Abstract
Purpose:
The purpose of this study was to determine the effectiveness of preventing eye injury with the use of safety eyewear in agriculture workers.
Methods:
A sample group of 575 agricultural workers (Group A) engaged in harvesting paddy were provided with goggles with side covers. Following harvesting, a questionnaire-based survey was carried out to determine the frequency of their eye injuries. Workers with goggles were asked about the duration for which they used the goggles and also list barriers or difficulties with the same. The frequency of eye injuries in this group was compared with another group of agriculture workers (Group B) who did not use any safety eyewear.
Results:
The frequency of eye injuries in Group A was 4 (0.7%) and Group B was 61 (11.3%) which was highly significant (P = 0.0001). The relative risk calculated was 0.06 (95% confidence interval: 0.02–0.2). Agricultural workers in Group A had 94% less risk of ocular trauma compared to those in Group B. Injuries in both groups were caused by parts of the paddy plant. A significant number (76.2%) of workers used the goggles all or most of the time during work. Impaired vision when wearing goggles was the most frequent barrier reported by the workers. Other barriers were discomfort, shyness, forgetfulness, apathy, slowing of work pace, awkward appearance, and breakages.
Conclusion:
Safety eyewear conferred significant protection against work-related eye injuries in agriculture. Although safety eyewear was widely adopted by the workers, barriers reported by them will need to be addressed to make such programs more effective.
Keywords: Agriculture, eye injuries, goggles, primary prevention, safety eyewear
Worldwide agriculture ranks among the most hazardous occupations alongside mining, manufacturing, and construction in the prevalence of work-related eye injuries.[1,2,3,4,5] In developed countries where most farming practices are mechanized, eye injuries are mostly machine-related, either open or closed globe injuries.[6,7,8] In contrast, in the developing countries with a lesser degree of mechanization, corneal ulceration is a more common manifestation.[5,9,10,11,12,13] For example, in southeast Asia where paddy cultivation is predominant, injury from the paddy leaf during harvesting causes corneal abrasion which gets secondarily infected from lack of care or the use of traditional eye medicines.[10,11,12,13] The resultant corneal ulcer (harvest ulcer,[14] or rice-harvesting keratitis[11]) is a significant cause of ocular morbidity and visual impairment.[10,11,12,15,16,17] Work-related injuries in agriculture result in huge economic losses,[18,19] placing an enormous burden on the agrarian community across the world.
Work-related eye injuries can be prevented by wearing safety eyewear like goggles.[20,21,22,23,24,25] While the use of safety eyewear is universally known and advocated by industry, compliance with safety guidelines among workers is poor.[21,22,23,24,25] The reasons are behavioral (indifference and lack of awareness of workplace hazards and safety), lack of safety eyewear in workplaces or inappropriate design of the same.
Compared to other occupations, the use of safety eyewear among agricultural workers is less prevalent,[3,6,26,27,28,29] and almost nonexistent in India.[5,17] We believe that its use will protect workers from work-related injuries and consequent morbidity. Studies evaluating safety eyewear usage in agriculture come mostly from the West,[26,27,28,29,30,31,32] but because of the different farming practices and sociocultural characteristics, their results cannot be directly extrapolated to the Indian scenario. We are not aware of any study evaluating the use of safety eyewear among Indian agricultural workers. Therefore, the purpose of this study is to evaluate the effectiveness of safety eyewear in Indian agricultural workers and identify barriers to its use.
Methods
This prospective comparative study between two groups randomly allocated to goggles-wear and no goggles-wear was carried out in three villages in Chhattisgarh in central India between 2010 and 2011. In these villages, agriculture is the chief occupation, with rice as the principal crop. Here, rice cultivation is predominantly manual. The study villages were populated mainly by small, marginal farmers or agricultural laborers, and socioeconomic conditions were common to those of the rest of the country.
The study was approved by the Institute Ethics Committee and followed the principles of the Declaration of Helsinki. Initially, permission was obtained from the village administration or panchayat, and then from the head of the agricultural households. The risk and consequences of eye injuries during farming and the purpose of the study was explained to all in detail. The sample size was determined considering the prevalence of eye injury at 11% based on a previously published study.[17] It was assumed that goggles wear would confer eye protection to the workers, and the prevalence of injury would reduce to nil and therefore a pooled estimate of 5% was considered as baseline estimate for sample size calculation. As the study population was distributed over three villages, a design effect of 1.5 was taken and with 5% effect size, 80% power, 95% confidence interval, and 10% nonresponse rate, and sample size calculation yielded a sample of 500 subjects. The allocation of subjects to each group was randomly done. All households with agricultural workers were pooled and enumerated with the help of the electoral rolls at the village administrative center. Each worker in the households was assigned a random number generated through a Microsoft Excel spreadsheet. Then, on the basis of simple randomization, 575 workers were selected in the study group (Group A). Although 500 subjects fulfilled the sample size, additional workers were recruited to compensate for a higher nonresponse rate than what had been anticipated during sample size calculation. All the adults engaged in farming were enrolled after their consent. Subjects already using spectacles were excluded. Those who refused consent were also excluded and replaced by the next worker.
All workers were provided with a pair of nontinted polycarbonate goggles with side covers (Innovision Ltd., Mumbai, India), [Fig. 1a and b]. The distribution of goggles was done in October 2010 before harvesting, because the highest frequency of ocular injuries is reported during this phase.[9,10,11,12,13] While harvesting manually, the worker needs to bend forward from the waist [Fig. 2a] which predisposes the eye to injury from the plant stalk or leaf. The study goggles had side covers that protected the eyes from all directions [Fig. 2b]. The workers were instructed to wear the goggles all the time during harvesting work. Each morning, volunteers stood at the exit roads of the villages to remind workers to carry the goggles to work. Members from the study team made random visits to monitor the use of goggles. They also conducted regular awareness meetings, group discussions, house visits, and pamphlet distribution to motivate the workers. Telephone numbers were shared by the study team to provide emergency eye care. After completing data collection, a screening camp for eye diseases was carried out in the villages.
Figure 1.

The safety eyewear or goggles used in the study, a) from the front and b) from the sides
Figure 2.
Agriculture-workers harvesting paddy without goggles (a) and with goggles (b)
In March-April of the following year, after cessation of all harvesting-related activities, a questionnaire-based survey to collect information on the frequency of eye injury, duration of goggles wear, and barriers was carried out by Vision technicians (persons trained for 1 year to provide eye care in rural areas). To achieve a 1:1 ratio between cases and controls, another group of 575 subjects from the existing list of agricultural workers not included in Group A were selected to act as controls (Group B). All the interviewers spoke the local dialect and were trained in the survey procedure. Each household was visited by vision technicians and agricultural workers were interviewed individually. In case of absence of the individual, a second attempt to interview the subject was made, and if that failed, it was considered as a nonresponse. The frequency of eye injury was obtained by asking “Did you suffer from any eye injury during harvesting,” a method used in a previous study.[16] Injuries to other parts of the body or injuries incurred during activities other than farming or outside the study period were excluded. The duration of goggles wear was categorized as: (1) all the time, if the participants spoke of using them at work for the entire duration; (2) most of the time, if they used them most but not at all times; (3) half of the time, if they used them for half the duration; (4) some time, if they used them infrequently; and (5) none of the time, if they did not use them at all.[3] Finally, each worker was asked to list difficulties encountered while wearing the goggles or reasons for not wearing them. The responses were closely matched by the interviewer to a preexisting list. If a response was not present on the list, it was recorded separately.
Statistical analysis
Data analysis was performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). Fisher's exact test was used to test the difference in frequencies between two groups, while central tendencies were tested with Student's t-test and difference in proportions with z test. A two-sided P < 0.05 was considered to be statistically significant.
Results
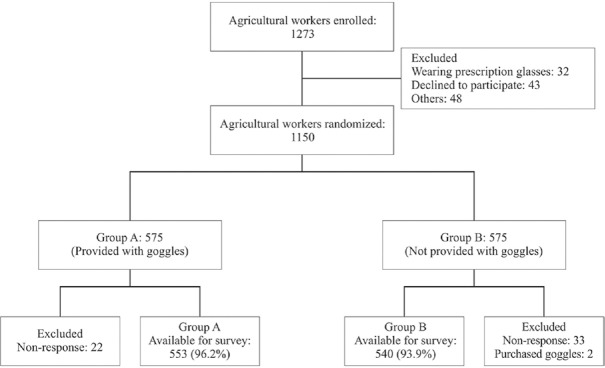
A total of 1150 subjects were enrolled in the study, and after exclusion, they were allocated randomly to the two groups [Fig. 3]. Postharvesting, 553 (96.2%) workers in Group A and 542 (94.3%) workers in Group B were available for the survey. Two workers from Group B were excluded from the study when it was later discovered that they had also been using goggles purchased from the local market. There were 290 (52.4%) males and 263 (47.7%) females in Group A with a mean age of 41.2 ± 13.2 years and 289 (53.2%) males and 251 (46.5%) females in Group B with a mean age of 40.9 ± 13.9 years. The groups were homogeneous in terms of age (P = 0.67) and gender (P = 0.77).
Figure 3.
Flowchart of patient disposition
The number of ocular injuries in Group A was 4 (0.7%) and 61 (11.3%) in Group B, which was statistically significant (P = 0.0001). The relative risk was 0.06 (95% confidence interval: 0.02–0.2), signifying that agricultural workers in Group A had 94% less risk of ocular trauma compared to those in Group B. The four cases of injury in Group A occurred when the participants were not wearing their goggles. Three of the injuries in Group A occurred during harvesting and one during threshing. In Group B, 56 (91.8%) injuries occurred during harvesting and 5 (8.2%) during threshing. Two injuries in this group developed into fungal corneal ulcers which were treated and healed. Three workers in this group reported an injury on more than one occasion. Overall, the injuries were caused by paddy leaf in 47 (72.3%), paddy ears in 11 (16.9%), paddy husk in 3 (4.6%), hay stalk in 1 (1.5%), and unknown foreign bodies in 3 (4.6%) cases.
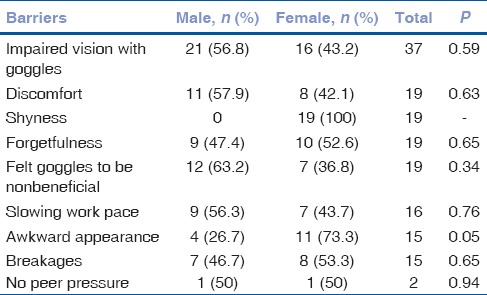
The duration of goggles wear by the workers is shown in Table 1. No pattern based on gender was observed related to use of goggles in the study population. About three-fourths of the workers used the goggles all or most of the time. On further, evaluating the duration of goggle wear within individual households, it was seen that members of 132 (80.1%) households reported similar wearing time while members of 25 (15.1%) households reported varying time. Eight households were excluded as there was only one working member. A majority of the agricultural workers did not report a barrier, and those reported by 156 (28.2%) workers and their distribution between male and female workers are shown in Table 2. Some workers reported more than one barrier. Overall, impaired vision during work due to fogging and slippage of the goggles was the most commonly reported barrier, while female workers reported feeling conscious because of their unaccustomed appearance on wearing the goggles.
Table 1.
Gender-wise distribution of duration of goggles wear by agricultural workers in Group A (n=553)
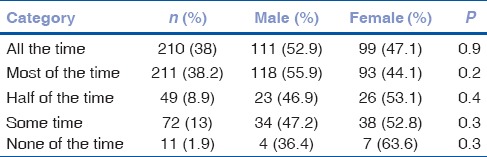
Table 2.
Gender-wise distribution of barriers reported by agricultural workers
Discussion
The frequency of eye injuries in agricultural workers wearing goggles was significantly less than those not using goggles. A majority of the agricultural workers in the study wore the goggles for sufficient time during work. This is notable as none of them were acquainted with any form of personal protective equipment nor exposed to workplace-related safety training before the study.
Several studies have reported the effectiveness of safety eyewear in the workplace, identifying it as the only factor that confers protection to the worker from eye injuries.[22,23,24,25,33,34] In agriculture, the use of safety eyewear is variable and generally low. Even in the United States, where there are strict safety requirements at the workplace, safety eyewear use is reported to range from as low as 2% to 50%.[3,29] Although comparable data are not available for India, usage of protective eyewear among Indian farmers is very low. A study from India reported that a majority of individuals incurring eye injuries residing in rural areas did not use any eye protection.[17] Forst et al. have categorized factors which govern agricultural workers wearing or not wearing protective eyewear like goggles as perception of risk and the expected effectiveness of goggles to reduce that risk, availability of goggles at the workplace and a mandate to use them, impact on visual acuity, comfort and appearance, and the need to carry them to the workplace.[27] Similar barriers have also been reported in other studies[26,28,29] and in the present one as well. Design-related shortcomings in protective eyewear hamper work and are an important concern for agricultural workers. Health and safety concerns come second to economic considerations and pressure to complete the work at hand.[28] In hot and humid climates, goggles tend to fog or get dirty, obscure vision due to sweat and tend to slip down the nose, all of which slow the work pace and cause workers not to use them.[29] In the present study, impaired vision due to goggles was the most common barrier reported by workers [Table 2]. Some of the other barriers included discomfort and slow work pace. The design of the goggles [Fig. 1] used in this study is limited by lack of a head strap to prevent slippage, which was reported by the workers in the study, and absence of venting holes, due to which the goggles tended to fog. While harvesting paddy in hot, humid weather, workers bend down from the waist [Fig. 2], and then these design-related flaws become important barriers to the acceptance of goggles among the workers. Therefore, due attention must be paid to the design of the goggles, and further studies are required to design appropriate protective eyewear for agricultural workers in Indian conditions. This design should also allow for concomitant wear of refractive correction if any by the worker. While some male agricultural workers reported awkwardness due to unfamiliarity, it was more common among female workers. Such gender difference is not unusual as women in rural India rarely use goggles or sunglasses. As mentioned, eye protection is not common in rural India, which is a significant cultural barrier that needs to be addressed in future programs.
None of the workers in this study suffered eye injuries while wearing the goggles, but four suffered injuries when they were not wearing them. Studies in different occupational settings have also reported gaps in eye protection at the workplace caused by disregard for work-related dangers, forgetfulness, or reduced risk perception.[23,24] Welch et al. observed that workers tended to use eye protection only when they perceived the task to be risky.[24] Behavior-related barriers can be overcome by imparting safety training to workers. Some studies have noted that safety training at the workplace is effective in changing workers' attitude toward safety measures and motivates them to actively adopt the same in daily work.[25,30,31,32,33,34,35] In the present study, safety training was provided through group and one-on-one discussions by volunteers, pamphlets in the local language and intermittent field monitoring. However, it seems that more robust awareness programs need to be implemented to promote safety eyewear in the rural population and this can be combined with other primary eye care programs.
In this study, workers belonging to the same household tended to report uniform wearing time. This has important connotations in the sociocultural scenario of rural India. The reason for uniform wearing time within the household lies in the social structure of rural India where the family is patriarchal, and the closely-knit community often displays herd behavior. The active support for the study from the village administration was one of the reasons behind the high usage rate of the goggles. Agriculture in India lacks an organizational structure that is similar to other industries. Most of the farms are run by marginal farmers who are often illiterate and follow traditional practices. Therefore, safety education for the community as a whole and participation by all its members becomes crucial to promoting safety eyewear. Stallones et al. have observed in their study that sociocultural differences among farming populations influence perceptions of health, safety, and treatment preferences.[28] Community health workers have been used to model safe behavior by wearing safety eyewear at all times during work, distributing goggles to fellow workers, and encouraging them to wear them in a few reports from the United States.[29,30,31,32] Such role models were successful in changing workers' perception of personal protection in the United States. This is because community health workers, with their intimate knowledge of farming practices and members of the community, can make personal connections with other workers and overcome language and cultural barriers more effectively than traditional health providers.[29] Although this model was not adopted in the present study, we feel that such role models will promote safety eyewear among Indian agricultural workers as well.
This study has limitations inherent to its design. It would have been ideal to conduct a randomized trial over a larger area to gain a more representative population. Although the questionnaire-based survey was conducted immediately after harvesting, recall bias may still confound the results. The results of wearing time of the goggles could be more precise if monitoring had been done by means of a daily log, but such an approach was not feasible. Furthermore, the workers could have falsely reported a higher wear time to please interviewers. The study was carried out during rice harvesting, and therefore, extrapolation of these findings to different phases of crop cycle or crops should be done cautiously. Nevertheless, the inclusion of a control group, an adequate sample size, and the setting in a developing country make the findings of our study relevant to agricultural populations with similar characteristics. Previous studies in southeast Asia have successfully shown that prophylactic treatment with topical antibiotics prevented corneal abrasions progressing to ulceration in the rural community.[13] Our study extends this concept of prevention of corneal ulcers a step further by attempting to prevent eye injuries altogether. This may significantly lessen corneal blindness in this region.
Conclusion
This study has clearly demonstrated that goggles are effective in lessening work-related eye injuries during farming and that agricultural workers can be motivated to use them at work. Barriers existing in particular communities need to be adequately addressed. Hazards in agriculture and their prevention in developing countries need to be studied more extensively to provide comprehensive safety guidelines.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. Anupam Sahu, Consultant, MGM Eye Institute, for helping during data collection; Dr. Sannapaneni Krishnaiah, Phd., Sankara Eye Foundation, Coimbatore, for sample size calculation; Dr. B. R. Shamanna, Professor, School of Health Sciences, University of Hyderabad, Hyderabad, for reviewing the manuscript; Mr. Tukaram Chauhan, Sonbhatta for assistance during field work; and the residents of the 3 villages for participating in the study.
References
- 1.Islam SS, Doyle EJ, Velilla A, Martin CJ, Ducatman AM. Epidemiology of compensable work-related ocular injuries and illnesses: Incidence and risk factors. J Occup Environ Med. 2000;42:575–81. doi: 10.1097/00043764-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Forrest KY, Cali JM. Epidemiology of lifetime work-related eye injuries in the U. S. population associated with one or more lost days of work. Ophthalmic Epidemiol. 2009;16:156–62. doi: 10.1080/09286580902738175. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Eye injuries to agricultural workers – Minnesota, 1992-1993. MMWR Morb Mortal Wkly Rep. 1995;44:364–6. [PubMed] [Google Scholar]
- 4.Solomon C. Accidental injuries in agriculture in the UK. Occup Med (Lond) 2002;52:461–6. doi: 10.1093/occmed/52.8.461. [DOI] [PubMed] [Google Scholar]
- 5.Vasu U, Vasnaik A, Battu RR, Kurian M, George S. Occupational open globe injuries. Indian J Ophthalmol. 2001;49:43–7. [PubMed] [Google Scholar]
- 6.Saari KM, Aine E. Eye injuries in agriculture. Acta Ophthalmol Suppl. 1984;161:42–51. doi: 10.1111/j.1755-3768.1984.tb06783.x. [DOI] [PubMed] [Google Scholar]
- 7.Schelp L. The occurrence of farm – Environmental injuries in a Swedish municipality. Accid Anal Prev. 1992;24:161–6. doi: 10.1016/0001-4575(92)90033-f. [DOI] [PubMed] [Google Scholar]
- 8.Sprince NL, Zwerling C, Whitten PS, Lynch CF, Burmeister LF, Gillette PP, et al. Farm activities associated with eye injuries in the Agricultural Health Study. J Agromedicine. 2008;13:17–22. doi: 10.1080/10599240801986025. [DOI] [PubMed] [Google Scholar]
- 9.Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol. 2004;88:456–60. doi: 10.1136/bjo.2003.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Upadhyay MP, Karmacharya PC, Koirala S, Tuladhar NR, Bryan LE, Smolin G, et al. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991;111:92–9. doi: 10.1016/s0002-9394(14)76903-x. [DOI] [PubMed] [Google Scholar]
- 11.Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8. doi: 10.1111/j.1442-9071.1992.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 12.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 13.Srinivasan M, Upadhyay MP, Priyadarsini B, Mahalakshmi R, Whitcher JP. Corneal ulceration in south-east Asia III: Prevention of fungal keratitis at the village level in South India using topical antibiotics. Br J Ophthalmol. 2006;90:1472–5. doi: 10.1136/bjo.2006.103028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joseph T. Paddy grain injury of the eye. A study of 277 cases. Br J Ophthalmol. 1968;52:191–7. doi: 10.1136/bjo.52.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dandona R, Dandona L. Corneal blindness in a Southern Indian population: Need for health promotion strategies. Br J Ophthalmol. 2003;87:133–41. doi: 10.1136/bjo.87.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, et al. Ocular trauma in a Rural South Indian population: The Aravind Comprehensive Eye Survey. Ophthalmology. 2004;111:1778–81. doi: 10.1016/j.ophtha.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of Southern India: The Andhra Pradesh Eye Disease Study. Ophthalmology. 2006;113:1159–64. doi: 10.1016/j.ophtha.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 18.Leigh JP, McCurdy SA, Schenker MB. Cost of occupational injuries in agriculture. Public Health Rep. 2001;116:235–48. doi: 10.1016/S0033-3549(04)50039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tiwari PS, Gite LP, Dubey AK, Kot LS. Agricultural injuries in Central India: Nature, magnitude, and economic impact. J Agric Saf Health. 2002;8:95–111. doi: 10.13031/2013.7221. [DOI] [PubMed] [Google Scholar]
- 20.Lehtonen KE. Practical principles of the prevention of occupational eye injuries. Acta Ophthalmol Suppl. 1984;161:38–41. doi: 10.1111/j.1755-3768.1984.tb06782.x. [DOI] [PubMed] [Google Scholar]
- 21.Henderson D. Ocular trauma: One in the eye for safety glasses. Arch Emerg Med. 1991;8:201–4. doi: 10.1136/emj.8.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de la Hunty D, Sprivulis P. Safety goggles should be worn by Australian workers. Aust N Z J Ophthalmol. 1994;22:49–52. doi: 10.1111/j.1442-9071.1994.tb01695.x. [DOI] [PubMed] [Google Scholar]
- 23.Fong LP, Taouk Y. The role of eye protection in work-related eye injuries. Aust N Z J Ophthalmol. 1995;23:101–6. doi: 10.1111/j.1442-9071.1995.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 24.Welch LS, Hunting KL, Mawudeku A. Injury surveillance in construction: Eye injuries. Appl Occup Environ Hyg. 2001;16:755–62. doi: 10.1080/10473220117500. [DOI] [PubMed] [Google Scholar]
- 25.Yu TS, Liu H, Hui K. A case-control study of eye injuries in the workplace in Hong Kong. Ophthalmology. 2004;111:70–4. doi: 10.1016/j.ophtha.2003.05.018. [DOI] [PubMed] [Google Scholar]
- 26.Quandt SA, Elmore RC, Arcury TA, Norton D. Eye symptoms and use of eye protection among seasonal and migrant farmworkers. South Med J. 2001;94:603–7. [PubMed] [Google Scholar]
- 27.Forst L, Noth IM, Lacey S, Bauer S, Skinner S, Petrea R, et al. Barriers and benefits of protective eyewear use by Latino farm workers. J Agromedicine. 2006;11:11–7. doi: 10.1300/J096v11n02_04. [DOI] [PubMed] [Google Scholar]
- 28.Stallones L, Acosta MS, Sample P, Bigelow P, Rosales M. Perspectives on safety and health among migrant and seasonal farmworkers in the United States and México: A qualitative field study. J Rural Health. 2009;25:219–25. doi: 10.1111/j.1748-0361.2009.00221.x. [DOI] [PubMed] [Google Scholar]
- 29.Monaghan PF, Bryant CA, McDermott RJ, Forst LS, Luque JS, Contreras RB. Adoption of safety eyewear among citrus harvesters in rural Florida. J Immigr Minor Health. 2012;14:460–6. doi: 10.1007/s10903-011-9484-3. [DOI] [PubMed] [Google Scholar]
- 30.Forst L, Lacey S, Chen HY, Jimenez R, Bauer S, Skinner S, et al. Effectiveness of community health workers for promoting use of safety eyewear by Latino farm workers. Am J Ind Med. 2004;46:607–13. doi: 10.1002/ajim.20103. [DOI] [PubMed] [Google Scholar]
- 31.Monaghan PF, Forst LS, Tovar-Aguilar JA, Bryant CA, Israel GD, Galindo-Gonzalez S, et al. Preventing eye injuries among citrus harvesters: The community health worker model. Am J Public Health. 2011;101:2269–74. doi: 10.2105/AJPH.2011.300316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tovar-Aguilar JA, Monaghan PF, Bryant CA, Esposito A, Wade M, Ruiz O, et al. Improving eye safety in citrus harvest crews through the acceptance of personal protective equipment, community-based participatory research, social marketing, and community health workers. J Agromedicine. 2014;19:107–16. doi: 10.1080/1059924X.2014.884397. [DOI] [PubMed] [Google Scholar]
- 33.Chen SY, Fong PC, Lin SF, Chang CH, Chan CC. A case-crossover study on transient risk factors of work-related eye injuries. Occup Environ Med. 2009;66:517–22. doi: 10.1136/oem.2008.042325. [DOI] [PubMed] [Google Scholar]
- 34.Lipscomb HJ. Effectiveness of interventions to prevent work-related eye injuries. Am J Prev Med. 2000;18(4 Suppl):27–32. doi: 10.1016/s0749-3797(00)00138-0. [DOI] [PubMed] [Google Scholar]
- 35.Adams JS, Raju R, Solomon V, Samuel P, Dutta AK, Rose JS, et al. Increasing compliance with protective eyewear to reduce ocular injuries in stone-quarry workers in Tamil Nadu, India: A pragmatic, cluster randomised trial of a single education session versus an enhanced education package delivered over six months. Injury. 2013;44:118–25. doi: 10.1016/j.injury.2011.10.001. [DOI] [PubMed] [Google Scholar]