Abstract
Surgical knee arthroscopy is among the most commonly performed procedures in the United States. The decision to treat is often based on clinical examination and magnetic resonance imaging. Equivocal results frequently require patients to undergo surgical arthroscopy, exposing the patient to inherent risks and potential surgical complications. Office-based needle arthroscopy provides an alternative approach to visualizing intra-articular anatomy and pathology in real time. The purpose of this article is to provide a standardized diagnostic approach to needle arthroscopy of the knee.
Surgical knee arthroscopy is among the most commonly performed procedures in the United States. In 2006, the National Survey of Ambulatory Surgery reported that approximately 1 million knee arthroscopies were performed, up nearly 49% from 1996.1, 2 The decision to treat for a majority of these procedures was based on a thorough physical examination followed by magnetic resonance imaging (MRI) to provide a confirmatory diagnosis. Previous studies have demonstrated MRI to have a sensitivity and specificity of 86% and 91%, respectively, for the diagnosis of ligamentous and meniscal tears.3 However, regular use of MRI has led to increased health care expenditures and a larger financial burden for patients, which ultimately can lead to delay in diagnosis.4 Other limiting factors precluding the use of MRI include patients who are morbidly obese, claustrophobic, renally impaired, or have implanted medical devices that are incompatible with MRI (Table 1). Furthermore, patients who have had recent or previous surgery to the joint in question can have less than definitive findings on subsequent MRI. Conversely, there are limited situations in which an in-office diagnostic arthroscope would be inferior to traditional MRI or MRI-arthrogram. Such instances would be suspected insufficiency fractures of the subchondral bone, avascular necrosis, or to evaluate bony incorporation of a previously placed bone graft.
Table 1.
Indications for Office-Based Needle Arthroscopy
| Office-based needle arthroscopy provides an alternative method for visualization of intra-articular structures. The table lists (but is not limited to) indications for which this procedure may be beneficial. | |
| Non-MRI candidates | Claustrophobia Pacemaker/internal defibrillator Metal implants Anxiety |
| Patients with suspected pathologies | Meniscal tears Cruciate ligament tears Articular cartilage defects Loose bodies Osteoarthritis |
| Arthritic patients who are candidates for: | Arthroscopy Unicompartmental knee replacement Total knee replacement High tibial osteotomy |
| Cartilage repair patients planning and assessment | ACI procedure planning Regenerative procedures Analyzing size, depth, and severity of defect Second-look evaluations status post procedure |
| Existing negative MRI with continued pain | |
| Postsurgical evaluation | |
NOTE. The table lists select indications for which this procedure may be beneficial.
ACI, autologous chondrocyte implantation; MRI, magnetic resonance imaging.
Small-bore needle arthroscopy has previously been described as a cost-effective, alternative diagnostic tool with demonstrated similar efficacy and accuracy to MRI and standard arthroscopes.4, 5 The procedure is carried out using a disposable hand piece attached to a reusable tablet to allow for ease of transport and visualization (Table 2). It provides physicians with real-time visualization of the patient's anatomy in an office-based setting. This ultimately reduces the time from injury to recovery, as patients can be scheduled to undergo surgical intervention or begin conservative treatment sooner. However, no literature has been published to describe a standardized technique for performing an office-based, diagnostic needle arthroscopy. We aim to provide a surgical guide for performing a standardized diagnostic needle arthroscopy of the knee, and to offer pearls to optimize visualization of intra-articular anatomy.
Table 2.
Needle Arthroscope Overview
| Specifications of the needle arthroscope are listed in the table. Of note, the viewing angle is 0°, compared with the 30° viewing angle commonly used in standard arthroscopy. |
| Disposable handpiece with re-usable tablet |
| 14-gauge retractable needle |
| 15 mm set focal length from the tip of the device |
| 0° arthroscopic view |
| 120° field of view |
| Single entry and visualization system, with camera and light source built into the handpiece |
| Still images or 15 minutes of video can be taken during the procedure and saved |
Technique
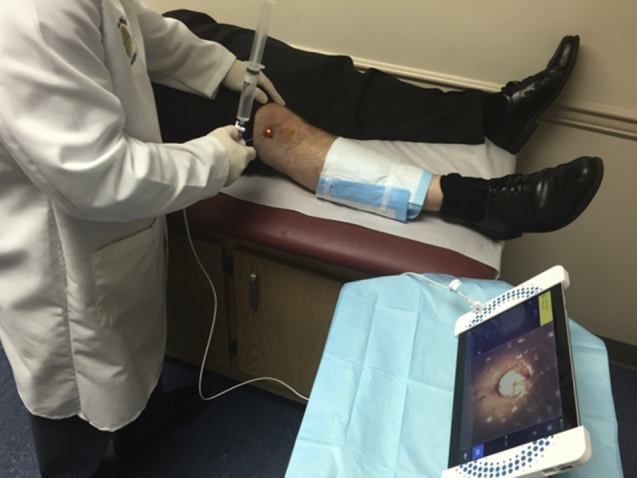
Patients who undergo the in-office procedure are provided informed consent for a diagnostic arthroscopy. Figure 1 depicts a typical room setup. Table 3 provides a preprocedure checklist to ensure all the necessary items are available at the bedside. A sterile field is created on a mayo stand and placed adjacent to the patient bed. The visualization tablet (Mi-Eye, Trice Medical, King of Prussia, PA) is placed at the far end of the mayo stand angled facing the physician. Below is a step-by-step breakdown of a knee in-office diagnostic arthroscopy (Video 1). Within this breakdown lie a few pearls that can help a physician navigate the procedure smoothly (Table 4).
-
1.
The patient is positioned laying supine with a gel bump under his or her affected knee, allowing for approximately 45° flexion. This can be removed if needed for patellofemoral evaluation if desired. Alternatively, the patient may be positioned lying supine or sitting up with the knee flexed to 90°, based on physician preference.
-
2.
A sterile dressing is applied distal to the knee to allow for manipulation throughout the procedure.
-
3.
The portal sites depicted in Figure 2 are sterilized with a betadine preparation stick. The preferred technique for the authors consists of identifying a medial and lateral infrapatellar portal 1 finger's breadth above the joint line. A standard superolateral portal can be prepped and used if needed. The device used for joint entry and viewing is a self-blunting needle arthroscope with a 0° viewing angle (Mi-Eye, Trice Medical).
-
4.
Portal location is just approximately 1 cm above the tibial joint line (typically at the level of the inferior pole of the patella) and 1 cm medial or lateral (depending on the portal being used) to the border of the patellar tendon.
-
5.
A 10-mL syringe of 1% lidocaine with a 22-gauge needle is used to create a skin wheel at the potential portal sites using 1 to 2 mL. The remaining lidocaine is then applied to the joint to allow for gentle distention and anesthesia. Before injecting the joint, the needle can be used to check the trajectory of the future needle arthroscope positioning.
-
6.
The authors recommend waiting 3 to 5 minutes to allow the anesthetic to take effect prior to joint entry with the needle arthroscope. During this time, a separate patient may be seen.
-
7.
In preparation for the procedure, the needle arthroscope is connected in a sterile manner to the viewing tablet, and a 30-mL syringe of sterile saline is connected to the inflow port on the arthroscope hand piece.
-
8.
The diagnostic procedure is begun with joint entry based on the pathology identified on the physical examination. Our preferred approach is to view for the pathology suspect on examination, followed by completing the remainder of the joint inspection. For the purpose of this paper, we will reference the medial infrapatellar entry site as the portal of initiation (Fig 3).
-
9.
When entering the joint from either portal, it is recommended to aim for the intracondylar notch to avoid iatrogenic cartilage injury.
-
10.
Upon entry into the joint through the anesthetized medial skin wheel, the needle sheath is retracted to allow for visualization by the scope. The retraction button is ergonomically placed on the superior portion of the handheld device (Fig 4). If tissue obscures visualization after retraction, a gentle flush can be performed using the 30-mL saline syringe through the inflow port. It is recommended to retract the optics when flushing to remove entrapped synovial tissue.
-
11.
The femoral and tibial cartilage is first evaluated. If a cartilage flap is suspected, an 18-gauge needle can be introduced from the lateral skin wheel for gentle palpation.
-
12.
Next, the needle arthroscope is directed toward the posterior horn of the medial meniscus, and is moved systematically toward the midbody and anterior horn (Fig 5). Tears and tissue quality can be noted. If an undersurface tear is suspected, a gentle flush can be performed with the saline syringe to flutter the meniscus superiorly and inferiorly.
-
13.
The medial gutter is then checked for loose bodies.
-
14.
The needle arthroscope is then withdrawn slightly and swung superiorly to evaluate the medial femoral condyle and trochlear cartilage. The lateral trochlea and femoral condyle are then inspected as well.
-
15.
As the needle arthroscope is brought down the lateral femoral condyle, the lateral gutter can be inspected, followed by entry into the lateral compartment.
-
16.
The lateral meniscus is evaluated again by starting at the root of the posterior horn and working around to the midbody and anterior horn (Fig 6).
-
17.
After the lateral meniscus is evaluated, the lateral femoral condyle cartilage can be evaluated. For a thorough examination, the knee can be ranged as needed to gain access to the deep portion of the condyle.
-
18.
Next the anterior cruciate ligament is inspected by directing the needle arthroscope into the intercondylar notch. To aid in evaluating the quality of the femoral attachment, the knee can be manipulated into a figure-4 position to apply tension to the ligament (Fig 7).
-
19.
Finally, the needle arthroscope can be placed into the patellofemoral compartment. This can be achieved through the original medial or lateral starting portal, or by accessing the compartment through the previously anesthetized superolateral portal. The authors recommend removing the bump from behind the knee and extending the leg to 0° (Fig 8).
-
20.
Once access has been obtained, the evaluation begins medially in the compartment to look for plica bands.
-
21.
The needle arthroscope is then moved toward the center of the compartment. This will allow for evaluation of the integrity of the cartilage and also to access the patellar congruency over the trochlea. The knee can be gently flexed to gain further understanding of the tracking.
-
22.
The superior recess of the knee joint can then be evaluated to ensure there are no signs of loose bodies.
-
23.
Once the diagnostic arthroscopy is complete, the authors recommend placing an empty 30-mL syringe into the inflow port and aspirating any residual saline that was placed into the joint.
-
24.
The needle arthroscope is then removed and a compressive dressing is applied for the evening.
-
25.
The patient may weight-bear as tolerated. Patients are instructed to ice the knee for 24 hours, and to take a nonsteroidal anti-inflammatory drug if permitted.
Fig 1.

In-office room setup. A sterile field is created near the ipsilateral (right) knee to allow for adequate visualization of tablet and portal sites. A gel/foam bump is placed under the knee to provide for approximately 30°-45° of flexion. The distal extremity is wrapped with a sterile dressing to allow for manipulation.
Table 3.
Preprocedure Checklist for Office-Based Needle Arthroscopy
| Necessary items to perform an office-based needle arthroscopy are listed below. It is imperative to maintain sterile technique through the entire procedure. Besides the viewing tablet, the instruments are for one-time use only and should be discarded appropriately after the procedure. |
Setup
|
Procedure
|
Postprocedure
|
Table 4.
Pearls for Performing Diagnostic Needle Arthroscopy of the Knee
| Similar to standard surgical arthroscopy, diagnostic needle arthroscopy requires many considerations prior to performing the procedure to obtain adequate visualization of intra-articular structures. The surgeon must have a standardized approach to minimize the risk of missed diagnoses. The following applies for either a right or left knee: |
| Flex the knee 45°-90° for medial and lateral compartment evaluations. Place the knee in extension for the patellofemoral joint. |
| Using a 10-mL syringe, inject a 1-2-mL skin wheel for each anticipated portal location, with care taken to also anesthetize the joint capsule. If desired, the surgeon can inject the remaining 1% lidocaine into the joint. Allow 3-5 minutes for it to take effect. |
| The height of the medial and lateral portals is approximately 1 cm superior to the anterior tibial slope, at the level of the inferior pole of the patella. The entry point, once this level has been established, is approximately 1 cm from the patellar tendon toward the “soft spot.” Varus or valgus forces can gently be placed on the leg to facilitate entry into the lateral and medial compartments, respectively. |
| If there is difficulty with visualization upon entry to the medial or lateral compartment, the authors recommend entry through a superior-lateral approach. After the patellofemoral joint is evaluated, a separate needle can be placed under direct visualization at the medial or lateral portal location to ensure an appropriate, synovial-free trajectory. |
| At the conclusion of the procedure, the authors recommend inserting an empty 30-mL syringe onto the inflow port, and aspirating any residual saline that was placed into the joint. |
Fig 2.

Standard portal sites (right knee). The medial (MED) and lateral (LAT) infrapatellar portal sites are identified approximately 1 cm above the tibial joint line and 1 cm medial or lateral to the border of the patellar tendon. The superolateral (SL) portal site is identified at the level of the superior aspect of the patella and 1 cm lateral to the lateral border of the patella. These sites are sterilized and anesthetized prior to needle arthroscope insertion.
Fig 3.

Medial knee compartment visualized (right knee). Needle arthroscope inserted 1 finger's breadth above the joint line, just medial to the patellar tendon using a medial infrapatellar portal. A 30-mL syringe is connected to the outflow port on the arthroscope handpiece. The arthroscope is connected to the tablet placed on the ipsilateral side to allow for adequate visualization while performing the procedure.
Fig 4.
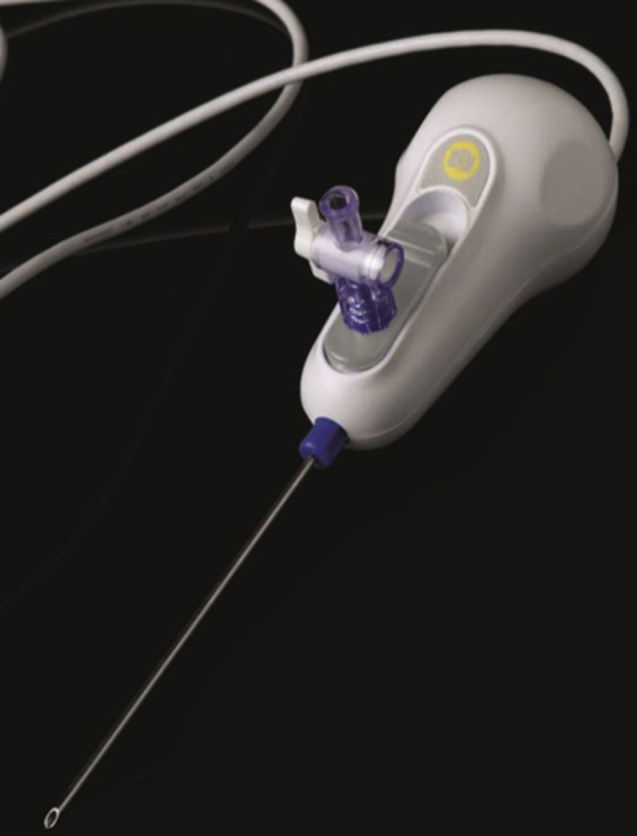
Needle arthroscope configuration (right knee). The needle sheath is retracted once the surgeon is within the joint by pushing back on the gray retraction button found on superior portion of the arthroscope hand piece. This exposes the camera (not seen in this figure) within the sheath to allow for full visualization of intra-articular anatomy.
Fig 5.
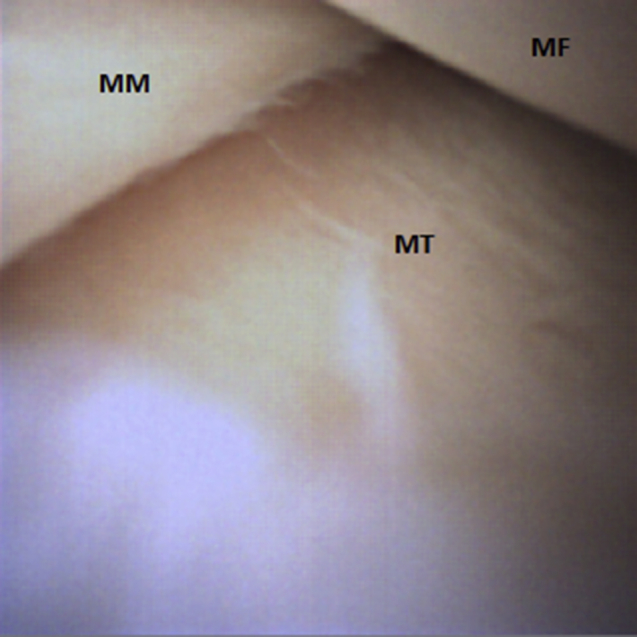
Medial meniscus (right knee). The needle arthroscope is introduced through the medial infrapatellar portal and pointed toward the notch. Once acceess has been obtained, the device is directed into the medial compartment. The surgeon can then systematically follow the medial meniscus to the midbody (MM) and then anterior horn. The medial femoral (MF) and tibial (MT) cartilage can be assessed through this portal as well.
Fig 6.
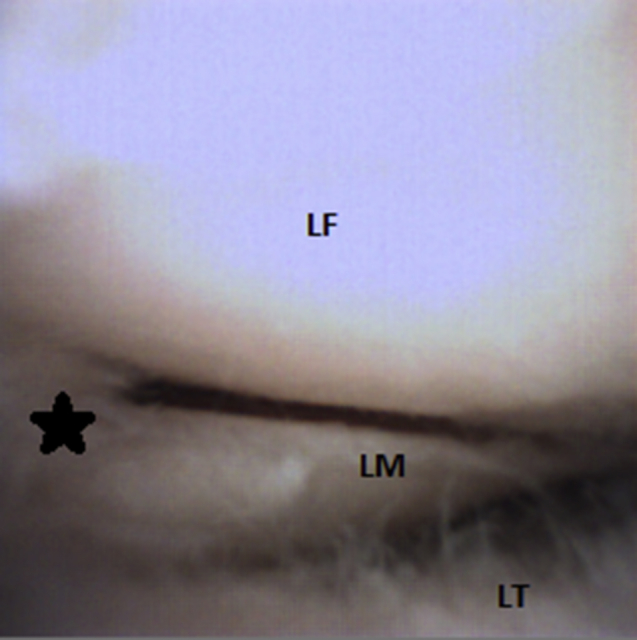
Lateral meniscus (right knee). Using the medial infrapatellar portal, the lateral compartment is entered. The lateral meniscus (LM) is evaluated in a posterior-to-superior direction. Here a tear of the posterior horn of the lateral meniscus (star) is visualized. Inspection of the lateral femoral (LF) and tibial (LT) cartilage should be performed. If there is diffculty with visualization, the lateral infrapatellar portal may be used to complete the full assessment of the lateral compartment.
Fig 7.
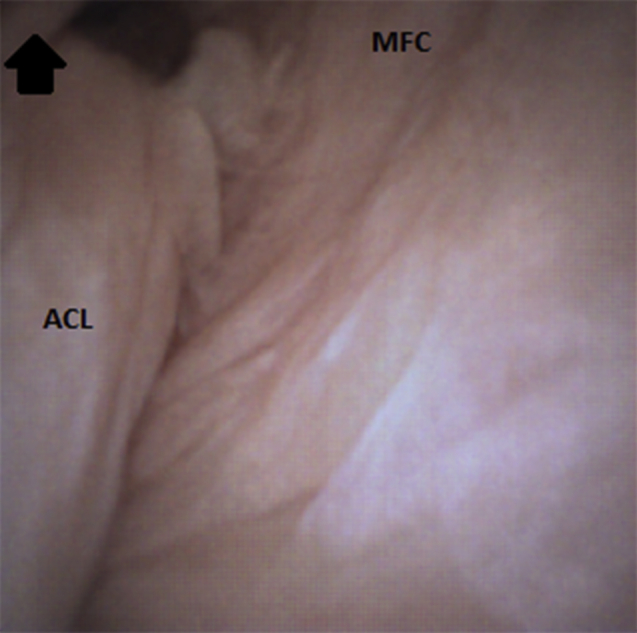
Anterior cruciate ligament (ACL) (right knee). The ACL and the intercondylar notch is visualized from the medial infrapatellar portal. The surgeon should thoroughly assess the ACL, inspecting both the tibial and femoral insertions. The knee may be brought in to a figure-4 position to tension the ligament and aid in visualizing the attachment to the medial aspect of the lateral femoral condyle (arrow). The lateral aspect of the medial femoral condyle (MFC) is labeled here for reference.
Fig 8.
Positioning for access to patellofemoral joint (right knee). The patellofemoral joint can be accessed and inspected through the superolateral portal. The bump is removed from behind the knee prior to gaining access, allowing for full extension. The arthroscope should be advanced to the medial aspect of the patellofemoral joint. As the surgeon slowly withdraws the arthroscope, evaluation of cartilage integrity and patellofemoral tracking should be performed.
Discussion
Office-based needle arthroscopy provides instant access to injury assessment and allows physicians to develop a plan of care more efficiently. This modality eliminates unnecessary outpatient diagnostic arthroscopy procedures because of an equivocal examination or imaging findings. This not only lessens wasted health care dollars, but also limits possible complications secondary to surgical arthroscopy. Szachnowski et al. demonstrated major and minor complication rates of 1.2% and 12.8%, respectively, in 335 rheumatoid patients who underwent office-based knee arthroscopies.6 Baeten et al. later reported no major complications and minor complications in less than 10% of patients who received needle arthroscopy for knee synovitis.7 These studies suggest that office-based needle arthroscopy has a safety profile that compares favorably with standard arthroscopy. Larger studies further examining the safety profile of needle arthroscopy in the general population should be an area of future research as this technology continues to develop. Additional benefit lies in the form of time-savings for the patient. A review of the average time saved by using an in-office diagnostic arthroscope versus MRI was approximately 2 weeks.8 Lastly, the ability to perform a dynamic examination of the knee under direct visualization will minimize missed chondral flaps injuries, and will better distinguish a new injury versus sequela from a previous arthroscopy. It can further allow for a better understanding of healing through a second look evaluation for patients who have undergone a cartilage procedure.
Limitations of needle arthroscopy still remain, however. Unlike standard arthroscopy, fluid is not continuously irrigated through the joint. This may hinder visualization in patients with significant hemarthrosis or severe synovitis, allowing small meniscal tears to be missed. By forgoing an MRI, evaluation of the subchondral bone is negated. This can potentially have ramifications if a subchondral insufficiency fracture or avascular necrosis is suspected. Furthermore, incorporation of a bone plug cannot be fully evaluated without the use of an MRI.
In summary, office-based needle arthroscopy offers a safe, accurate, and cost-effective means to evaluate intra-articular knee anatomy. Using a standardized approach optimizes the application of this technology and can provide a real-time diagnosis of pathology for both the treating physician and the patient. Through a series of standardized steps, the physician can quickly and safely perform the procedure without disruption to the standard office work flow.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.M. is a paid consultant for Trice Medical in the form of teaching and receives consultancy fees from Mitek, Zimmer, Rotation Medical, Arthrex, Trice Medical, and Exatech.
Supplementary Data
Demonstration of in-office diagnostic needle arthroscopy. In this video, superolateral, inferomedial, and inferolateral portals are used to perform a standard diagnostic knee arthroscopy of the right knee. Full visualization of intra-articular anatomy in the suprapatellar pouch, patellofemoral articulation, and medial and lateral compartments is achieved.
References
- 1.Kim S., Bosque J., Meehan J.P., Jamali A., Marder R. Increase in outpatient knee arthroscopy in the United States: A comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 2.Cullen K.A., Hall M.J., Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;11:1–25. [PubMed] [Google Scholar]
- 3.Crawford R., Walley G., Bridgman S., Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: A systematic review. Br Med Bull. 2007;84:5–23. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 4.Voigt J.D., Mosier M., Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: A cost analysis. Appl Health Econ Health Policy. 2014;12:523–535. doi: 10.1007/s40258-014-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gramas D.A., Antounian F.S., Peterfy C.G., Genant H.K., Lane N.E. Assessment of needle arthroscopy, standard arthroscopy, physical examination, and magnetic resonance imaging in knee pain: A pilot study. J Clin Rheumatol. 1995;1:26–34. doi: 10.1097/00124743-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Szachnowski P., Wei N., Arnold W.J., Cohen L.M. Complications of office based arthroscopy of the knee. J Rheumatol. 1995;22:1722–1725. [PubMed] [Google Scholar]
- 7.Baeten D., Van den bosch F., Elewaut D., Stuer A., Veys E.M., De keyser F. Needle arthroscopy of the knee with synovial biopsy sampling: Technical experience in 150 patients. Clin Rheumatol. 1999;18:434–441. doi: 10.1007/s100670050134. [DOI] [PubMed] [Google Scholar]
- 8.O'Donnell J. Trice Medical Literature. #4-10-0032 Rev A.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demonstration of in-office diagnostic needle arthroscopy. In this video, superolateral, inferomedial, and inferolateral portals are used to perform a standard diagnostic knee arthroscopy of the right knee. Full visualization of intra-articular anatomy in the suprapatellar pouch, patellofemoral articulation, and medial and lateral compartments is achieved.


