Abstract
Background:
The rate of cesarean delivery is increasing in North America. Surgical site infection following this operation can make it difficult to recover, care for a baby and return home. We aimed to determine the incidence of surgical site infection to 30 days following cesarean delivery, associated risk factors and whether risk factors differed for predischarge versus postdischarge infection.
Methods:
We identified a retrospective cohort in Nova Scotia by linking the provincial perinatal database to hospital admissions and physician billings databases to follow women for 30 days after they had given birth by cesarean delivery between Jan. 1, 1997 and Dec. 31, 2012. Logistic regression with generalized estimating equations was used to determine risk factors for infection.
Results:
A total of 25 123 women had 33 991 cesarean deliveries over the study period. Of the 25 123, 923 had surgical site infections, giving an incidence rate of 2.7% (95% CI 2.54%-2.89%); the incidence decreased over time. Risk factors for infection (adjusted odds ratios ≥ 1.5) were prepregnancy weight 87.0 kg or more, gaining 30.0 kg or more during pregnancy, chorioamnionitis, maternal blood transfusion, anticoagulation therapy, alcohol or drug abuse, second stage of labour before surgery, delivery in 1997-2000 and delivery in a hospital performing 130-1249 cesarean deliveries annually. Women who gave birth earlier in the study period, those who gave birth in a hospital with 130-949 cesarean deliveries per year and those with more than 1 fetus were at a significantly higher risk for surgical site infection before discharge; women who smoked were at significantly higher risk for surgical site infection after discharge.
Interpretation:
Most risk factors are known before delivery, and some are potentially modifiable. Although the incidence of surgical site infection decreased over time, targeted clinical and infection prevention and control interventions could further reduce the burden of illness associated with this health-care-related infection.
The proportion of infants born by cesarean delivery has been increasing in North America. In Canada, the cesarean delivery rate was 20% in 19881 and rose to 26% in 2012.2 Surgical site infection following this procedure can adversely influence the postpartum period for the women and her newborn, making it difficult to recover, care for a baby and return home. Although Canada has no national surveillance for surgical site infection following cesarean delivery, the US National Healthcare Safety Network follows this infection and reported a mean rate of 0.16% in 2014.3 An Australian study of 81 health care facilities from 2002 to 2013 showed a rate of 2.05%, which decreased over the study period.4 Some hospitals conduct surveillance on these infections up until discharge, and others also conduct postdischarge surveillance. The rate of surgical site infection until hospital discharge following cesarean delivery varies, with reported values ranging from 0.16% to 3.2%.3,5,6 Although rates are higher if postdischarge surveillance is conducted, this activity is resource intensive and therefore is not routinely performed.
Risk factors for surgical site infection following cesarean delivery have been identified in the literature. Most studies have shown a significant association between obesity and risk for surgical site infection,7,8 and a dose-response relation between body mass index and risk for infection has been noted.5 Findings for other risk factors, such as hypertension and diabetes, have been less consistent.5,9,10 Both appropriately timed antibiotic prophylaxis11 and chlorhexidine antiseptic skin preparation12 have been shown to decrease the infection risk. Few studies report infection rates to 30 days post partum. There is little or no evidence regarding whether risk factors differ based on time of infection presentation, and the influence of hospital size, anticoagulation therapy and smoking on infection risk.
In this retrospective population-based cohort study, we followed women from the perinatal period to 30 days post partum to determine 1) the incidence of surgical site infection including before and after hospital discharge, 2) risk factors associated with infection and 3) whether risk factors differed with time of presentation of infection.
Methods
Setting
This study took place in Nova Scotia (population roughly 950 000), which in 2011 had 8860 births and a cesarean delivery rate of 26.6%.13 About half of deliveries are performed at the regional and tertiary care centre, IWK Health Centre, based in the capital city (Halifax).
Participants
Women with a Nova Scotia health card who gave birth via cesarean delivery in the province between Jan. 1, 1997 and Dec. 31, 2012 were eligible. Before 1997, International Classification of Diseases, 9th revision (ICD-9) codes were not captured with decimals in the physician billings database and, therefore, could not be used to distinguish surgical site infections from other types of infection. When this study was begun, administrative health databases were complete up until 2012. In Nova Scotia, everyone is eligible for a health card if they can provide proof of citizenship or immigration. Women were excluded if they delivered a baby weighing less than 500 g or at less than 20 weeks' gestational age.
Design and data sources
We identified the retrospective cohort using the Nova Scotia Atlee Perinatal Database (NSAPD), administered by the Reproductive Care Program of Nova Scotia. It contains information on all pregnancies and deliveries in the province, which is collected by health care professionals using standardized forms and patient charts. The database is regularly analyzed for accuracy and reliability. From the database, we obtained relevant information on pregnancy, labour, delivery and the postpartum period, including surgical site infection identified before discharge.
Outcome
The outcome was surgical site infection following cesarean delivery within 30 days of surgery. The NSAPD was linked with the Canadian Institute for Health Information's Discharge Abstract Database (to capture the delivery admission or readmission) and with the Nova Scotia Medical Services Insurance Physician Billings Database (to capture insured service encounters rendered by a physician) to identify women with a diagnostic code indicative of surgical site infection. The Discharge Abstract Database used the ICD-9 until 2000 and the Canadian enhancement of the 10th revision (ICD-10-CA) from 2001 onward; the Physicians Billings Database used ICD-9 codes. Diagnostic codes indicative of surgical site infection were those for wound infection or endometritis according to any of the coding systems: the NSAPD, ICD-9 (614.3, 674.30, 674.32, 674.34, 998.51, 998.59) or ICD-10-CA (N71.0, N71.9, N73.0, O86.0xx). We categorized infections according to whether the infection was diagnosed during the hospital stay for delivery of the infant or after discharge. The timing of predischarge surgical site infections could not be defined as only admission and discharge dates are recorded in the Discharge Abstract Database. For infections identified after discharge, we estimated the number of days from surgery to infection identification based on the date of either hospital readmission or physician encounter.
Potential risk factors
We examined several potential risk factors for surgical site infection based on a literature review and the variables available in the NSAPD (Table 1). This database has information on smoking at various times (i.e., at first prenatal visit, 20 weeks' gestation and delivery), from which we determined whether the woman smoked. Height was not recorded in the NSAPD until 2003; therefore, we approximated standard body mass index categories14 using weight cut-points determined by means of receiver operator characteristic curve analysis: less than 53.0 kg = underweight, 53.0-66.9 kg = normal, 67.0-76.9 kg = overweight, 77.0-86.9 kg = obese I, 87.0-97.9 kg= obese II and 98.0 kg or more = obese III. In supplementary analyses of deliveries from 2003 on, we examined body mass index (< 18.5 kg/m2, 18.5-24.9 kg/m2, 25.0-29.9 kg/m2, 30.0-39.9 kg/m2 and ≥ 40.0 kg/m2) for comparison. Hypertension, diabetes and depression variables were all combinations of both diagnostic codes and codes indicating that the woman was taking medication for these medical conditions from the NSAPD.
Table 1: Potential risk factors for surgical site infection that were examined, to determine inclusion in multivariable model in univariate analyses.
| Category | Factors not associated with infection (p ≥ 0.10) | Factors associated with infection (p < 0.10) |
|---|---|---|
| Institution-related | - | No. of cesarean deliveries in delivery hospital (< 130, 130-949, 950-1249, ≥ 1250) |
| Area-level | Maternal residence (urban, rural) | Region of maternal residence (A, B, C, D) Neighbourhood-level income quintile (1, 2, ≥ 3) |
| Maternal demographic characteristics | - | Maternal age (< 25 yr, 25-34 yr, ≥ 35 yr) Prepregnancy weight (< 53.0 kg, 53.0-66.9 kg, 67.0-76.9 kg, 77.0-86.9 kg, 87.0-97.9 kg, ≥ 98.0 kg, missing) Marital status (married or common-law, other, missing) Smoking during pregnancy (no, yes) Alcohol or drug abuse during pregnancy (no, yes) |
| Maternal medical conditions | Maternal influenza immunization in pregnancy (no, yes) | Nonobstetric preexisting health condition affecting pregnancy (no, yes) Hypertension (no, preexisting, gestational or unspecified, preeclampsia) Diabetes (no, preexisting, gestational) Anemia during pregnancy (no, yes) Depression (no, yes) Anticoagulation therapy during pregnancy (no, yes) |
| Pregnancy history | Surgical site infection after previous cesarean delivery (no, yes) | Parity (primiparous, multiparous) Mode of delivery in last pregnancy (none, vaginal, cesarean Previous cesarean delivery (0, 1, ≥ 2) |
| Pregnancy characteristics | - | Weight gain during pregnancy (< 10.0 kg, 10.0-19.9 kg, 20.0-29.9 kg, ≥ 30.0 kg, missing) Chorioamnionitis (no, yes) Diagnostic and/or therapeutic procedure(s) performed in woman (no, yes) Steroid use ≥ 48 h before delivery for fetal lung maturity (no, yes) |
| Labour | Cervical dilation at last examination before cesarean delivery (0 cm, 1-3 cm, 4-10 cm) Time between rupture of membranes to delivery (≤ 1 h, 2-11 h, ≥ 12 h) Stage of labour before cesarean delivery (none, first, second) Spontaneous rupture of membranes (yes, no) |
|
| Delivery | Season of delivery (December-February, March-May, June-August, October-November) Type of cesarean delivery (low segment transverse, other) Instrumentation use (no, forceps/vacuum) General anesthesia during labour and/or delivery (no, yes) Other procedure(s) performed during cesarean delivery (no, yes) |
Length of antepartum stay (< 24 h, 24-49 h, ≥ 50 h) Year of delivery (1997-2000, 2001-2004, 2005-2008, 2009-2012) Delivery on weekend (no, yes) Primary indication for cesarean delivery (breech presentation, dystocia, fetal distress, other, previous cesarean delivery) Regional anesthesia during labour and/or delivery (no, yes) Antibiotic therapy during labour and delivery (yes, no) Maternal blood transfusion (no, yes) |
| Fetal and neonatal | Presentation at delivery (vertex, other, missing) No. of fetuses (1, ≥ 2) Diagnostic and/or therapeutic procedure(s) performed in fetus (no, yes) |
Infant birth weight (< 2500 g, 2500-3999 g, ≥ 4000 g) Apgar score at 5 min (< 7, ≥ 7) Gestational age (< 37 wk, 37 wk to 39 wk + 6 d, ≥ 40 wk) Breastfeeding at discharge (yes, no) |
Statistical analysis
The unit of analysis was cesarean delivery rather than women. We used descriptive statistics to estimate the incidence of predischarge, postdischarge and total surgical site infection to 30 days with exact confidence intervals (CIs). We used χ2 tests to determine which risk factors were significantly associated with surgical site infection. We entered risk factors associated with infection at p < 0.10 into a multiple logistic regression model, from which we removed risk factors that were not independently associated with surgical site infection using backward stepwise selection. Only risk factors that were associated with infection at p < 0.05 were retained. From the logistic models, we estimated adjusted odds ratios (ORs) with 95% CIs. We examined risk factors for pre- and postdischarge surgical site infection using multinomial logistic regression. Generalized estimating equations were used for all logistic models to account for potential correlation between women who had more than 1 cesarean delivery over the study period. If 5% or more of data was missing for a risk factor, we created a "missing" category. Because a missing-value category would have low numbers for risk factors with less than 5% of data missing, we excluded deliveries with missing values for these risk factors from regression analyses. We did not use multiple imputation for our primary analyses owing to the large size of our data set. Estimates from analyses using 5 data sets with missing values imputed with chained equations were very similar to those shown herein. We conducted all analyses using Stata/SE 13 (StataCorp LP).
Ethics approval
This study was approved by the Reproductive Care Program of Nova Scotia's Joint Data Access Committee, Health Data Nova Scotia and the IWK Health Centre's Research Ethics Board.
Results
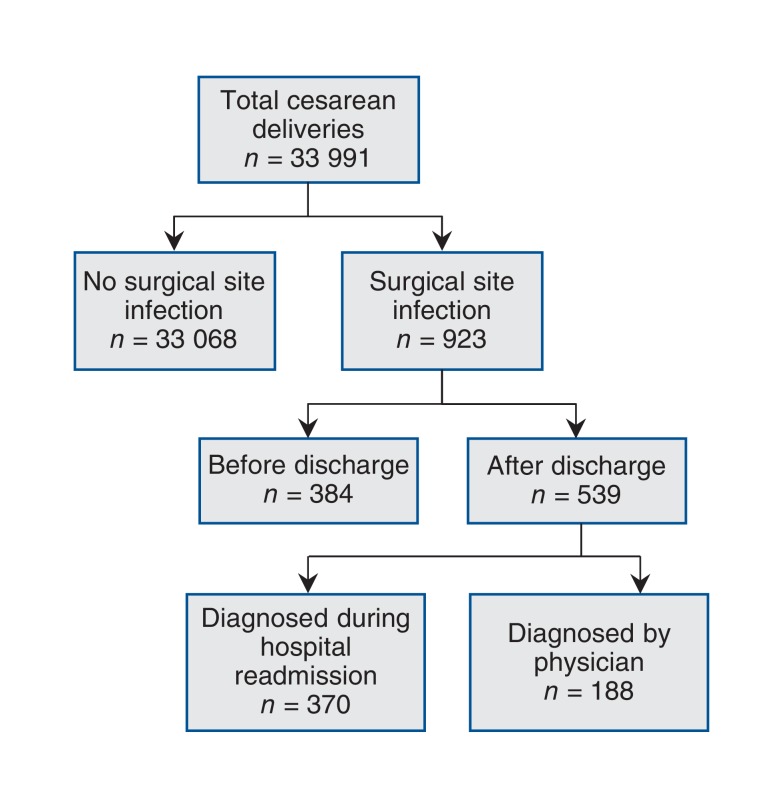
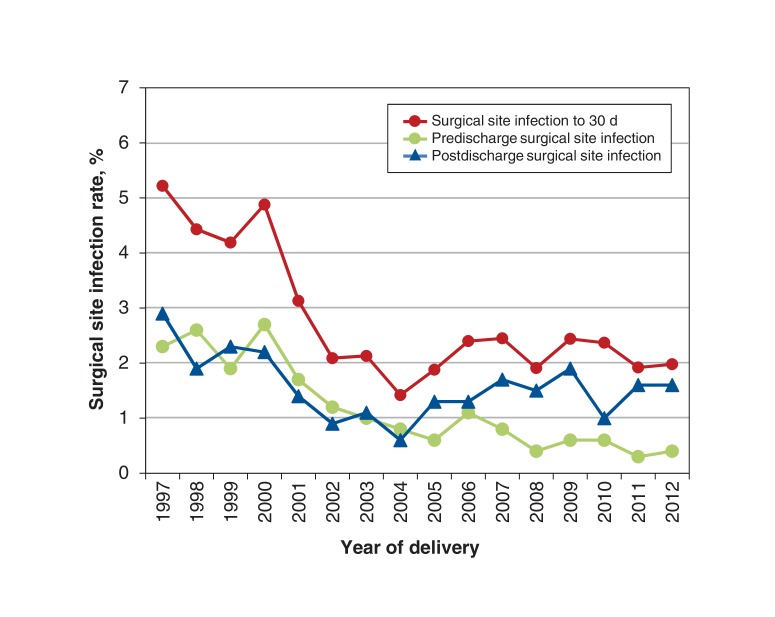
During the period 1997-2012, 25 123 women (with 33 991 cesarean deliveries) were identified from the NSAPD and could be linked to hospital and physician billings data (> 96% linkage). A total of 923 surgical site infections followed the 33 991 deliveries within 30 days, giving an incidence rate of 2.7% (95% CI 2.54%-2.89%) (Figure 1). Fifteen women had more than 1 surgical site infection during the study period. The incidence of surgical site infections decreased from 5.2% in 1997 to 2.0% in 2012 (Figure 2). The incidence of infection was higher after discharge (1.6% [95% CI 1.45%-1.72%]) than before discharge (1.1% [95% CI 1.02%-1.24%]) (p < 0.001). Of the 539 postdischarge surgical site infections, 370 (68.6%) were identified during hospital readmission. Of the 539 women who presented with surgical site infection after discharge, 469 (87.0%) did so within 2 weeks of their surgery. The mean length of postpartum stay decreased from 3.86 (standard deviation 1.53) days in 1997-2000 to 3.23 (standard deviation 1.04) days in 2009-2012 (p < 0.001). The rate of administration of antibiotic therapy for prophylaxis or treatment during labour and delivery increased from 46.9% in 1997-2000 to 73.6% in 2009-2012; we were unable to distinguish between these indications from the data available. We were able to determine that, from 2003 to 2012, the indication was group B Streptococcus infection in 972 (8.2%)of the 11 854 women who received antibiotics.
Figure 1.
Participant flow diagram. "Diagnosed during hospital readmission" and "diagnosed by physician" do not add to 539 as 19 women were coded as having a surgical site infection during a hospital readmission and a physician office visit.
Figure 2.
Rate of surgical site infection by year.
Table 2 shows the risk factors independently associated with the odds of developing surgical site infection within 30 days following cesarean delivery at p < 0.05 (see Appendix 1, available at www.cmajopen.ca/content/5/3/E546/suppl/DC1, for univariate analysis). Women who gave birth in 1997-2000 had a higher risk of infection (adjusted OR 2.31, 95% CI 1.88-2.84) than those who gave birth in 2009-2012. Compared to women who were primiparous, those who were multiparous had a lower risk of surgical site infection (adjusted OR 0.81, 95% CI 0.69-0.95). A dose-response relation was observed between prepregnancy weight and infection, with women who weighed 98.0 kg or more having more than 3 times the odds of infection as women who weighed 53.0-66.9 kg. In supplementary analyses conducted for 2003-2012, body mass index was similarly positively associated with infection (data not shown).
Table 2: Risk factors for surgical site infection following cesarean delivery to 30 days post partum.
| Risk factor | % of total* | No. of deliveries | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| No infection | Infection | |||
| Institution-related | ||||
| No. of cesarean deliveries per hospital per year | ||||
| < 130 | 25.1 | 8165 | 158 | Reference |
| 130-949 | 21.7 | 6910 | 282 | 2.20 (1.79-2.71) |
| 950-1249 | 27.7 | 8861 | 317 | 1.85 (1.50-2.29) |
| ≥ 1250 | 25.5 | 8305 | 154 | 1.39 (1.09-1.79) |
| Area-level | ||||
| Quintile of neighbourhood-level income | ||||
| 1 (lowest) | 20.1 | 6410 | 262 | 1.40 (1.19-1.65) |
| 2 | 18.1 | 5824 | 172 | 1.09 (0.91-1.30) |
| 3-5 | 61.8 | 20 007 | 477 | Reference |
| Maternal demographic characteristics | ||||
| Age, yr | ||||
| < 25 | 18.6 | 5929 | 225 | 1.13 (0.94-1.36) |
| 25-34 | 61.5 | 19 880 | 511 | Reference |
| ≥ 35 | 19.9 | 6432 | 175 | 1.21 (1.01-1.45) |
| Prepregnancy weight, kg | ||||
| < 53.0 | 8.0 | 2603 | 61 | 1.05 (0.78-1.41) |
| 53.0-66.9 | 29.3 | 9519 | 194 | Reference |
| 67.0-76.9 | 16.8 | 5429 | 135 | 1.28 (1.02-1.61) |
| 77.0-86.9 | 12.1 | 3888 | 108 | 1.43 (1.12-1.82) |
| 87.0- 97.9 | 7.8 | 2488 | 85 | 1.86 (1.42-2.43) |
| ≥ 98.0 | 9.5 | 2961 | 186 | 3.63 (2.90-4.54) |
| Missing | 16.6 | 5353 | 142 | 1.52 (1.12-2.06) |
| Marital status | ||||
| Married/common-law | 72.7 | 23 511 | 578 | Reference |
| Single/divorced/separated/widowed | 22.3 | 7116 | 285 | 1.34 (1.13-1.58) |
| Missing | 5.0 | 1614 | 48 | 1.14 (0.83-1.58) |
| Alcohol or drug abuse | ||||
| No | 98.6 | 31 809 | 885 | Reference |
| Yes | 1.4 | 432 | 26 | 1.71 (1.12-2.61) |
| Maternal medical conditions | ||||
| Nonobstetric preexisting health conditions affecting pregnancy | ||||
| No | 80.9 | 26 160 | 676 | Reference |
| Yes | 19.1 | 6081 | 235 | 1.28 (1.09-1.51) |
| Diabetes | ||||
| No | 93.5 | 30 181 | 809 | Reference |
| Preexisting | 0.6 | 196 | 11 | 1.62 (0.86-3.04) |
| Gestational | 5.9 | 1864 | 91 | 1.49 (1.17-1.88) |
| Depression during pregnancy | ||||
| No | 95.6 | 30 826 | 855 | Reference |
| Yes | 4.4 | 1415 | 56 | 1.40 (1.05-1.87) |
| Anticoagulation therapy during pregnancy | ||||
| No | 99.1 | 31 965 | 888 | Reference |
| Yes | 0.9 | 276 | 23 | 2.58 (1.64-4.05) |
| Pregnancy history | ||||
| Parity | ||||
| Primiparous | 49.4 | 15 837 | 539 | Reference |
| Multiparous | 50.6 | 16 404 | 372 | 0.81 (0.69-0.95) |
| Pregnancy characteristics | ||||
| Weight gain during pregnancy, kg | ||||
| < 10.0 | 16.7 | 5372 | 155 | 0.81 (0.66-0.99) |
| 10.0-19.9 | 41.8 | 13 522 | 350 | Reference |
| 20.0-29.9 | 13.6 | 4352 | 142 | 1.26 (1.03-1.54) |
| ≥ 30.0 | 1.9 | 601 | 37 | 2.14 (1.49-3.06) |
| Missing | 26.0 | 8394 | 227 | 1.10 (0.86-1.41) |
| Chorioamnionitis | ||||
| No | 97.8 | 31 569 | 856 | Reference |
| Yes | 2.2 | 672 | 55 | 2.78 (2.07-3.75) |
| Labour | ||||
| Stage of labour before cesarean delivery | ||||
| None | 48.6 | 15 793 | 332 | Reference |
| First | 31.9 | 10 235 | 350 | 1.20 (1.01-1.43) |
| Second | 19.4 | 6213 | 229 | 1.54 (1.27-1.88) |
| Delivery | ||||
| Year of delivery | ||||
| 1997-2000 | 22.0 | 6947 | 342 | 2.31 (1.88-2.84) |
| 2001-2004 | 26.5 | 8607 | 191 | 1.14 (0.91-1.41) |
| 2005-2008 | 27.0 | 8742 | 193 | 1.02 (0.83-1.25) |
| 2009-2012 | 24.5 | 7945 | 185 | Reference |
| Antibiotic therapy during labour and delivery | ||||
| Yes | 62.9 | 20 355 | 506 | Reference |
| No | 37.1 | 11 886 | 405 | 1.30 (1.12-1.51) |
| Maternal blood transfusion | ||||
| No | 99.0 | 31 932 | 885 | Reference |
| Yes | 1.0 | 309 | 26 | 2.70 (1.77-4.12) |
| Fetal and neonatal | ||||
| Gestational age | ||||
| < 37 wk | 9.8 | 3125 | 120 | 1.36 (1.10-1.69) |
| 37 wk to 39 wk + 6 d | 57.1 | 18 475 | 443 | Reference |
| ≥ 40 wk | 33.1 | 10 641 | 348 | 1.09 (0.93-1.28) |
Note: CI = confidence interval, OR = odds ratio.
*A total of 33 152 cesarean deliveries were included in the analysis; 839 deliveries were excluded because of missing values for neighbourhood-level income (n = 724), stage of labour (n = 1) and/or gestational age (n = 118).
The results of the multinomial logistic regression analysis comparing the risk factors for pre- and postdischarge infection are given in Table 3 (see Appendix 2, available at www.cmajopen.ca/content/5/3/E546/suppl/DC1, for univariate associations). Women who smoked during pregnancy had significantly higher odds of infection presenting after discharge (adjusted OR 1.39, 95% CI 1.13-1.70) than before discharge (adjusted OR 0.94, 95% CI 0.73-1.21). Deliveries earlier in the study period, of more than 1 fetus and in a hospital performing 130-949 cesarean deliveries annually had significantly higher odds of surgical site infection presenting before discharge than after discharge.
Table 3: Risk factors for surgical site infection before and after discharge following cesarean delivery.
| Risk factor | No infection, no. of deliveries* | Infection before discharge | Infection after discharge | ||
|---|---|---|---|---|---|
| No. of deliveries* | Adjusted OR (95% CI) |
No. of deliveries* | Adjusted OR (95% CI) |
||
| Institution-related | |||||
| No. of cesarean deliveries per hospital per year | |||||
| < 130 | 8070 | 51 | Reference | 104 | Reference |
| 130-949 | 6893 | 125 | 3.16 (2.26-4.44) | 157 | 1.76 (1.34-2.30)† |
| 950-1249 | 8787 | 142 | 2.46 (1.73-3.51) | 170 | 1.58 (1.20-2.08) |
| ≥ 1250 | 8223 | 59 | 1.76 (1.16-2.67) | 95 | 1.26 (0.92-1.73) |
| Area-level | |||||
| Quintile of neighbourhood-level income | |||||
| 1 (lowest) | 6349 | 97 | 1.22 (0.95-1.57) | 162 | 1.54 (1.25-1.90) |
| 2 | 5784 | 70 | 1.03 (0.78-1.36) | 102 | 1.15 (0.91-1.46) |
| 3-5 | 19 840 | 210 | Reference | 262 | Reference |
| Maternal demographic characteristics | |||||
| Age, yr | |||||
| < 25 | 5876 | 82 | 1.08 (0.81-1.43) | 142 | 1.18 (0.93-1.49) |
| 25-34 | 19 719 | 211 | Reference | 295 | Reference |
| ≥ 35 | 6378 | 84 | 1.41 (1.08-1.83) | 89 | 1.08 (0.84-1.38) |
| Prepregnancy weight, kg | |||||
| < 53.0 | 2593 | 27 | 1.04 (0.67-1.60) | 34 | 1.08 (0.72-1.60) |
| 53.0-66.9 | 9463 | 92 | Reference | 102 | Reference |
| 67.0-76.9 | 5410 | 51 | 1.02 (0.72-1.45) | 82 | 1.46 (1.09-1.97) |
| 77.0-86.9 | 3868 | 46 | 1.29 (0.90-1.85) | 62 | 1.53 (1.11-2.12) |
| 87.0-97.9 | 2480 | 37 | 1.70 (1.15-2.51) | 48 | 1.97 (1.38-2.81) |
| ≥ 98.0 | 2954 | 71 | 3.07 (2.21-4.25) | 114 | 4.06 (3.02-5.45) |
| Missing | 5205 | 53 | 1.06 (0.68-1.67) | 84 | 1.95 (1.28-2.97) |
| Marital status | 3868 | ||||
| Married/common-law | 23 323 | 250 | Reference | 323 | Reference |
| Single/divorced/separated/widowed | 7044 | 111 | 1.34 (1.03-1.75) | 172 | 1.28 (1.03-1.58) |
| Missing | 1606 | 16 | 1.26 (0.73-2.18) | 32 | 1.07 (0.72-1.60) |
| Smoking during pregnancy | |||||
| No | 25 151 | 282 | Reference | 361 | Reference |
| Yes | 6822 | 95 | 0.94 (0.73-1.21) | 165 | 1.39 (1.13-1.70)† |
| Maternal medical conditions | |||||
| Nonobstetric preexisting health conditions affecting pregnancy | |||||
| No | 25 941 | 278 | Reference | 393 | Reference |
| Yes | 6032 | 99 | 1.37 (1.08-1.75) | 133 | 1.22 (0.99-1.50) |
| Diabetes | |||||
| No | 29 923 | 335 | Reference | 467 | Reference |
| Preexisting | 194 | 6 | 2.29 (0.96-5.48) | 5 | 1.28 (0.52-3.16) |
| Gestational | 1856 | 36 | 1.50 (1.05-2.15) | 54 | 1.47 (1.09-1.98) |
| Depression during pregnancy | |||||
| No | 30 567 | 357 | Reference | 490 | Reference |
| Yes | 1406 | 20 | 1.44 (0.91-2.29) | 36 | 1.45 (1.01-2.08) |
| Anticoagulation therapy during pregnancy | |||||
| No | 31 700 | 365 | Reference | 515 | Reference |
| Yes | 273 | 12 | 3.94 (2.02-7.70) | 11 | 1.93 (1.03-3.63) |
| Pregnancy history | |||||
| Parity | |||||
| Primiparous | 15 723 | 208 | Reference | 329 | Reference |
| Multiparous | 16 250 | 169 | 0.87 (0.69-1.08) | 197 | 0.75 (0.61-0.93) |
| Pregnancy characteristics | |||||
| Weight gain during pregnancy, kg | |||||
| < 10.0 | 5353 | 62 | 0.83 (0.61-1.12) | 93 | 0.80 (0.62-1.05) |
| 10.0-19.9 | 13 468 | 140 | Reference | 208 | Reference |
| 20.0-29.9 | 4341 | 61 | 1.40 (1.02-1.90) | 80 | 1.14 (0.87-1.48) |
| ≥ 30.0 | 599 | 18 | 2.98 (1.79-4.96) | 19 | 1.68 (1.02-2.75) |
| Missing | 8212 | 96 | 1.43 (1.01-2.02) | 126 | 0.92 (0.65-1.29) |
| Chorioamnionitis | |||||
| No | 31 307 | 352 | Reference | 496 | Reference |
| Yes | 666 | 25 | 3.30 (2.11-5.16) | 30 | 2.47 (1.67-3.63) |
| Diagnostic and/or therapeutic procedure(s) performed in woman | |||||
| No | 31 049 | 365 | Reference | 500 | Reference |
| Yes | 924 | 12 | 0.88 (0.49-1.57) | 26 | 1.52 (1.01-2.29) |
| Labour | |||||
| Stage of labour before cesarean delivery | |||||
| None | 15 645 | 155 | Reference | 172 | Reference |
| First | 10 159 | 132 | 1.00 (0.77-1.29) | 217 | 1.40 (1.11-1.77) |
| Second | 6169 | 90 | 1.35 (1.02-1.79) | 137 | 1.66 (1.28-2.15) |
| Delivery | |||||
| Year of delivery | |||||
| 1997-2000 | 6891 | 172 | 5.69 (4.01-8.07) | 163 | 1.30 (1.01-1.68)† |
| 2001-2004 | 8532 | 102 | 2.91 (2.00-4.25) | 88 | 0.63 (0.48-0.84)† |
| 2005-2008 | 8670 | 63 | 1.52 (1.03-2.25) | 130 | 0.88 (0.69-1.12)† |
| 2009-2012 | 7880 | 40 | Reference | 145 | Reference |
| Antibiotic therapy during labour and delivery | |||||
| Yes | 20 185 | 187 | Reference | 316 | Reference |
| No | 11 788 | 190 | 1.48 (1.18-1.84) | 210 | 1.17 (0.97-1.41) |
| Maternal blood transfusion | |||||
| No | 31 675 | 367 | Reference | 511 | Reference |
| Yes | 298 | 10 | 2.80 (1.43-5.48) | 15 | 2.66 (1.53-4.62) |
| Fetal or neonatal | |||||
| No. of fetuses | |||||
| 1 | 30 939 | 350 | Reference | 515 | Reference |
| ≥ 2 | 1034 | 27 | 1.78 (1.13-2.80) | 11 | 0.64 (0.34-1.20)† |
| Gestational age | |||||
| < 37 wk | 3057 | 62 | 1.42 (1.02-1.96) | 54 | 1.21 (0.88-1.66) |
| 37 wk to 39 wk + 6 d | 18331 | 191 | Reference | 248 | Reference |
| ≥ 40 wk | 10585 | 124 | 0.98 (0.77-1.24) | 224 | 1.19 (0.98-1.46) |
Note: CI = confidence interval, OR = odds ratio.
*A total of 32 876 cesarean deliveries were included in the analysis; 1115 deliveries were excluded because of missing values for neighbourhood-level income (n = 724), smoking (n = 283), stage of labour (n = 1) and/or gestational age (n = 118).
†p < 0.05 for association between risk factor and timing of infection (before v. after discharge).
Interpretation
In this 16-year study of nearly 34 000 births by cesarean delivery, the incidence of surgical site infection to 30 days post partum was 2.7%. More infections presented after discharge than before discharge (58.4% v. 41.6%), as noted by other investigators.15 Infection rates decreased over time. Our analysis identified some risk factors that are modifiable or known before delivery, such as prepregnancy weight and anticoagulation therapy, and some risk factors were associated differently with pre- versus postdischarge surgical site infection.
The incidence of surgical site infection of 2.7% observed in the present study is comparable to the lower end of the infection rates reported in the literature, which range from 0.16%3 to 9.6%.5 Rates reported from infection prevention and control programs are fairly consistent and are at the lower end of the range. 3,4 In a study from Nova Scotia, the authors reported an incidence of surgical site infection following cesarean delivery of 1.5% for 1988-2002 but followed women only to discharge.16 We do not know why Nova Scotia rates are at the lower end of the reported range. Possible contributing factors include universal access to health care, introduction of standardized antibiotic administration before cesarean delivery at some sites and the salutary effect of a provincial reproductive care program that sets quality standards and provides education to all obstetric health care providers. Variation in reported infection rates can often be attributed to different populations, time periods and definitions of surgical site infection, secular trends and improvements in health care.17 For example, Wloch and colleagues5 found a considerably higher infection rate than we did, possibly owing to higher prevalence of comorbidities such as diabetes and active follow-up. The decrease in our rate over a 16-year period, from 5.2% to 2.0%, is similar to the absolute decrease of 2.05% reported in an Australian study4 and to trends in health-care-associated infections seen in the United States.3 Possible reasons for these temporal trends include quality-improvement interventions such as surgical checklists, use of 2% chlorhexidine skin antisepsis, standing orders for systemic antimicrobial prophylaxis with adjusted dosages for obesity and increased administration of appropriate prophylactic antibiotics following published guidelines by the Centers for Disease Control and Prevention in 1999,18 the American College of Obstetricians and Gynecologists in 200319 and the Canadian Society of Obstetricians and Gynaecologists in 2010.11 Reported rates could also erroneously decrease if only predischarge infections are surveilled, as the length of postpartum stay has decreased over time.
We identified several risk factors for surgical site infection after cesarean delivery, including higher prepregnancy weight and weight gain during pregnancy. Like Wloch and colleagues,5 we observed a dose-response relation between prepregnancy weight and infection, with weighing 98.0 kg or more (approximating obese class III) being associated with more than 3 times the odds of surgical site infection compared to weighing 53.0-66.9 kg (approximating normal weight). Prepregnancy obesity has been a significant and strong independent risk factor for surgical site infection in most studies7,8 and, given its high prevalence (estimated at 35% in our cohort), is therefore important. Other risk factors identified in the present study that are theoretically modifiable included smoking, alcohol or drug abuse, gaining 30.0 kg or more during pregnancy and no antibiotic therapy. Antibiotic prophylaxis is an established protective factor for surgical site infection,20 whereas smoking has not been observed consistently to be a risk factor.21 Our findings regarding alcohol or drug abuse and weight gain as risk factors can be used to refine or to initiate and evaluate targeted clinical and infection prevention and control interventions to decrease the infection rate and lower this burden of illness following cesarean delivery on patients and the health care system.
Some factors associated with surgical site infection before discharge in our study may be linked to an increased potential for contamination during surgery (e.g., not receiving antibiotic therapy) and longer surgery duration (e.g., obesity and multiple fetuses). In contrast, risk factors associated with postdischarge infection may be indicative of increased potential for wound contamination (e.g., smoking and low socioeconomic status) and delayed wound healing or wound separation (e.g., obesity). These findings suggest that the effect of some individual risk factors is influenced by the length of time since surgery. A previous study of various operations (excluding cesarean delivery) also showed a significant difference between risk factors for surgical site infection before and after discharge, including age and duration of surgery.22 More studies are necessary to see whether these findings are observed in other populations and to separate the influence of location (hospital v. home) from that of time since surgery.
Limitations
As demand for quality improvement in health care increases, administrative claims databases have been used in recent years for surveillance of health-care-associated infections. In 2 systematic reviews of the diagnostic accuracy of administrative claims databases for this purpose, highly variable accuracy was found.23,24 One of the reviews23included surgical site infection following cesarean delivery and identified 3 validation studies.15,25,26 Leth and colleagues26 found sensitivities of infection diagnosed in hospital and after discharge of 77.1% and 68.9%, respectively, and specificities of 99.5% and 98.2%, respectively. A Canadian study showed that the sensitivity for detection of surgical site infection after cesarean delivery was 16.7% when using hospital data but 77.3% when including emergency department and physician claims databases; those authors concluded that the low sensitivity and positive predictive value make claims databases inadequate for use as quality indicators.25 A third, small study showed that infection after cesarean delivery identified through such data sources was confirmed in 40% of 204 cases, with some criteria for surgical site infection met in an additional 27% of cases.15 Since we used administrative databases to identify infections, there is likely some risk of misclassification. However, the comparability of our infection rates to those reported to the National Healthcare Safety Network3 and to our institution's infection prevention control program, serving 50% of the population of Nova Scotia (data not shown), is reassuring. Although hospital-based surveillance conducted by infection prevention and control programs remains the gold standard for detection of health-care-associated infection, it is resource intensive and time consuming. Such programs often do not have the resources to detect postdischarge infections and therefore will miss most of these events. Use of administrative databases, as in our study, can detect trends over time, facilitate multisite surveillance when surveillance systems are not integrated across administrative health regions and allow linking of other data sets, such as those with risk factors or longer-term health outcomes.
Data on some risk factors (e.g., maternal height) were unavailable for the entire study period, and some risk factors had a high proportion of missing values. Although our study covered a 16-year period, the data are historical, as we followed patients only until 2012. Finally, the NSAPD does not contain certain surgical information (e.g., length of surgery), so we did not include such details as potential risk factors for surgical site infection.
Conclusion
Use of administrative databases can identify postdischarge infection associated with health care that is not detected by hospital-based surveillance. The incidence of surgical site infection following cesarean delivery in Nova Scotia decreased over time. Obesity and weight gain during pregnancy were key risk factors for infection. Our findings are generalizable to populations with health care systems and demographic and clinical factors similar to those in Nova Scotia. Knowing which risk factors are associated with pre- versus postdischarge infection can assist clinicians in identifying women with specific risk factor profiles who may be at risk for surgical site infection. This offers an opportunity to develop systematic approaches to eliminate or reduce risk factors through patient, public and health care provider education, and system approaches such as timely administration of appropriate antibiotics.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/5/3/E546/suppl/DC1.
Supplementary Material
Acknowledgements
The authors thank the Reproductive Care Program of Nova Scotia and Health Data Nova Scotia for the use of their data. Part of this research was completed for a thesis to fulfill a portion of Felicia Ketcheson's degree requirements for an MSc degree in Community Health and Epidemiology, Faculty of Medicine, Dalhousie University. This research was previously presented at the 2016 Infection Prevention and Control Canada conference, May 15-18, 2016, Niagara Falls, Ont.
Footnotes
Funding: This study was supported by a Category A grant from the IWK Health Centre Research Office and a student stipend provided to Felicia Ketcheson through a Nova Scotia Support Grant provided by the Nova Scotia Health Research Foundation.
Disclaimer: Although part of this research is based on data obtained from the Nova Scotia Department of Health and Wellness, the observations and opinions expressed are those of the authors and do not represent those of either Health Data Nova Scotia or the Nova Scotia Department of Health and Wellness.
References
- 1.Best practices in the use of cesarean sections in Nova Scotia. Halifax: Reproductive Care Program of Nova Scotia; 2008. [Google Scholar]
- 2.Nova Scotia Atlee Perinatal Database report of indicators: 2005-2014. Halifax: Perinatal Epidemiology Research Unit, Dalhousie University; 2015. [Google Scholar]
- 3.Healthcare-associated infections (HAI) progress report - data tables. Atlanta: Centers for Disease Control and Prevention; 2016. [accessed 2017 Mar. 23]. Available https://www.cdc.gov/hai/surveillance/progress-report/index.html.
- 4.Worth L, Bull A, Spelman T, et al. Diminishing surgical site infections in Australia: time trends in infection rates, pathogens and antimicrobial resistance using a comprehensive Victorian surveillance program, 2002-2013. Infect Control Hosp Epidemiol. 2015;36:409–16. doi: 10.1017/ice.2014.70. [DOI] [PubMed] [Google Scholar]
- 5.Wloch C, Wilson J, Lamagni T, et al. Risk factors for surgical site infection following caesarean section in England: results from a multicentre cohort study. BJOG. 2012;119:1324–33. doi: 10.1111/j.1471-0528.2012.03452.x. [DOI] [PubMed] [Google Scholar]
- 6.Johnson A, Young D, Reilly J. Caesarean section surgical site infection surveillance. J Hosp Infect. 2006;64:30–5. doi: 10.1016/j.jhin.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 7.Anderson V, Chaboyer W, Gillespie B. The relationship between obesity and surgical site infections in women undergoing caesarean sections: an integrative review. Midwifery. 2013;29:1331–8. doi: 10.1016/j.midw.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Marchi J, Berg M, Dencker A, et al. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev. 2015;16:621–38. doi: 10.1111/obr.12288. [DOI] [PubMed] [Google Scholar]
- 9.Schneid-Kofman N, Sheiner E, Levy A, et al. Risk factors for wound infection following cesarean deliveries. Int J Gynaecol Obstet. 2005;90:10–5. doi: 10.1016/j.ijgo.2005.03.020. [DOI] [PubMed] [Google Scholar]
- 10.Merchavy S, Levy A, Holcberg G, et al. Method of placental removal during cesarean delivery and postpartum complications. Int J Gynaecol Obstet. 2007;98:232–6. doi: 10.1016/j.ijgo.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 11.van Schalkwyk J, Van Eyk N Society of Obstetricians and Gynaecologists of Canada Infectious Diseases Committee. Antibiotic prophylaxis in obstetric procedures. J Obstet Gynaecol Can. 2010;32:878–92. doi: 10.1016/S1701-2163(16)34662-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayoub F, Quirke M, Conroy R, et al. Chlorhexidine-alcohol versus povidone-iodine for pre-operative skin preparation: a systematic review and meta-analysis. Int J Surg Open. 2015;1:41–6. [Google Scholar]
- 13.Nova Scotia Atlee Perinatal Database report of indicators: 2002-2011. Halifax: Perinatal Epidemiology Research Unit, Dalhousie University; 2012. [Google Scholar]
- 14.Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 15.Miner AL, Sands KE, Yokoe DS, et al. Enhanced identification of postoperative infections among outpatients. Emerg Infect Dis. 2004;10:1931–7. doi: 10.3201/eid1011.040784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen VM, O'Connell CM, Baskett TF. Maternal morbidity associated with cesarean delivery without labor compared with induction of labor at term. Obstet Gynecol. 2006;108:286–94. doi: 10.1097/01.AOG.0000215988.23224.e4. [DOI] [PubMed] [Google Scholar]
- 17.Corcoran S, Jackson V, Coulter Smith S, et al. Surgical site infection after cesarean section: implementing 3 changes to improve the quality of patient care. Am J Infect Control. 2013;41:1258–63. doi: 10.1016/j.ajic.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 18.Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132, quiz 133-4, discussion 96. [PubMed] [Google Scholar]
- 19.American College of Obstetricians and Gynecologists. ACOG practice bulletin number 47, October 2003: prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2003;102:875–82. doi: 10.1016/s0029-7844(03)00984-0. [DOI] [PubMed] [Google Scholar]
- 20.Smaill FM, Grivell RM. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database Syst Rev. 2010:CD007482.. doi: 10.1002/14651858.CD007482.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boggess KA, Tita A, Jauk V, et al. Risk factors for postcesarean maternal infection in a trial of extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2017;129:481–5. doi: 10.1097/AOG.0000000000001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delgado Rodríguez M, Gómez Ortega A, Sillero Arenas M, et al. Epidemiology of surgical-site infections diagnosed after hospital discharge: a prospective cohort study. Infect Control Hosp Epidemiol. 2001;22:24–30. doi: 10.1086/501820. [DOI] [PubMed] [Google Scholar]
- 23.van Mourik MS, van Duijn PJ, Moons KG, et al. Accuracy of administrative data for surveillance of health care-associated infections: a systematic review. BMJ Open. 2015;5:e008424. doi: 10.1136/bmjopen-2015-008424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goto M, Ohl M, Schweizer M, et al. Accuracy of administrative code data for the surveillance of healthcare-associated infections: a systematic review and meta-analysis. Clin Infect Dis. 2014;58:688–96. doi: 10.1093/cid/cit737. [DOI] [PubMed] [Google Scholar]
- 25.Daneman N, Ma X, Eng-Chong M, et al. Validation of administrative population-based data sets for the detection of cesarean delivery surgical site infection. Infect Control Hosp Epidemiol. 2011;32:1213–5. doi: 10.1086/662623. [DOI] [PubMed] [Google Scholar]
- 26.Leth R, Norgarrd M, Uldbjerg N, et al. Surveillance of selected post-caesarean infections based on electronic registries: validation study including postdischarge infections. J Hosp Infect. 2010;75:200–4. doi: 10.1016/j.jhin.2009.11.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.