Diabetes and hypertension were common comorbid conditions seen in 11.4% of the cases each.
Conclusion:
Palmoplantar psoriasis was the most common disorder affecting palms and soles followed by palmoplantar keratoderma.
Keywords: Keratinizing disorders, palmoplantar dermatosis, psoriasis
Introduction
Palms and soles are the readily visible areas of the body that are affected in various dermatoses. This may have considerable concern to the patient and can cause diagnostic dilemma at times. Moreover, palmoplantar dermatoses also limit our day to day activities, and thereby have a significant impact on the quality of life. Previous studies have focused on some specific palmoplantar dermatoses,[1,2] and none has performed a comprehensive study on dermatoses involving both the palms and soles. The present study attempted to study palmoplantar dermatoses involving all the disorders of the palms and soles with their demographic and clinicomorphological details, whether limited to palms and soles, spread to other sites of body, and associated with any systemic involvement or not.
Patients and Methods
The present study was a prospective observational study carried out from June 2014 to May 2015 in the department of Dermatology, Venerology and Leprosy at a rural tertiary care centre after taking approval from the institutional ethical committee. In total, 202 cases were enrolled during the 1-year period after obtaining informed written consent in vernacular language. Patients with palmoplantar dermatoses with or without other body part involvement of any age group and sex were included. Patients who were not willing to participate or did not give their written consent were excluded from the study. A detailed history was taken and a thorough clinical examination was done according to a prestructured proforma. Investigations such as KOH mount, wood's lamp examination, patch testing, and biopsy were done as and when required. The data was analyzed using Chi-square test.
Results
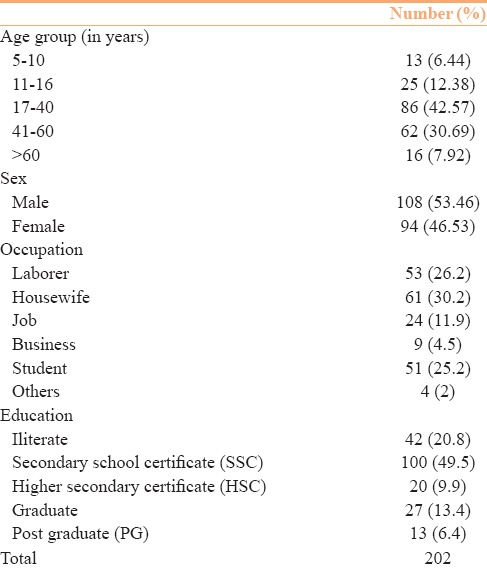
In total, 202 patients were enrolled in the study, of which 108 (53.46%) were males and 94 (46.53%) were females. The most common age group affected was 17–40 years in 86 (42.57%) cases followed by 41–60 years in 62 (30.69%) cases. Housewives were most commonly affected in 61 (30.2%) cases followed by laborers in 53 (26.2%) cases. Most of the patients were educated up to SSC 100 (49.5%) [Table 1].
Table 1.
Demographic details
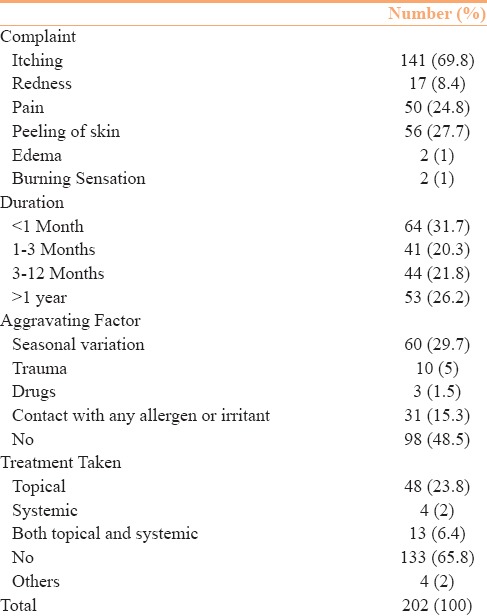
Most of the patients with palmoplantar dermatoses complained of itching in 141 (69.8%), followed by peeling of skin in 56 (27.7%). Sixty-four (31.7%) cases were having disease for less than 1 month whereas 53 (26.2%) had disease duration of more than 1 year. Only 60 (29.7%) patients showed seasonal variation whereas 98 (48.5%) had no known aggravating factor. Forty-eight (23.8%) patients were applying some topical medication whereas 133 (65.8%) had taken no treatment [Table 2]. One hundred forty-nine (73.8%) patients had progressive illness whereas in 53 (26.2%) cases it was nonprogressive. Associated comorbid conditions were seen in 48 (23.76%) patients, of which diabetes and hypertension was present in 23 (11.4%) cases each.
Table 2.
Clinical profile
Palmoplantar psoriasis was the most common dermatoses found in 57 (28.22%) cases followed by keratinizing disorders in 54 (26.72%). Palms were involved in 134 (66.34%) cases, soles in 140 (69.30%), and both palms and soles in 75 (37.12%) cases [Table 3]. Of the 134 cases with palmar involvement, 19 (9.4%) had unilateral whereas 115 (56.9%) had bilateral involvement. Single lesion was seen in 33 (16.34%) patients and 101 (50%) had multiple lesions. Of the 140 patients with sole involvement, 30 (14.9%) had unilateral whereas 110 (54.5%) had bilateral involvement [Figure 1]. Thirty-eight (18.81%) patients had single lesion and 102 (50.5%) had multiple lesions. Digits and web spaces (35.33%) followed by thenar (33.38%) and hypothenar (31.28%) areas over the palms and heels (25.72%) over soles were the most common sites to be involved [Figures 2 and 3]. Dorsum of hands and feet were involved in 78 (38.61%) and 54 (26.73%) cases, respectively. Nail involvement was seen in 64 (31.68%) cases, with fingernails being involved in 30 (46.87%) cases and toe nails in 34 (53.13%) cases. Ridges 42 (20.79%) and pitting 16 (7.92%) were common changes found in nails. Involvement of other body parts was seen in 31 (15.34%) cases.
Table 3.
Distribution of palmoplantar dermatoses
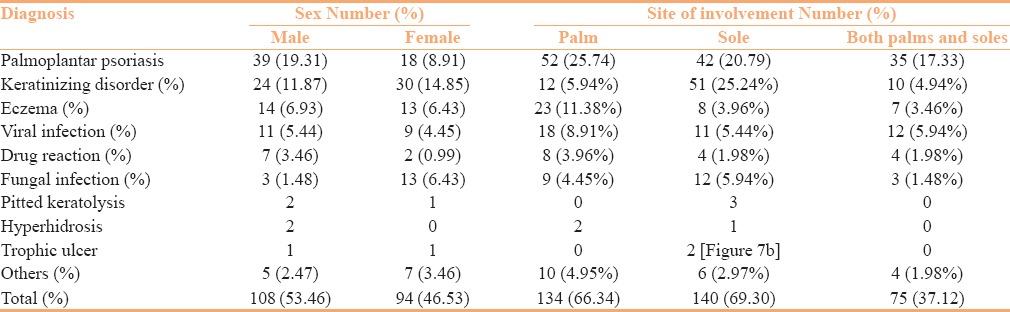
Figure 1.
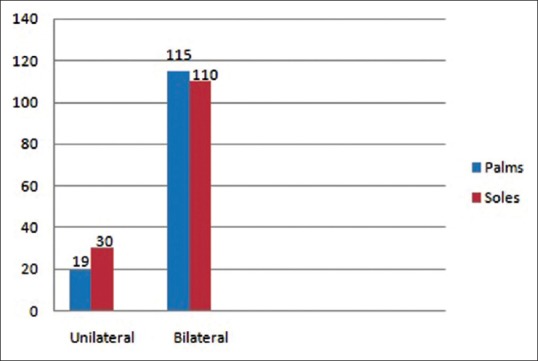
Dermatoses over the palms and soles
Figure 2.
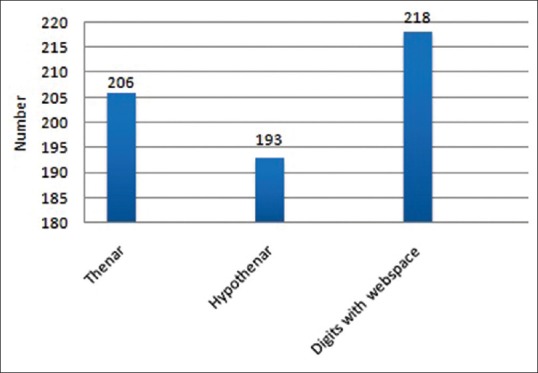
Distribution of dermatoses over the palms
Figure 3.
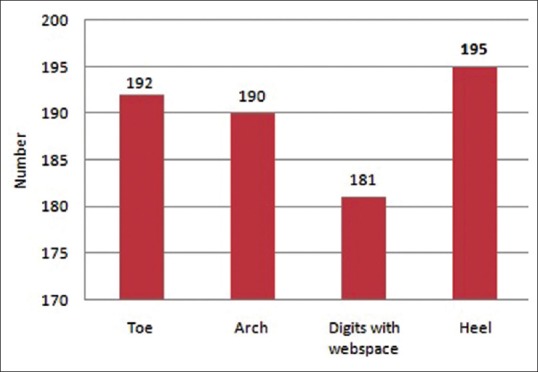
Distribution of dermatoses over the soles
We had conducted a noninterventional study and diagnosed the conditions clinically after obtaining detailed history and a thorough clinical examination. However, in 9 cases, there was a diagnostic dilemma, for which punch skin biopsies were taken and diagnosis was confirmed by histopathological examination.
Discussion
Palmoplantar dermatoses include all the skin diseases which involve palms and soles exclusively. Dermatosis which along with involvement of palms and soles also involves other body parts includes a range of conditions such as hyperhidrosis, keratinizing disorders; eczema, infections such as viral, fungal, bacterial, drug reactions, and many more. Many dermatological conditions pose minimal threat to patients in terms of mortality, but have the capacity to severely impinge on a patient's quality of life because of the disfiguring nature of skin pathology with its adverse impact on body image and burden on social function, which may be independent of clinical severity, including dermatosis involving the palms and soles. Routine day to day activities are affected and can lead to loss of daily wages in patients, particularly from rural areas such as ours.
Our study of 202 patients showed male preponderance of 53.46%, which was similar to other studies.[3,4,5,6] Male preponderance of palmoplantar dermatoses is probably because of their outdoor occupation and activities resulting in predisposition to trauma caused by manual labor or walking barefoot.
Middle age group, i.e., 17–40 years (42.57%), was the most common age group affected, with a mean age of 35.14 years that was comparable to Bong Seon Kang et al.[3] and Kodali et al.[5] having common age groups 40–59 years (36.2%) and 41–50 years (26%) and mean ages being 37.5 years and 43.72 years, respectively.
Palmoplantar dermatoses are very commonly seen in farmers and manual laborers as they are engaged in strenuous physical work and are exposed to various forms of trauma, friction, and chemicals. Similarly, housewives are also exposed to various detergents and water while doing washing and cleansing work. They frequently come in contact with vegetable juices which makes their palms and soles prone to various dermatosis. In our study, 30.2% were housewives and 26.2% were laborers and farmers. Chopra et al.[6] reported 48.16% manual workers such as laborers and farmers and 18.69% housewives. Similarly, Kodali et al.[5] reported 53% farmers 20% housewives as the commonly affected occupational groups with palmoplantar dermatoses. They also found palmoplantar keratoderma as the predominant dermatoses in laborers in accordance to the usual belief that more friction would cause hyperkeratosis of palms and soles.[7] This can be explained by the fact that pressure areas are more exposed to trauma and friction with koebner's phenomenon contributing to it, and maceration is commonly present over webspaces due to exposure to detergents and other chemicals.
Various studies[3,7,8] reported itching to be the predominant symptom in palmoplantar dermatoses whereas duration of complaints considerably varied and no specific trend was seen. Usually, palmoplantar dermatoses are chronic in nature, however in our study, most patients were having complains for less than 1 month (31.7%); whilein the study reported by Bong Seon Kang et al.[3] duration ranged from 2 days to 50 years. Psoriasis and eczema are usually aggravated in winters whereas fungal infections are seen commonly in summers; the same findings were present in various studies. We showed 29.7% cases exhibiting a seasonal variation.
In our study, while dividing dermatosis in broad groups, we found 28.22% cases presented with palmoplantar psoriasis, 26.72% cases with keratinizing disorders, 13.36% cases with eczema, 9.90% cases with viral infections, 7.92% cases with fungal infections [Figure 4a], and 4.45% cases with drug reactions. Among individual dermatoses, palmoplantar psoriasis [Figure 4b] was present in 28.22% cases followed by palmoplantar keratoderma with fissures in 17.33%, corn in 8.41%, irritant contact dermatitis in 6.93%, pompholyx, candidiasis and warts each in 5.45% cases [Figure 5a and b], and others including vitiligo and lichen planus [Figure 6a and b]. A study reported by Bong Seon Kang et al.[3] showed palmoplantar pustulosis with 23.2%, warts with 11.4%, pompholyx with 10.1%, palmoplantar keratoderma with 8.9%, and contact dermatitis with 8.0% cases; while in a study by Kodali et al.,[5] 52% cases were diagnosed as psoriasis, 31% as eczema, 11% as lichen planus, 2% as fungal infection, 2% as leprosy, and 1% as warts.
Figure 4.

(a) Tinea pedis; (b) Psoriasiform erythroderma involving the palms
Figure 5.

(a) Candidiasis of foot mimiking pitted keratolysis; (b) Plantar warts
Figure 6.

(a) Vitiligo over the hands; (b) Lichen planus over the palms
Palmoplantar keratodermas is a diverse entity of cutaneous disorders which are characterized by abnormal and excessive thickening of the skin over the palms and soles. It is classified into inherited and acquired disorders. Numerous diseases have been implicated as the cause of this common and interesting group. Acquired palmoplantar keratoderma in later years of life occurring due to the cumulative insult of constant exposure to trauma, allergens, and irritants may produce keratoderma.
Psoriasis of palms and soles present as erythematous sharply circumscribed plaques with silvery white scales and peripheral overhanging scale on the palms, sides of fingers, finger tips, and on extensor surfaces of joints.[9] Palmoplantar psoriasis is shown to constitute 3–4% of all psoriasis cases in most of the studies conducted.[10] In our study, among palmoplantar psoriasis, palms were involved in 52 (25.74) cases [Figure 7a], soles in 42 (20.79), and both palms and soles were involved in 35 (17.33) cases. In a study conducted by Kumar et al.,[11] plantar psoriasis was more common than palmar psoriasis. Equal incidence of palms and soles involvement was noticed in other studies. Out of the 403 cases studied by Anandan et al.[8] in his study of psoriasis, palmoplantar psoriasis constituted approximately 59% cases. Patients of palmoplantar psoriasis complain of irritation, pain, fissuring, and difficulty in walking and manual work.[11] Both palms and soles involvement was seen in 52% of the cases, exclusive palmar involvement was present in 28% cases whereas only plantar involvement in 20% cases as reported by Anandan et al.,[8] and lesions were symmetrically distributed in 79% cases. In a study by Kumar et al.,[11] plantar involvement was twice as common as palmar involvement. Sujay et al.[12] in their study of palmoplantar psoriasis found pressure areas commonly involved with 44% fingers, 11% thenar, and 15% hyothenar eminences, with centre and distal aspects of palms being less frequently affected. In soles instep, sides of feet heel were commonly affected, with distal sole and toes less commonly affected. Extension to dorsum was seen in 68% by sujay et al.,[12] and 45% by kumar et al.[11] Webspace involvement was seen in 28% by sujay et al.[12] and 8% by kumar et al.[11] Webspace involvement leads to high prevalence of maceraton in a tropical country like ours and to the design of Indian footwear.
Figure 7.

(a) Psoriasis over the palms; (b) Trophic ulcer over the soles
We had 6 patients of hand foot mouth diseases with palmoplantar involvement in the form of vesicles with fever, sore throat, and ulcers in the mouth. In most of the studies, it is only the palms and dorsum of hands which are commonly affected.[13]
Involvement of palms and soles is thought to be uncommon in Lichen planus (LP).[14] In a study by Gutte et al.,[15] exclusive palm or sole involvement was found in 4 out of 18 patients, whereas in our study, we found 3 patients of lichen planus, 2 over soles and 1 over the palm. Palmoplantar LP has varied morphological presentations apart from classically described yellowish hyperkeratotic papules and plaques.
Conclusion
Middle-aged males were the most common affected group. Palmoplantar psoriasis was the most common dermatosis followed by palmoplantar keratoderma with fissuring. Palms were involved in 66.34% cases, soles in 69.30%, and both palms and soles in 37.12% cases. Diagnosis of palmoplantar dermatoses is important at the earliest for appropriate management which helps in improving the patient's quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kumar B, Saraswat A, Kaur I. Palmoplantar lesions in psoriasis: A study of 3065 patients. Acta Derm Venereol. 2002;82:192–5. doi: 10.1080/00015550260132488. [DOI] [PubMed] [Google Scholar]
- 2.Valia RG. Eczema. In: Valia RG, Valia AR, editors. IADVL Text Book of dermatology. 3rd edition. India: Bhalani Publishing house; 2008. pp. 490–526. [Google Scholar]
- 3.Kang BS, Lee JD, Cho SH. A Clinicopathological Study of Palmoplantar Dermatoses. Korean J Dermatology. 2006;44:714–20. [Google Scholar]
- 4.Mahajan PM, Gharpuray MB, Kulkarni V. Clinical and histopathological study of palmoplantar keratoderma. Indian J Dermatol Venereol Leprol. 1994;60:258–61. [Google Scholar]
- 5.Kodali S. A Clinico-Histopathological Study of Acquired Palmoplantar Keratoderma in a Rural-Based Tertiary Hospital. J Evolution Med Dent Sci. 2014;30:8500–5. [Google Scholar]
- 6.Chopra A, Maninder, Gill SS. Hyperkeratosis of palms and soles: Clinical study. Indian J Dermatol Venereol Leprol. 1997;63:85–8. [PubMed] [Google Scholar]
- 7.Samanta BC, Banerjee BN, Panja RK. Etiology of plantar keratoderma. Ind J Dermatol Venereol Leprol. 1976;42:116–25. [PubMed] [Google Scholar]
- 8.Venkatesan A, Aravamudhan R, Perumal SK, Kannan R, Thirunavukkarasu V, Shukla S. Palmoplantar Psoriasis- Ahead in the Race-A Prospective Study from a Tertiary Health Care Centre in South India. J Clin Diagn Res. 2015;9:WC01–3. doi: 10.7860/JCDR/2015/11716.5669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farber EM, Nall ML. Natural history of psoriasis in 5600 patients. Dermatologica. 1974;148:1–18. doi: 10.1159/000251595. [DOI] [PubMed] [Google Scholar]
- 10.Suman Babu PS, Reddy S. Clinico Epidemiological Study of Palmoplantar Psoriasis. J Evid Based Med Healthc. 2014;1:656–60. [Google Scholar]
- 11.Kumar B, Saraswat A, Kaur I. Palmoplantar lesions in psoriasis: A study of 3065 patients. Acta Derm Venereol. 2002;82:192–5. doi: 10.1080/00015550260132488. [DOI] [PubMed] [Google Scholar]
- 12.Khandpur S, Singhal V, Sharma VK. Palmoplantar involvement in psoriasis: A clinical study. Indian J Dermatol Venereol Leprol. 2011;77:625. doi: 10.4103/0378-6323.84071. [DOI] [PubMed] [Google Scholar]
- 13.Kar B, Dwibedi B, Kar S. An Outbreak of Hand, Foot and Mouth Disease in Bhubaneswar, Odisha. Indian Pediatr. 2013;50:139–42. doi: 10.1007/s13312-013-0033-0. [DOI] [PubMed] [Google Scholar]
- 14.Sánchez-Pérez J, Rios Buceta L, Fraga J, García-Díez A. Lichen planus with lesions on the palms and/or soles: Prevalence and clinicopathological study of 36 patients. Br J Dermatol. 2000;142:310–4. doi: 10.1046/j.1365-2133.2000.03303.x. [DOI] [PubMed] [Google Scholar]
- 15.Gutte R, Khopkar U. Predominant palmoplantar lichen planus: A diagnostic challenge. Indian J Dermatol. 2014;59:343–7. doi: 10.4103/0019-5154.135477. [DOI] [PMC free article] [PubMed] [Google Scholar]


