Abstract
The meniscal allograft transplantation (MAT) has been reported to be an effective treatment in terms of pain relief and functional improvement in symptomatic meniscus-deficient knee. The medial MAT is usually performed with the bone plug technique or soft tissue fixation for root fixation. We describe medial MAT with modified bone plug technique that permits easy passage of posterior bone plugs and facilitates bone-to-bone healing. With this method, an anterior bone plug with a long cylindrical shape is prepared, and the posterior bone plug is prepared with a flat bone shell containing a cancellous portion. This modified technique facilitates graft passage as well as bone-to-bone healing.
Numerous biomechanical, clinical review studies about meniscal allograft transplantation (MAT) have been reported, and most of them have revealed that MAT improved knee function and symptoms in meniscus-deficient knee.1, 2, 3, 4 MAT has been implemented with various surgical techniques, which have been categorized into soft tissue fixation and bone plug fixation techniques.1, 2, 5, 6, 7 The medial and lateral sides have distinct anatomic and biomechanical characteristics; there is less mobility and a longer distance between the anterior and posterior roots in the medial meniscus.8, 9, 10 Hence, medial MAT has been preferred for bone plug fixation for anterior and posterior roots,5, 6, 11 and it has been supported by the fact that bone fixation leads to better results than soft tissue fixation.12
However, passing the 10 × 10-mm cylindrical bone plugs of the posterior horn into the knee is technically demanding in patients with tight medial compartments, because the medial femoral condyle often obstructs the approach to the posterior portion of the knee joint during arthroscopic procedures. Even though soft tissue alone is technically easier, several studies have reported that load transmission is superior when the graft is secured with bone.12, 13
Our modified bone plug technique was designed to allow an easy passage for the posterior root of the allograft by reducing the size of the bone plug rather than making a large tibial tunnel to fix the posterior root. We describe an effective surgical technique of arthroscopic medial MAT using a modified bone plug and small tibial tunnel without creating an additional bone tunnel as with soft tissue fixation (Video 1).
Surgical Technique
The surgical indications and contraindications are listed in Table 1. Table 2 describes the advantages and disadvantages, and Table 3 presents the pitfalls and tips of the present technique.
Table 1.
Medial Meniscal Allograft Transplantation Indications
| Indications |
|---|
| Age: between 20 and 45 years |
| Body mass index <30 |
| Symptomatic knee more than 1 year after previous total or subtotal meniscectomy |
| Outerbridge classification of less than grade 3, repairable focal grade 4 |
| Kellgren-Lawrence grade I or II, some salvage cases for grade III |
| Symmetric alignment (<3°) |
| Ability to endure a relatively high-demand activity |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| 1. Easy fixation of the posterior bone plug is possible in the tight medial compartment. 2. Secure fixation is achieved through bone-to-bone healing. 3. Only the posterior bone socket rather than the transtibial tunnel is needed. |
1. There would be still concern about healing potential between the posterior bone shell of the graft and bone. 2. Making 2-mm-deep posterior bone shell is sometimes technically demanding and learning curve is in play. |
Table 3.
Pitfalls and Tips
| Pitfalls | Tips |
|---|---|
| 1. It is difficult to make a posterior root footprint in the anatomic position and secure the graft through a tight posteromedial joint space. 2. Sometimes, the posterior root of the allograft is bent and loosened after fixation. |
1. The posterior bone plug is reduced for the bone shell containing cancellous bone. 2. Superficial medial collateral ligament release is performed using a periosteum elevator to obtain increased medial compartment opening. 3. Leading suture of bone plug is pulled out via the anterolateral side of tibia to provide firm fixation. |
Intra-articular Preparation and Skin Incision
The arthroscope is introduced through the anterolateral portal, and a thorough examination is performed. After diagnostic arthroscopy, a 3-cm longitudinal skin incision is made at the anteromedial aspect of the proximal tibia, and superficial medial collateral ligament release is performed using a periosteum elevator to widen the medial compartment opening, which provides better visualization and working space as described in previous published methods.14, 15
The remnant meniscus is arthroscopically resected, leaving 1 to 2 mm of bleeding at the peripheral rim, and the exact anterior and posterior root attachments are marked using electrocautery (ArthroCare, Austin, TX). Viewing from the anterolateral portal with instruments inserted through the anteromedial portal, the footprint of the posterior root is re-marked by electrocautery and decorticated at a diameter of about 10 mm and a depth of 5 mm using a curette until the subchondral bone is exposed (Fig 1). Then, a 4-cm anterior arthrotomy is done just medial to the patellar tendon in line with the previous anteromedial portal, and the footprint of the anterior root is re-marked by electrocautery. Next, a vertical incision is performed for routine posteromedial approach to expose the posteromedial capsule releasing from the medial head of the gastrocnemius, and to repair the medial meniscal allograft later. An elevator is used to release soft tissue adhesion between the anteromedial and posteromedial sides to make the same interval. Finally, a 2-cm oblique incision is made on the Gerdy tubercle for creating 2 tibial tunnels.
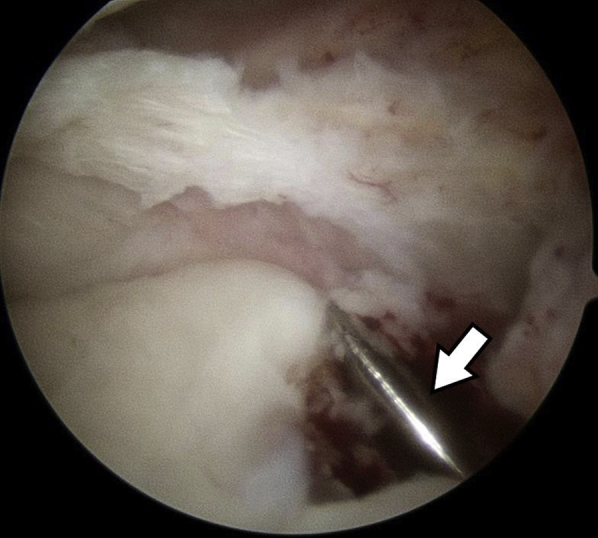
Fig 1.

Viewing from the anterolateral portal, a tibial socket (black arrow), with a diameter of about 10 mm and a depth of 5 mm, for posterior bone shell fixation is made using a curette until subchondral bone is exposed via the anteromedial portal on the left knee.
Tibial Tunnel Preparation for Root Attachments
The tibial tunnel to pull out of the posterior root leading suture is made by drilling from the Gerdy tubercle to the medial meniscus posterior root footprint with an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) and the guide pin (Fig 2). A suture-passing wire with the loop positioned anteriorly is inserted through the posterior tibial tunnel, and the suture-passing wire is retrieved through the anterior arthrotomy incision. Through an anterior arthrotomy, 2 suture-passing wires with the loop positioned posteriorly for the guide suture are passed via the posteromedial capsule in an inside-to-out fashion superior and inferior to the remnant medial meniscus (Fig 3), and the ends of the suture-passing wires are held by Kelly clamps. The footprint of the anterior root is visualized from the anterior arthrotomy site, and the anterior bone plug tunnel (10 mm in diameter, 15 mm in depth) is created under direct visualization using a guide pin followed by a 10-mm reamer (Fig 4). After reaming, a suture-passing wire with the loop positioned anteriorly is inserted through the exit of the anterior tibial tunnel on the Gerdy tubercle, and the suture-passing wire is retrieved through the anterior arthrotomy incision.
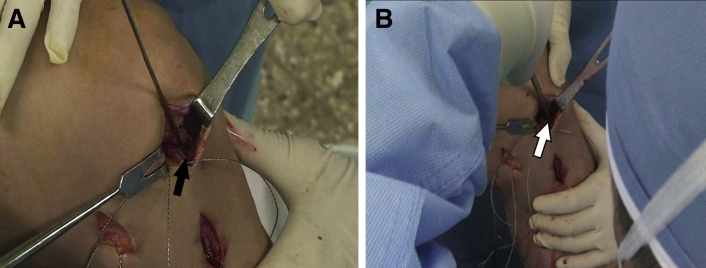
Fig 2.
Viewing from the anterolateral portal, the tibial tunnel for the posterior root leading suture is created by drilling from the Gerdy tubercle to the posterior root footprint using anterior cruciate ligament reconstruction (ACLR) tibial tunnel guide (Linvatec) and the guide pin (white arrow) on the left knee with valgus flexion at extension.
Fig 3.
Through an anteromedial arthrotomy, 2 suture-passing wires with the loop positioned posteriorly for the posterior traction suture are passed via the posteromedial capsule in an inside-to-out fashion superior (black arrowhead) and inferior (black arrow) of the remnant left medial meniscus viewing from the anterolateral portal. The white arrow indicates the suture-passing wire for the traction suture.
Fig 4.
The tibial tunnel for the anterior bone plug (10 mm in diameter, 15 mm in depth) is created under direct visualization using a guide pin (A) (black arrow) followed by a 10-mm reamer (B) (white arrow) via an anteromedial arthrotomy on the left knee.
Graft Preparation
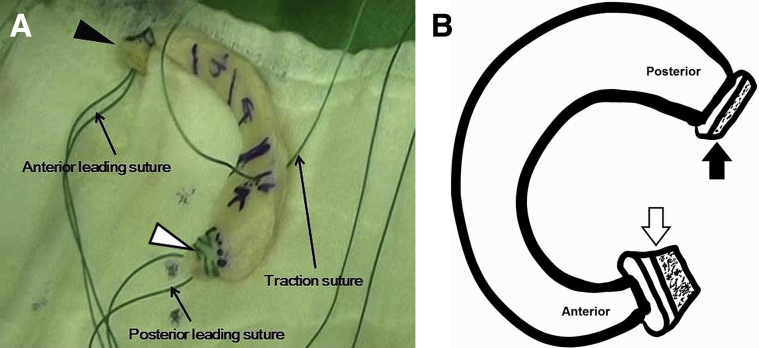
Fresh-frozen and nonirradiated grafts are used in all cases, and graft size is determined preoperatively on anteroposterior and lateral radiographs with a scanogram for correction of magnification, as described by a previous article.16 This modified method of measurement has been estimated to reduce the graft size by 5% compared with the method by Pollard et al,17 which decreases the percentage of meniscal extrusion after MAT without any adverse outcome clinically or radiographically.16 An 8-mm-diameter, 8-mm-deep cylindrical anterior bone plug and an 8-mm-diameter, 2-mm-deep posterior bone shell are cored from the meniscal allograft (Fig 5). A 1-mm drill bit is used to create a suture hole in each bone plug, and a no. 5 Ethibond (Ethicon, Somerville, NJ) is inserted through the hole of each bone plug. Anterior and posterior horns including bone are sutured with no. 5 Ethibond by placing a baseball stitch (Fig 5). The posterior guide suture is placed 10 mm medially from the posterior bone plug for later traction and spreading using no. 2 Ethibond (Fig 5).
Fig 5.
Meniscal allograft is prepared for medial meniscus transplantation with modified bone plug technique. (A) The posterior bone plug (black arrowhead) measures 8 mm in diameter and 2 mm in depth, whereas the anterior bone plug (white arrowhead) measures 8 mm in diameter and 8 mm in depth. Anterior and posterior leading sutures and posterior traction suture are placed using no. 5 and no. 2 Ethibond. (B) Schema of medial meniscal allograft for the modified bone plug technique. The black arrow and the white arrow indicate the posterior bone shell and anterior bone plug, respectively.
Allograft Insertion and Fixation
The graft, with leading sutures and guide suture connected to the loop of each suture-passing wire, is inserted into the joint through the anterior arthrotomy by pulling out the opposite side of the loop of the suture-passing wire. Under arthroscopic guide, the posterior bone shell and the anterior bone plug of the graft are reduced into the root insertion under traction of the posterior guide suture through the capsule, and the whole medial meniscus allograft is spread evenly. Occasionally, graft passage is facilitated by applying valgus stress and cyclic loading. Then, the anterior and posterior bone plug stitches are tied firmly together on the anterolateral tibial cortex.
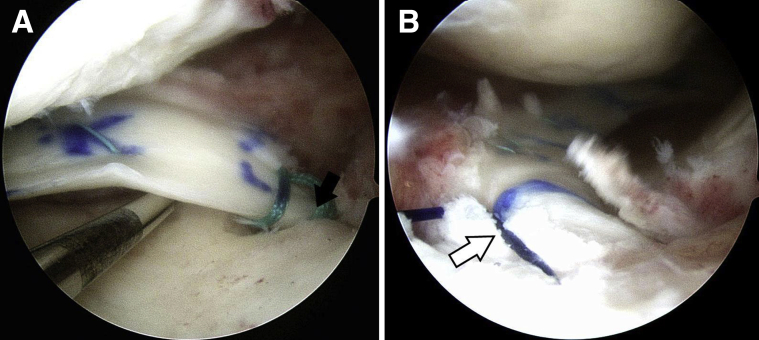
Viewing from the anterolateral portal, the posterior one-third and middle horn are repaired with 2 superior and 1 inferior obliquely arranged sutures in an inside-out fashion with double-armed needles containing nonabsorbable suture materials. Then, the leading sutures are tied on the anterolateral tibial cortex. This repair procedure allows the allograft to secure to the remnant meniscus and the capsule firmly. The anterior one-third is repaired with 3 or 4 direct sutures using no. 2 polydioxanone (Ethicon) through the anterior arthrotomy in an outside-in fashion. Once graft fixation is confirmed with arthroscopy, the sutures are ligated. A final arthroscopic evaluation is performed to confirm the fixed posterior and anterior roots and tension of the entire medial meniscus (Fig 6).
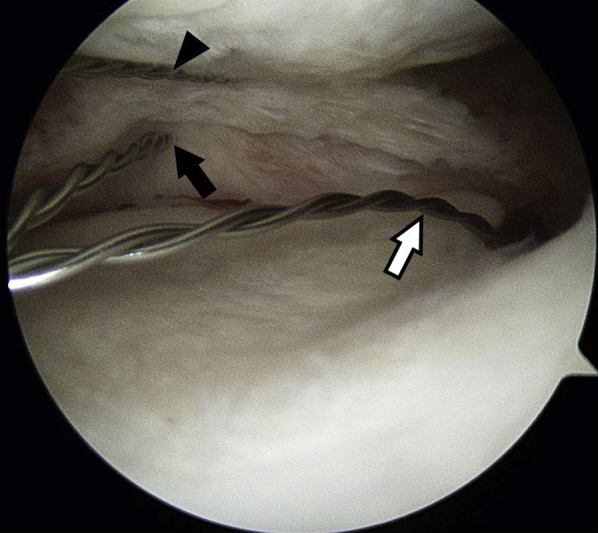
Fig 6.
Final arthroscopic evaluation is performed to confirm the fixed posterior (A) and anterior (B) roots and tension of the left entire medial meniscus, viewing from the anterolateral portal. The black arrow shows the firm fixed posterior root, and the white arrow represents the anterior horn, which is well secured to the capsule and anterior root insertion.
Discussion
The purpose of this Technical Note was to describe an arthroscopic medial MAT with a modified bone plug technique. The short- and midterm results of MAT have been reported to be successful in terms of pain relief and functional improvement.1, 2, 6 A recent systematic review of MAT outcomes concluded that MAT allowed return to the same level of sports in 75% to 85% of the patients at short- to midterm follow-up (Level IV evidence), and might prevent progression of cartilage damaged at long-term follow-up, but may not prevent degeneration in previously healthy cartilage.2
Even though there has been debate on graft fixation methods, it has been shown that the bone fixation is superior to soft tissue fixation.12, 18, 19, 20 Wang et al19 compared the dynamic contact mechanics between bone plug fixation and soft fixation in medial MAT using 7 human cadaveric knees and concluded that the mean contact stress significantly decreased with bone plug fixation (5.0 ± 0.7 MPa) but not with soft tissue fixation (5.9 ± 0.7 MPa), and bone plug fixation restored it closer to the intact condition. Abat et al18 revealed that soft tissue fixation in medial MAT (35.9% ± 18.1%) showed a significantly higher degree of meniscal extrusion than bone plug fixation (25.8% ± 16.2%) on magnetic resonance imaging at a minimum 3 years' follow-up, although there was no influence on the functional outcome. Kim et al5 reported that the 10-year survival rate was 98.0% (95% confidence interval, 94.1%-100%), and the 15-year survival rate was 93.3% (95% confidence interval, 83.7%-100%) according to the Kaplan-Meier analysis after MAT with bone fixation technique. In addition, the medial meniscus has lower mobility and has a larger anteroposterior diameter than the lateral meniscus8, 9, 10; hence, bone plug fixation would be more beneficial than soft tissue fixation for anterior and posterior roots in medial MAT.5, 6, 11
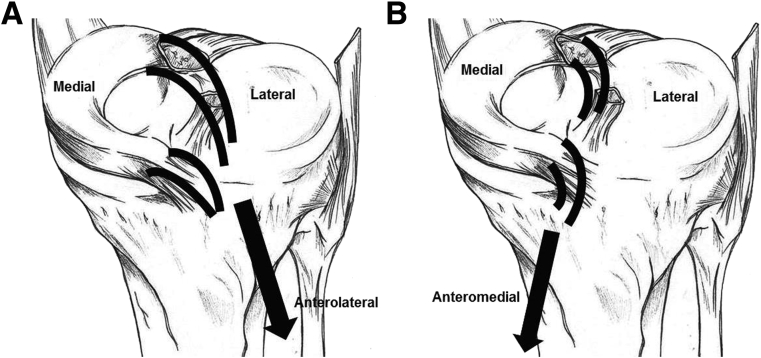
The bone plug fixation technique commonly used for medial MAT is technically challenging, because it is difficult to make a posterior root footprint in the anatomic position under arthroscopy and secure the graft with a 10 × 10-mm cylindrical bone plug through a tight posteromedial joint space. There has been some efforts to overcome these problems including reducing medial tibial spine with notchplasty,5 and using a femoral distractor.21 The alternative we prefer is a modified bone plug technique in which the bone plug of the posterior root is reduced, leaving a depth of only 2 mm of cancellous bone for the bone shell. This technique is advantageous for easy graft passage and bone-to-bone healing. Additionally, the tibial plateau can be preserved for the concomitant ligament reconstruction procedure as much as possible to prevent converging tunnels, because a large and long transtibial tunnel is not necessary with this technique—which needs only a guide pin–drilled tunnel to pull out the leading suture. The other thing the current authors have assumed is that leading sutures of anterior and posterior bone plugs of the medial meniscal allograft are pulled out via the anterolateral side of the tibia, which could provide firmer fixation than on the anteromedial side of the tibia (Fig 7).
Fig 7.
Leading sutures of anterior and posterior bone plugs of the left medial meniscal allograft are pulled out via the anterolateral side of the tibia (A), and it could provide more firm fixation than the anteromedial side of the tibia (B).
There would be concern about the healing potential between the posterior bone shell of the graft and the tibial plateau. Ha et al22 reported that 83.3% of 22 cases and 81.8% of 11 cases showed complete healing of the posterior bone shell of the medial meniscus allograft on magnetic resonance imaging and second-look arthroscopy, respectively. They suggested that the healing status between the posterior bone shell and the tibial plateau was reliable.
In summary, the described arthroscopic medial MAT with modified bone plug technique facilitates easy fixation of the posterior bone plug, which is only a 2-mm-deep flat bone shell containing cancellous bone and bone-to-bone healing.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We demonstrate the surgical technique of arthroscopic medial meniscus allograft transplantation with modified bone plug technique on the left knee. After diagnostic arthroscopy, a 3-cm longitudinal skin incision is made at the anteromedial aspect of the proximal tibia, and superficial medial collateral ligament release is performed using a periosteum elevator to widen the medial compartment opening, which provides better visualization and working space. The remnant meniscus is arthroscopically resected, leaving 1-2 mm of bleeding at the peripheral rim, and the exact anterior and posterior root attachments are marked using electrocautery (ArthroCare). Viewing from the anterolateral portal with instruments inserted through the anteromedial portal, the footprint of the posterior root is re-marked by electrocautery and decorticated at a diameter of about 10 mm and a depth of 5 mm using a curette until the subchondral bone is exposed. Then, a 4-cm anterior arthrotomy is done just medial to the patellar tendon in line with the previous anteromedial portal, and the footprint of the anterior root is re-marked by electrocautery. Next, a vertical incision is made for routine posteromedial approach to expose the posteromedial capsule releasing from the medial head of the gastrocnemius, and to repair the medial meniscal allograft later. Finally, a 2-cm oblique incision is made on the Gerdy tubercle for creating 2 tibial tunnels. The tibial tunnel to pull out of the posterior root leading suture is made by drilling from the Gerdy tubercle to the medial meniscus posterior root footprint with an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) and the guide pin. A suture-passing wire with the loop positioned anteriorly is inserted through the posterior tibial tunnel, and the suture-passing wire is retrieved through the anterior arthrotomy incision. Through an anterior arthrotomy, 2 suture-passing wires with the loop positioned posteriorly for the guide suture are passed via the posteromedial capsule in an inside-to-out fashion superior and inferior of the remnant medial meniscus, and the ends of the suture-passing wires are held by Kelly clamps. The footprint of the anterior root is visualized from the anterior arthrotomy site, and the anterior bone plug tunnel (10 mm in diameter, 15 mm in depth) is created under direct visualization using a guide pin followed by a 10-mm reamer. After reaming, a suture-passing wire with the loop positioned anteriorly is inserted through the exit of the anterior tibial tunnel on the Gerdy tubercle, and the suture-passing wire is retrieved through the anterior arthrotomy incision. An 8-mm-diameter, 8-mm-deep cylindrical anterior bone plug and an 8-mm-diameter, 2-mm-deep posterior bone shell are cored from the meniscal allograft. A 1-mm drill bit is used to create a suture hole in each bone plug, and no. 5 Ethibond (Ethicon) is inserted through the hole of each bone plug. Anterior and posterior horns including bone are sutured with no. 5 Ethibond by placing a baseball stitch. The posterior guide suture is placed 10 mm medially from the posterior bone plug for later traction and spreading using no. 2 Ethibond. The graft, with leading sutures and guide suture connected to the loop of each suture-passing wire, is inserted into the joint through the anterior arthrotomy by pulling out the opposite side of the loop of the suture-passing wire. Under arthroscopic guide, the posterior bone shell and the anterior bone plug of the graft are reduced into the root insertion under traction of the posterior guide suture through the capsule, and the whole medial meniscus allograft is spread evenly. Occasionally, graft passage is facilitated by applying valgus stress and cyclic loading. Then, the anterior and posterior bone plug stitches are tied firmly together on the anterolateral tibial cortex. Viewing from the anterolateral portal, the posterior one-third and middle horn are repaired with 2 superior and 1 inferior obliquely arranged sutures in an inside-out fashion with double-armed needles containing nonabsorbable suture materials. Then, the leading sutures are tied on the anterolateral tibial cortex. The anterior one-third is repaired with 3 or 4 direct sutures using no. 2 polydioxanone (Ethicon) through the anterior arthrotomy in an outside-in fashion. Once graft fixation is confirmed with arthroscopy, the sutures are ligated. A final arthroscopic evaluation is performed to confirm the fixed posterior and anterior roots and tension of the entire medial meniscus. The current modified technique could provide an easy fixation of the posterior bone plug and facilitate bone-to-bone healing by reducing the posterior bone plug, which is only a 2-mm-deep flat bone shell containing cancellous bone.
References
- 1.Rosso F., Bisicchia S., Bonasia D.E., Amendola A. Meniscal allograft transplantation: A systematic review. Am J Sports Med. 2015;43:998–1007. doi: 10.1177/0363546514536021. [DOI] [PubMed] [Google Scholar]
- 2.Samitier G., Alentorn-Geli E., Taylor D.C. Meniscal allograft transplantation. Part 2: Systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23:323–333. doi: 10.1007/s00167-014-3344-3. [DOI] [PubMed] [Google Scholar]
- 3.Smith N.A., MacKay N., Costa M., Spalding T. Meniscal allograft transplantation in a symptomatic meniscal deficient knee: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:270–279. doi: 10.1007/s00167-014-3310-0. [DOI] [PubMed] [Google Scholar]
- 4.Samitier G., Alentorn-Geli E., Taylor D.C. Meniscal allograft transplantation. Part 1: Systematic review of graft biology, graft shrinkage, graft extrusion, graft sizing, and graft fixation. Knee Surg Sports Traumatol Arthrosc. 2015;23:310–322. doi: 10.1007/s00167-014-3334-5. [DOI] [PubMed] [Google Scholar]
- 5.Kim J.M., Bin S.I., Lee B.S. Long-term survival analysis of meniscus allograft transplantation with bone fixation. Arthroscopy. 2017;33:387–393. doi: 10.1016/j.arthro.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Ha J.K., Jang H.W., Jung J.E., Cho S.I., Kim J.G. Clinical and radiologic outcomes after meniscus allograft transplantation at 1-year and 4-year follow-up. Arthroscopy. 2014;30:1424–1429. doi: 10.1016/j.arthro.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 7.Spalding T., Parkinson B., Smith N.A., Verdonk P. Arthroscopic meniscal allograft transplantation with soft-tissue fixation through bone tunnels. Arthrosc Tech. 2015;4:e559–e563. doi: 10.1016/j.eats.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smigielski R., Becker R., Zdanowicz U., Ciszek B. Medial meniscus anatomy—From basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8–14. doi: 10.1007/s00167-014-3476-5. [DOI] [PubMed] [Google Scholar]
- 9.Ellman M.B., LaPrade C.M., Smith S.D. Structural properties of the meniscal roots. Am J Sports Med. 2014;42:1881–1887. doi: 10.1177/0363546514531730. [DOI] [PubMed] [Google Scholar]
- 10.Fox A.J., Wanivenhaus F., Burge A.J., Warren R.F., Rodeo S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin Anat. 2015;28:269–287. doi: 10.1002/ca.22456. [DOI] [PubMed] [Google Scholar]
- 11.Yoon K.H., Lee S.H., Park S.Y., Kim H.J., Chung K.Y. Meniscus allograft transplantation: A comparison of medial and lateral procedures. Am J Sports Med. 2014;42:200–207. doi: 10.1177/0363546513509057. [DOI] [PubMed] [Google Scholar]
- 12.Rodeo S.A. Meniscal allografts—Where do we stand? Am J Sports Med. 2001;29:246–261. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 13.Paletta G.A., Jr., Manning T., Snell E., Parker R., Bergfeld J. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med. 1997;25:692–698. doi: 10.1177/036354659702500519. [DOI] [PubMed] [Google Scholar]
- 14.Chung K.S., Ha J.K., Ra H.J., Kim J.G. Does release of the superficial medial collateral ligament result in clinically harmful effects after the fixation of medial meniscus posterior root tears? Arthroscopy. 2017;33:199–208. doi: 10.1016/j.arthro.2016.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Lee D.W., Kim M.K., Jang H.S., Ha J.K., Kim J.G. Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: Comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30:1439–1446. doi: 10.1016/j.arthro.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 16.Jang S.H., Kim J.G., Ha J.G., Shim J.C. Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy. 2011;27:914–922. doi: 10.1016/j.arthro.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 17.Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–687. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 18.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Gonzalez-Lucena G., Monllau J.C. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40:1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 19.Wang H., Gee A.O., Hutchinson I.D. Bone plug versus suture-only fixation of meniscal grafts: Effect on joint contact mechanics during simulated gait. Am J Sports Med. 2014;42:1682–1689. doi: 10.1177/0363546514530867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abat F., Gelber P.E., Erquicia J.I., Tey M., Gonzalez-Lucena G., Monllau J.C. Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1516–1522. doi: 10.1007/s00167-012-2032-4. [DOI] [PubMed] [Google Scholar]
- 21.Sekiya J.K., Ellingson C.I. Meniscal allograft transplantation. J Am Acad Orthop Surg. 2006;14:164–174. doi: 10.5435/00124635-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Ha J.K., Sung J.H., Shim J.C., Seo J.G., Kim J.G. Medial meniscus allograft transplantation using a modified bone plug technique: Clinical, radiologic, and arthroscopic results. Arthroscopy. 2011;27:944–950. doi: 10.1016/j.arthro.2011.02.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We demonstrate the surgical technique of arthroscopic medial meniscus allograft transplantation with modified bone plug technique on the left knee. After diagnostic arthroscopy, a 3-cm longitudinal skin incision is made at the anteromedial aspect of the proximal tibia, and superficial medial collateral ligament release is performed using a periosteum elevator to widen the medial compartment opening, which provides better visualization and working space. The remnant meniscus is arthroscopically resected, leaving 1-2 mm of bleeding at the peripheral rim, and the exact anterior and posterior root attachments are marked using electrocautery (ArthroCare). Viewing from the anterolateral portal with instruments inserted through the anteromedial portal, the footprint of the posterior root is re-marked by electrocautery and decorticated at a diameter of about 10 mm and a depth of 5 mm using a curette until the subchondral bone is exposed. Then, a 4-cm anterior arthrotomy is done just medial to the patellar tendon in line with the previous anteromedial portal, and the footprint of the anterior root is re-marked by electrocautery. Next, a vertical incision is made for routine posteromedial approach to expose the posteromedial capsule releasing from the medial head of the gastrocnemius, and to repair the medial meniscal allograft later. Finally, a 2-cm oblique incision is made on the Gerdy tubercle for creating 2 tibial tunnels. The tibial tunnel to pull out of the posterior root leading suture is made by drilling from the Gerdy tubercle to the medial meniscus posterior root footprint with an anterior cruciate ligament reconstruction tibial tunnel guide (Linvatec) and the guide pin. A suture-passing wire with the loop positioned anteriorly is inserted through the posterior tibial tunnel, and the suture-passing wire is retrieved through the anterior arthrotomy incision. Through an anterior arthrotomy, 2 suture-passing wires with the loop positioned posteriorly for the guide suture are passed via the posteromedial capsule in an inside-to-out fashion superior and inferior of the remnant medial meniscus, and the ends of the suture-passing wires are held by Kelly clamps. The footprint of the anterior root is visualized from the anterior arthrotomy site, and the anterior bone plug tunnel (10 mm in diameter, 15 mm in depth) is created under direct visualization using a guide pin followed by a 10-mm reamer. After reaming, a suture-passing wire with the loop positioned anteriorly is inserted through the exit of the anterior tibial tunnel on the Gerdy tubercle, and the suture-passing wire is retrieved through the anterior arthrotomy incision. An 8-mm-diameter, 8-mm-deep cylindrical anterior bone plug and an 8-mm-diameter, 2-mm-deep posterior bone shell are cored from the meniscal allograft. A 1-mm drill bit is used to create a suture hole in each bone plug, and no. 5 Ethibond (Ethicon) is inserted through the hole of each bone plug. Anterior and posterior horns including bone are sutured with no. 5 Ethibond by placing a baseball stitch. The posterior guide suture is placed 10 mm medially from the posterior bone plug for later traction and spreading using no. 2 Ethibond. The graft, with leading sutures and guide suture connected to the loop of each suture-passing wire, is inserted into the joint through the anterior arthrotomy by pulling out the opposite side of the loop of the suture-passing wire. Under arthroscopic guide, the posterior bone shell and the anterior bone plug of the graft are reduced into the root insertion under traction of the posterior guide suture through the capsule, and the whole medial meniscus allograft is spread evenly. Occasionally, graft passage is facilitated by applying valgus stress and cyclic loading. Then, the anterior and posterior bone plug stitches are tied firmly together on the anterolateral tibial cortex. Viewing from the anterolateral portal, the posterior one-third and middle horn are repaired with 2 superior and 1 inferior obliquely arranged sutures in an inside-out fashion with double-armed needles containing nonabsorbable suture materials. Then, the leading sutures are tied on the anterolateral tibial cortex. The anterior one-third is repaired with 3 or 4 direct sutures using no. 2 polydioxanone (Ethicon) through the anterior arthrotomy in an outside-in fashion. Once graft fixation is confirmed with arthroscopy, the sutures are ligated. A final arthroscopic evaluation is performed to confirm the fixed posterior and anterior roots and tension of the entire medial meniscus. The current modified technique could provide an easy fixation of the posterior bone plug and facilitate bone-to-bone healing by reducing the posterior bone plug, which is only a 2-mm-deep flat bone shell containing cancellous bone.