Abstract
Objectives
To compare the long-term functional and radiographic outcomes of the proximal femoral nail antirotation-Asia (PFNA-II) and INTERTAN nail (IT) in the management of intertrochanteric femoral fractures (IFFs) (AO/OTA Type 31A1.1-A2.3) in elderly patients with primary osteoporosis.
Methods
A retrospective comparative study was performed in our institution. From January 2009 to March 2012, 243 patients with osteoporosis (243 hips) with IFFs (AO/OTA Type 3.1A1.1-A2.3) underwent repair with either a PFNA-II or IT. Follow-up assessments were performed 1, 3, 6, 9, and 12 months postoperatively and every year thereafter. All implant position changes were noted. Patient-related functional outcomes were evaluated based on the Harris hip score.
Results
In total, 174 patients with osteoporosis (IT, n = 86; PFNA-II, n = 88) were evaluated during a mean follow-up period of 40 months (range, 38–60 months). An increased risk of femoral shaft fracture after implant removal was observed at month 9 of follow-up in 0.0% and 4.4% of the IT and PFNA-II groups, respectively. This difference remained over time with rates of 1.1% and 6.8%, respectively, at the last follow-up.
Conclusion
The IT nail appears to be a reliable implant in the management of IFFs (AO/OTA Type 3.1A1.1-A2.3) in elderly patients with primary osteoporosis.
Keywords: Intertrochanteric femur fracture, Complication, InterTAN nail, Proximal femoral nail anti-rotation-Asia, Harris Hip Score
Introduction
Short-term follow-up results from previous studies1–3 have shown that the INTERTAN nail (IT) (Smith–Nephew, Memphis, TN) is superior to the proximal femoral nail antirotation-Asia (PFNA-II) (Synthes, Solothurn, Switzerland) for treatment of intertrochanteric femoral fractures (IFFs) in patients with osteoporosis. Both nails have a tendency to provide rotational and angular stability, decrease the risks of various complications, increase the primary healing rate, and lead to rapid functional recovery in the management of stable or unstable IFFs. These results, together with those from trials of similar short-term duration, also support the fact that few differences exist between the two implants, particularly in patients without osteoporosis and in relatively young patients.3,4 However, the efficacy of both nails over a longer time period has been less well studied in elderly patients with osteoporosis (thin or brittle bones) diagnosed by bone mineral density.
Therefore, based on the current information, the best treatment (IT or PFNA-II without greater exposure of the fracture or bone surfaces and without extensive muscle dissection) for stable or unstable IFFs in elderly patients with osteoporosis remains controversial. The treatment of IFFs with an IT or PFNA-II is associated with various complications.5,6 In previous reports,1–3 more than 30% of patients with osteoporosis sustained screw cut-out, loss of reduction, delayed union, malunion or nonunion, and various deformities of the femur. Additionally, IFF fixation failure is more prone to osteoporosis. Numerous in vitro and in vivo investigations1–3,7–9 have confirmed that the IT and PFNA-II have distinct advantages based on the close proximity to the line of weight bearing, resulting in a shorter lever arm. However, achieving rigid fixation in elderly patients with osteoporosis may be rather difficult with both nails, and clinical outcomes are likely to be poor. Osteoporosis-related morbidity is a major problem in elderly patients, particularly in elderly female patients.10 Inadequate surgical interventions caused by poor bone conditions have been reported in 20% to 40% of patients with osteoporosis and unstable or displaced IFFs.11 In these elderly patients, early postoperative weight bearing often leads to impaired mobility and delayed weight bearing and may further weaken the bone, culminating in a dissatisfactory result.1,3 Although numerous studies of fixation with the IT and PFNA-II that were primarily based on short-term (≤1 year) evaluation indicators such as the operation time, length of stay, blood loss, fluoroscopy time, and pain demonstrated that both nails achieve good functional and radiographic outcomes,3,12–14 few studies have compared both nails in the management of IFFs (AO/OTA Type 3.1A1.1-A2.3) in terms of long-term functional and radiographic outcomes in elderly patients with osteoporosis. Thus, conclusive data regarding which implant is more advantageous are lacking in this area.
The aim of this initial study was to compare the clinical and radiographic outcomes of the IT and PFNA-II in the management of IFFs (AO/OTA Type 3.1A1.1-A2.3) in elderly patients with osteoporosis during a minimum 3-year follow-up period.
Materials and methods
Study population
This study was reviewed and approved by the review board of the First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China, and exemption for informed consent was obtained from the Investigational Ethical Review Board. The study was conducted in compliance with the provisions of the Declaration of Helsinki and EN 540.
Selection of the IT or PFNA-II was based on the surgeon’s preference and the availability of the device. The choice of intervention was limited to an IT or PFNA-II device. The choice of equipment size was based on the condition of the femur. The number and combination of screws were the same in each group. All procedures were performed at a single institution. Dual-energy X-ray absorptiometry of the femoral neck was performed preoperatively in all patients. Osteoporosis was defined as a bone mineral density T-score of ≤ −2.5 at the femoral neck.
The inclusion criteria were a freshly closed IFF (AO/OTA Type 3.1A1.1-A2.3), age of 60 to 88 years, a history of primary osteoporosis, the ability to walk independently without aids or with auxiliary equipment before the fracture, and a fixation device including only an intramedullary nail (IT or PFNA-II) but no absorbable screw or steel wire. The exclusion criteria were insufficient follow-up (<3 years), bone-active medication use, an open IFF, multiple IFFs or multiple traumatic injuries, developmental dysplasia of the hip, arthrosis/arthritis, any diseases affecting bone metabolism, a bed ridden status, the need for auxiliary equipment or the help of another person to walk, severe concomitant medical conditions (American Society of Anesthesiologists [ASA] score of V), cognitive dysfunction, malabsorption syndrome, mental illness, hypercalcemia, hypocalcemia, unreliability for follow-up, and a history of alcohol (>3 units) or drug abuse. Based on these inclusion and exclusion criteria, 243 patients with osteoporosis and IFFs treated with an IT or PFNA-II (IT: diameter: lag screw, 11 mm; compression screw, 7 mm; composite screw, 15.5 mm; length, normal; number of proximal/distal screws, 2/1; PFNA-II: proximal diameter, 16.5 mm; distal diameter, 9–10 mm; length, 240 or 300 mm; number of proximal/distal screws, 1/1; valgus curvature, 5°) were enrolled in this study from January 2009 to March 2012.
The patients’ baseline data, including sex, age, body mass index, fractured side, injury mechanism, AO/OTA fracture type, ASA classification, injury–operation interval, and follow-up time, are presented in Table 1.
Table 1.
Patient demographics and outcomes.
| Variable | ITa (n = 86) | PFNA-IIb (n = 88) | P-value |
|---|---|---|---|
| Sex, male/female | 30/56 | 34/54 | 0.608* |
| Age, years | 72.7 ± 7.6 | 74.6 ± 6.3 | 0.071* |
| BMI, kg/m2 | 26.7 ± 8.0 | 24.8 ± 7.7 | 0.122* |
| BMD | −4.0 ± 0.9 | −4.1 ± 0.8 | 0.202 |
| Side, left/right | 40/46 | 42/46 | 0.872* |
| Injury mechanism | 0.595* | ||
| Low-energy trauma | 44 | 42 | |
| Fall from height | 10 | 15 | |
| Vehicular accident | 32 | 31 | |
| AO/OTA fracture type | 0.955* | ||
| 31A1.1 | 14 | 14 | |
| 31A1.2 | 13 | 17 | |
| 31A1.3 | 10 | 11 | |
| 31A2.1 | 19 | 16 | |
| 31A2.2 | 16 | 18 | |
| 31A2.3 | 14 | 12 | |
| ASA classification | 0.830* | ||
| ASA 1 | 22 | 27 | |
| ASA 2 | 36 | 32 | |
| ASA 3 | 19 | 21 | |
| ASA 4 | 9 | 8 | |
| Injury–operation interval | 0.942* | ||
| <24 h | 16 | 14 | |
| 24–48 h | 36 | 38 | |
| 48–72 h | 24 | 27 | |
| >72 h | 10 | 9 | |
| Follow-up, months | 40.84 ± 2.73 | 41.51 ± 2.24 | 0.076* |
Data are presented as n or mean ± standard deviation.
No statistically significant values.
IT: INTERTAN nail; PFNA-II: proximal femoral nail antirotation-Asia; HHS: Harris hip score; ASA: American Society of Anesthesiologists; BMI: body mass index; BMD: bone mineral density; aSmith & Nephew, Memphis, TN; bSynthes, Solothurn, Switzerland.
Surgery and rehabilitation
All patients received antithrombotic prophylaxis perioperatively, an intravenous injection of cefazolin sodium pentahydrate (2.0 g) 30 minutes preoperatively, and spinal anesthesia. All operations were performed in our institution by four orthopedic surgeons. The surgical procedures were performed according to the standard protocols for either IT or PFNA-II, as recommended by the device manufacturers and described previously by Ruecker et al.15 for the IT and Mereddy et al.16 for the PFNA-II. Too-anterior hip screw placement was avoided. Intraoperative reduction of the neck shaft angle to a valgus position of 5° to 10° relative to the contralateral side was achieved. The tip–apex distance (TAD) as an important predictor of cut-out following extramedullary and intramedullary stabilization of IFFs was limited to about 20 mm (range, 18–22 mm) because a TAD of >25 mm was associated with an increased risk of cut-out or implant failure in stable or unstable IFFs. Closed reduction of fractures was performed under fluoroscopic guidance. Two implants were inserted without reaming of the medullary canal or drilling, and no nails were hammered into the marrow cavity. Distal interlocking of the PFNA-II was performed in a static manner with two screws in the PFNA-II group. No bone grafts, bone void filler, or suction drains were used in any patients. All incisions were closed in layers. The transfusion criterion was a hemoglobin concentration of <8 g/dl.
The postoperative rehabilitation protocol was equivalent in both groups. A low-molecular-weight heparin sodium injection (enoxaparin [Clexane] 4000 aXa IU; Shanghai, China) was administered to all patients once a day beginning on the day of admission and continuing for 7 subsequent days, and all patients received a prophylactic antibiotic (cefazolin sodium pentahydrate, 2.0 g) twice a day beginning the day before surgery and continuing for 3 subsequent days. When the patient was capable, continuous passive motion (Smith & Nephew, Shanghai, China) was administered by a physiotherapist three times a day beginning the first day postoperatively. Plain radiographs (anteroposterior and lateral projections) were assessed on the first postoperative day to check fracture reduction and implant position. The weight-bearing protocol was uniform for all of the patients. One week postoperatively, patients were allowed to engage in out-of-bed activities with axillary crutches. Two weeks postoperatively, the patients were encouraged to perform toe-touch weight-bearing ambulation. Six weeks postoperatively, the patients were permitted to ambulate with partial weight bearing. Once healing of the femoral fracture was confirmed by X-ray, full weight-bearing ambulation was required.
Twelve months postoperatively, the implant was removed in each patient. The procedure (anesthesia, surgery, wound care, etc.) was essentially the same. Three days postoperatively, the patients were encouraged to engage in partial weight-bearing ambulation. All of the patients were discharged with full weight-bearing ambulation approximately 7 days (5–8 days) after surgery.
Method of assessment
Follow-up visits occurred at 1, 3, 6, 9, and 12 months postoperatively and every year thereafter. Plain radiographic outcomes (anteroposterior and lateral projections) were obtained at each visit. Major changes in the implant position, major orthopedic complications (complications related to fixation), and fixation failures were noted. No missing data were observed throughout the follow-up period. Each evaluation was performed by a radiologist with no knowledge of the treatment or subjective or clinical outcomes of the patients.
The patient-related functional outcomes were evaluated based on the Harris hip score (HHS). The HHS was considered excellent (90–100), good (80–89), fair (70–79), or poor (<70).17 The primary outcome was the radiographic outcome. The secondary outcome was the functional outcome. The tertiary outcome was pain. Union was defined as clear demonstration of bone bridging across the fracture on radiographs with the ability to bear full weight on the extremity and evidence of clinical healing (i.e., return to prefracture mobility with no pain on palpation). Using this protocol, however, it was impossible to know when exactly the union had occurred in each patient. Nonunion was defined as the lack of union after 6 months of follow-up. Implant failure was defined as any condition that would necessitate revision surgery with a change of implant. The screw position was chosen centrally in the femoral head with a TAD of <25 mm.18 The TAD was determined by measuring the distance from the tip of the lag screw to the apex of the femoral head on both anteroposterior and lateral radiographs.19
Data analysis
Statistical analyses were performed using SPSS version 22.0.0 statistical software (IBM Corp., Armonk, NY). All continuous data are expressed as mean ± standard deviation (SD). Quantitative variables were analyzed using Student’s t-test, and categorical variables were analyzed by the chi-square test or Fisher’s exact test as appropriate. All tests were two-tailed. The level of significance was set at P < 0.05 for all statistical analyses.
Results
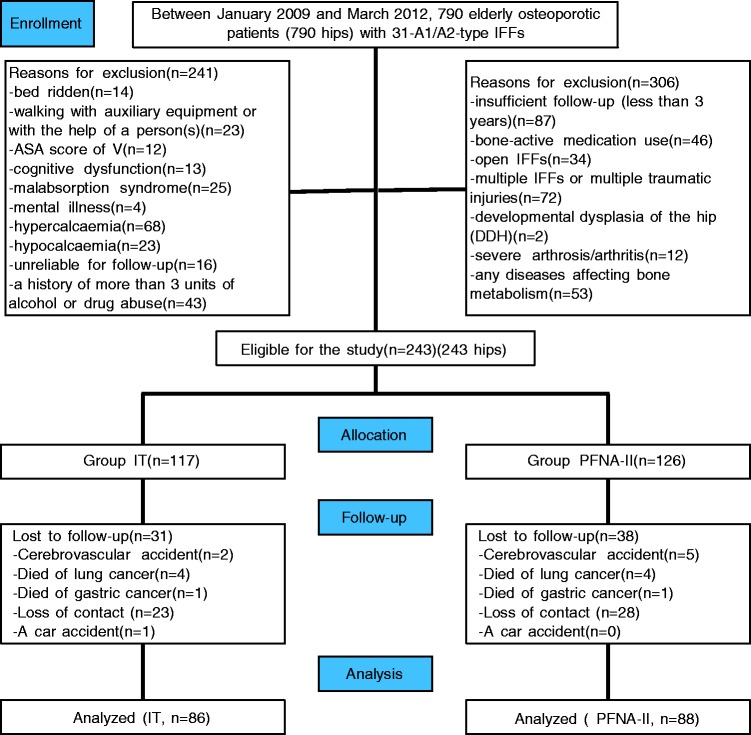
Approximately 28.4% of the patients (n = 69) were not available for follow-up because of death (n = 17; 7 due to cerebrovascular accident, 8 due to lung cancer, and 2 due to gastric cancer), a car accident (n = 1), or loss of contact (n = 51). Thus, 174 patients (174 hips) (IT, n = 86; PFNA-II, n = 88) were included in the final analysis. These patients had a mean age of 73 years (range, 60–88 years) and were followed up for an average of 40 months (range, 38–60 months) (Figure 1). Of the 174 primary procedures, most were performed in patients with an ASA grade of ≤ 2 (IT, n = 58, 67.4%; PFNA-II, n = 59, 67.0%), injury–operation interval of ≤ 72 h (IT, n = 76, 88.4%; PFNA-II, n = 79, 89.8%), ASA grade of ≤3 (IT, n = 77, 89.5%; PFNA-II, n = 80, 90.9%), and stable IFFs (31A1.1-2.1) (IT, n = 56, 65.1%; PFNA-II, n = 58, 65.9%). The most common injury mechanisms were low-energy trauma and vehicular accidents (IT, n = 72, 83.7%; PFNA-II, n = 73, 83.0%). Most surgical operations were completed in <2 hours. In all cases, calculation of the HHS, performance of the anteroposterior and lateral projections, and the physical examination were conducted by medium- or high-volume surgeons throughout the follow-up period in our hospital. The baseline data, which are shown in Table 1 and Table 2, were similar between the two groups.
Figure 1.
Flow diagram demonstrating methods for identification of studies to assess the treatment of osteoporotic intertrochanteric femur fractures (AO/OTA Type 3.1A1.1-A2.3) in the elderly using either the InterTAN nail (IT) or proximal femoral nail anti-rotation-Asia (PFNA-II) systems, and reasons for exclusion.
Table 2.
Operative variables.
| Variable | ITa (n = 86) | PFNA-IIb (n = 88) | P-value |
|---|---|---|---|
| Implant position | 0.567* | ||
| Optimal | 69 | 67 | |
| Suboptimal | 17 | 21 | |
| TAD, mm | 25.86 ± 0.98 | 26.00 ± 1.16 | 0.393* |
Data are presented as n or mean ± standard deviation.
No statistically significant values.
TAD: tip–apex distance; IT: INTERTAN nail; PFNA-II: proximal femoral nail antirotation-Asia; aSmith & Nephew, Memphis, TN; bSynthes, Solothurn, Switzerland
Functional outcomes
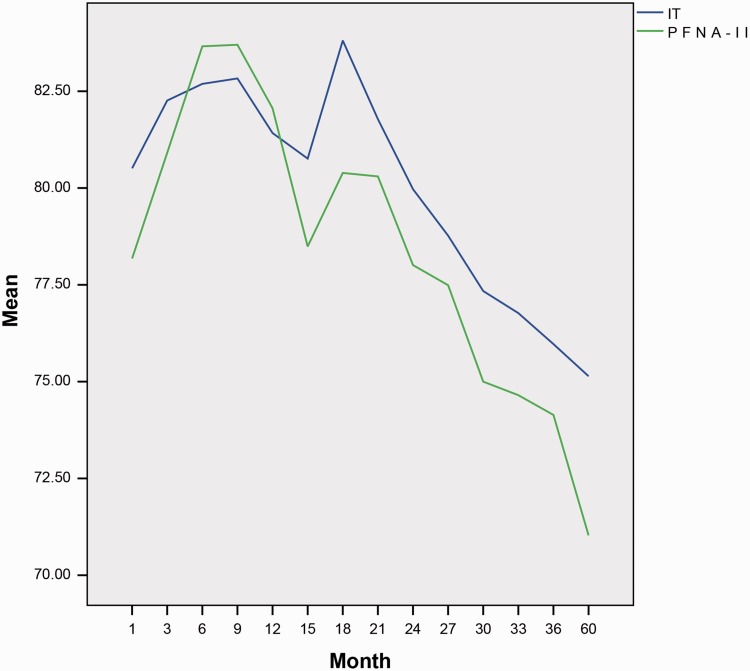
Functional outcome scores were obtained for all patients. The HHS was used to assess the functional outcome of the patients. More than 77% of the patients with osteoporosis and IFFs (AO/OTA Type 3.1A1.1-A2.3) had satisfactory functional scores at the final follow-up: 24 had excellent scores, 21 had good scores, 90 had fair scores, and 39 had poor scores. There was a significant difference between the two groups at each follow-up. At 1 and 3 months postoperatively, the HHS was greater in the IT than PFNA-II group. At 6, 9, and 12 months postoperatively, the HHS was greater in the PFNA-II than IT group. From 15 months postoperatively to the final follow-up, the HHS was consistently greater in the IT than PFNA-II group (Table 3). The law curve of the HHS changes is shown in Figure 2.
Table 3.
Long-term functional outcomes.
| Harris hip score | ITa (n = 86) | PFNA-IIb (n = 88) | P-value |
|---|---|---|---|
| 1 month postoperatively | 80.51 ± 2.91 | 78.18 ± 3.74 | 0.000* |
| 3 months postoperatively | 82.26 ± 3.02 | 80.91 ± 3.54 | 0.008* |
| 6 months postoperatively | 82.69 ± 2.93 | 83.66 ± 2.75 | 0.025* |
| 9 months postoperatively | 82.83 ± 2.79 | 83.70 ± 2.72 | 0.037* |
| 12 months postoperatively | 81.42 ± 1.78 | 82.06 ± 2.12 | 0.033* |
| 15 months postoperatively | 80.76 ± 3.43 | 78.49 ± 3.33 | 0.000* |
| 18 months postoperatively | 83.81 ± 4.38 | 80.39 ± 3.70 | 0.000* |
| 21 months postoperatively | 81.78 ± 3.85 | 80.30 ± 4.51 | 0.021* |
| 24 months postoperatively | 79.97 ± 3.60 | 78.01 ± 3.72 | 0.001* |
| 27 months postoperatively | 78.77 ± 3.41 | 77.49 ± 3.45 | 0.015* |
| 30 months postoperatively | 77.34 ± 2.97 | 75.00 ± 2.58 | 0.000* |
| 33 months postoperatively | 76.77 ± 2.89 | 74.65 ± 3.08 | 0.000* |
| 36 months postoperatively | 75.97 ± 2.30 | 74.14 ± 2.56 | 0.000* |
| Final follow-up | 75.14 ± 3.65 | 71.03 ± 3.54 | 0.000* |
Data are presented as mean ± standard deviation.
Statistically significant values.
IT: INTERTAN nail; PFNA-II: proximal femoral nail antirotation-Asia; aSmith & Nephew, Memphis, TN; bSynthes, Solothurn, Switzerland
Figure 2.
Law curve of changes in the Harris hip score in the two groups. IT, INTERTAN nail; PFNA-II, proximal femoral nail antirotation-Asia.
A total of 24% of patients in the PFNA-II group described some level of hip pain in the resting state, and this proportion increased to 43% in the active state. Severe pain is often observed in PFNA-II-treated patients. A total of 18% of patients in the IT group reported no or mild hip pain in the resting state, and this figure increased to 38% in the active state. Nevertheless, no statistically significant difference in the mean pain score between the two groups was noted at each follow-up point.
Radiographic outcomes
The major radiographic outcomes in this study were screw cut-out, which can be adjusted and repaired; prosthetic instability; periprosthetic fracture; lateral cortex fracture; femoral shaft fracture after implant removal; delayed union; malunion or nonunion; migration of the proximal screw(s); femoral head offset; lower limb shortening (>1.5 cm); implant failure, which cannot be adjusted or repaired; and the need for a new implant. The mean TAD was 20.2 mm (range, 16.0–24.6 mm; SD, 1.4 mm) in the PFNA-II group and 19.0 mm (range, 17.0–22.0 mm; SD, 1.6 mm) in the IT group. The number of implant failures was zero in the IT group and six in the PFNA-II group. Six of 88 (6.8%) patients in the PFNA-II group displayed evidence of implant failure at the final follow-up; 4 patients had screw cut-out, which cannot be adjusted or repaired, and 2 were experiencing unbearable pain due to an unstable fracture (AO/OTA Type 31A2.2 and A2.3) with medial calcar damage, without bone grafting during the operation. Revision surgery was performed as quickly as possible, without waiting for the situation to further deteriorate. During the second operation, bone grafting was applied for these patients, and bone union was observed 5 to 7 months postoperatively. These cases were considered implant failures and did not affect any other observation in the study. Significant differences were also observed with regard to lateral cortex fracture (IT, n = 0 vs. PFNA-II, n = 7; P = 0.022) and femoral shaft fracture after implant removal (IT, n = 1 vs. PFNA-II, n = 8; P = 0.044). There were no other significant differences in the remaining observation indices between the two groups (Table 4).
Table 4.
Long-term radiographic outcomes.
| Variable | ITa (n = 86) | PFNA-IIb (n = 88) | P-value |
|---|---|---|---|
| Screw cut-out | 1 | 2 | 1.000 |
| Prosthetic instability | 1 | 1 | 0.990 |
| Periprosthetic fracture | 0 | 1 | 1.000 |
| Lateral cortex fracture | 0 | 7 | 0.022* |
| Femoral shaft fracture after implant removal | 1 | 8 | 0.044* |
| Delayed union | 0 | 1 | 1.000 |
| Malunion | 2 | 0 | 0.243 |
| Nonunion | 1 | 1 | 0.990 |
| Migration of proximal screw(s) | 0 | 1 | 1.000 |
| Femoral head offset | 3 | 1 | 0.597 |
| Lower limb shortening (>1.5 cm) | 1 | 2 | 1.000 |
| Complications of distal interlocking | 0 | 1 | 1.000 |
| Heterotopic ossification | 1 | 1 | 0.990 |
| Avascular necrosis of the femoral head | 0 | 0 | 1.000 |
| Implant failure | 0 | 6 | 0.040* |
Data are presented as n.
Statistically significant values.
IT: INTERTAN nail; PFNA-II: proximal femoral nail anti-rotation-Asia; aSmith & Nephew, Memphis, TN; bSynthes, Solothurn, Switzerland
Discussion
The 3-year minimum follow-up results of this study revealed a trend toward a better postoperative HHS, less pain, and fewer radiographic complications in the two groups. More than 77% of the patients with osteoporosis and IFFs (AO/OTA Type 3.1A1.1-A2.3) had satisfactory functional scores and few or no significant radiographic complications. However, the marked functional benefit afforded by IT over PFNA-II in the initial 3 months was no longer present at 6, 9, and 12 months postoperatively. From 15 months postoperatively until the final follow-up, IT-treated patients had a higher HHS score than those PFNA-II-treated patients. However, we suspect that the small sample size of elderly patients with osteoporosis contributed to this finding. This effect may have also resulted from the increased comorbidities in these patients rather than any deterioration of the ITs because no patients in the IT group described any significant symptoms related to their affected limbs during follow-up. In addition, elderly patients with osteoporosis are more prone to screw movement or cutting of screws into the femoral head, which can result in fixation failure. Rigid fixation is critical for minimizing interfragmentary motion and maintaining fracture reduction under load.8 However, whether we need to strengthen the fixation (rigid fixation) is unclear because we have often found that one or more of the screws is loosened when implementing rigid fixation. Osteoporosis may also lead to technical problems during the procedure. We may be simultaneously creating a weak point around the fracture line and further destroying the bone (microfracture), thereby increasing the risk of refracture. Surgeons should carefully consider whether to ensure that all of the screws are tightened or whether a less tight, but “stable-enough” construct is sufficient to hold the pieces together. In this study, six patients in the PFNA-II group underwent conversion to total hip replacement because of implant failures in four (screw cut-out, AO/OTA Type 31A2.2 and A2.3) and unbearable pain possibly caused by an ongoing microfracture in two. Moreover, consistent with previous reports, the current study revealed a higher revision rate (6.8%) for patients in the PFNA-II group. Numerous prospective randomized clinical studies comparing IT with PFNA-II have shown that PFNA-II is associated with a high rate of reoperations and an increased incidence of femoral shaft fractures after implant removal.20–22 This was further confirmed in a meta-analysis by Ma et al.,23 who found a reoperation rate of 17.7%.
In the present study, the PFNA-II group exhibited a higher rate (9.1%) of femoral shaft fractures after implant removal. This result is in contrast to that reported by Aktselis et al.,24 who found similar between-group rates (15.5%) after a 1-year follow-up. Tang et al.25 also reported a lower rate (12.3%) after a 2-year follow-up. These rates differ from two other studies that reported rates of 18.9%6 and 19.5%,26 respectively. However, they are within the range reported by Chen et al.,27 whose results were confirmed by analysis of fracture line loading using an in vitro biomechanical test.
The potential advantages of the IT over the PFNA-II in treating IFFs remain controversial.1,2,5 The decision regarding whether an implant is superior to another should be based on its long-term efficacy rather than on its intraoperative or short-term postoperative outcome. When an IFF occurs and an implant is applied, the occurrence of a decisive difference in outcome cannot be automatically evaluated based on factors such as the operation time, length of stay, blood loss, fluoroscopy time, or short-term pain because numerous subjective and objective factors influence these parameters. Furthermore, as we have previously reported, there are few significant differences in these parameters between the IT and PFNA-II after short-term follow-up.1 In the present study, we chose to focus on major long-term factors to minimize confusion that might be created by including short-term indicators. In addition, inclusion of such indicators would have no important implications for treatment.
Zhang et al.2 evaluated the HHS at 1, 3, 6, 9, and 12 months postoperatively after treatment with the IT or PFNA-II. Although the findings from the intermediate months could not be explained at the 1-year follow-up, no significant differences in the return to prefracture ambulatory levels and independence were observed between the two groups. Thus, the authors concluded that the IT offered no advantage over the PFNA-II in the management of IFFs (AO/OTA Type 3.1A1.1-A2.3). Another study3 comparing the HHS 1 year after IT versus PFNA-II fixation revealed no between-group differences in the HHS. A meta-analysis comparing the IT with the PFNA-II confirmed no between-group differences in the postoperative HHS. In the present study, patients in the PFNA-II group had a significant reduction in the HHS from 15 months postoperatively to the final follow-up. However, no such loss of function appeared in the IT group, unlike in the study by Seyhan et al.3 Ruecker et al.15 concluded that the IT yielded faster recovery of function. Sciacca et al.4 demonstrated similar progress in hip strength and mobility in the first 3 months postoperatively in the IT group. Moreover, significant differences favoring the IT group were again observed 12 months after surgery and continued until the final follow-up, which is consistent with our findings. Contrary to our findings, however, Kim et al.9 found no differences in the postoperative HHS at the 3-month postoperative follow-up despite the fact that they followed their elderly patients for 1 year and had the additional benefit of different scores. The finding that the HHS is markedly poorer after PFNA-II than IT fixation in the first 3 months postoperatively is key because elderly patients require a more rapid return to the prefracture level. Similar findings have been reported by Seyhan et al.3 and Sciacca et al.4 In contrast, Liu et al.28 concluded that elderly patients with osteoporosis who underwent PFNA-II fixation achieved better outcomes in the initial 3 months. Eventually, however, there were parallel outcomes of functional recovery at the final follow-up. The value of this finding in elderly patients with osteoporosis is relative. There were more mechanical complications in the PFNA-II group, such as failure, loosening, and breakage of the implant, although the difference was not statistically significant. In summary, regardless of the similarity in the final HHS, the most significant finding was that elderly patients with osteoporosis undergoing IT fixation exhibited functional recovery as early as 3 months postoperatively, in contrast to the PFNA-II-treated patients. In practice, this finding implies that IT fixation tends to achieve faster functional recovery than PFNA-II fixation.
In the present study, seven lateral cortex fractures were observed during follow-up in the PFNA-II group (AO/OTA Type 31A1.3 in three patients and AO/OTA Type 31A2.1 in four patients). No patients in the IT group developed lateral cortex fractures. Although the lateral cortex is very delicate and susceptible to fracture during surgery, fractures in the present study tended to occur in the initial 3 months in the PFNA-II group. Furthermore, although the PFNA-II bypasses the lateral wall and acts as a prosthetic lateral cortex medial to the broken lateral wall, it has a weaker compression and antitorsion capacity of the fracture line and is less effective in resisting vertical and longitudinal displacement compared with the IT.8
Long or overlength nails are commonly used to manage IFFs caused by primary or metastatic tumors and are less commonly used in cases of trauma. Nevertheless, in elderly patients with osteoporosis who develop IFFs, a long or long-length PFNA-II should be considered. Consistent with our findings, previous studies6,28,29 have shown that implants have reliable outcomes when long PFNA-II are used to treat IFFs. In the PFNA-II group of the current study, 25 (75.8%) orthopedic complications occurred in association with the 240-cm-long nail compared with 8 (24.2%) in association with the 300-cm-long nail.
Despite our consistent findings among different orthopedic departments, there are several limitations to our study. First, the small sample size may have introduced bias. However, the focus of our study was to assess the 3-year minimum follow-up functional and radiographic outcomes of the IT and PFNA-II in the management of IFFs (AO/OTA Type 3.1A1.1-A2.3) in elderly patients with osteoporosis, an area that has not been studied extensively in the literature. Despite the small sample size, it was still possible to detect statistically significant differences. Second, this study had problems inherent to its retrospective nature, including nonrandomization. Third, patient- and surgeon-related confounders may have existed. Finally, because of the observational nature of this study, we may not have addressed all potential confounding variables in our analyses. Nevertheless, this study provides preliminary objective evidence about the effect of fracture patterns with the use of two nails. Despite these limitations, this analysis presents long-term follow-up results and is the first to evaluate covariates that may impact the clinical outcome of patients undergoing fixation with the IT or PFNA-II.
In conclusion, the short-term outcomes of the PFNA-II for IFFs (AO/OTA Type 3.1A1.1-A2.3) may be superior to those of the IT, but this is not true in the initial 3 months or after 15 months in independent elderly patients with osteoporosis. Femoral shaft fracture after implant removal, implant failure, and lateral cortex fracture remain the major complications associated with the PFNA-II, although the application of longer nails may decrease this incidence.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Yu W, Zhang X, Zhu X, et al. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J Orthop Surg Res 2016; 11: 10–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang S, Zhang K, Jia Y, et al. InterTan nail versus proximal femoral nail antirotation-asia in the treatment of unstable trochanteric fractures. Orthopedics 2013; 36: e288–e294. [DOI] [PubMed] [Google Scholar]
- 3.Seyhan M, Turkmen I, Unay K, et al. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci 2015; 20: 1053–1061. [DOI] [PubMed] [Google Scholar]
- 4.Sciacca S, Lidder SS, Grechenig C, et al. Variations of treatment in selected proximal femur fractures among surgeons with different surgical experience-A survey at an international AO course. Injury 2015; 46(Suppl 6): S57–S60. [DOI] [PubMed] [Google Scholar]
- 5.Matre K, Vinje T, Havelin LI, et al. TRIGEN INTERTAN Intramedullary nail versus sliding hip screw a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am 2013; 95: 200–208. [DOI] [PubMed] [Google Scholar]
- 6.Li M, Wu L, Liu Y, et al. Clinical evaluation of the Asian proximal femur intramedullary nail antirotation system (PFNA-II) for treatment of intertrochanteric fractures. J Orthop Surg Res 2014; 9: 112–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Werner BC, Fashandi AH, Gwathmey FW, et al. Trends in the management of intertrochanteric femur fractures in the United States 2005–2011. Hip Int 2015; 25: 270–276. [DOI] [PubMed]
- 8.Huang Y, Zhang C, Luo Y. A comparative biomechanical study of proximal femoral nail (InterTAN) and proximal femoral nail antirotation for intertrochanteric fractures. Int Orthop 2013; 37: 2465–2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim J-W, Kim T-Y, Ha Y-C, et al. Outcome of intertrochanteric fractures treated by intramedullary nail with two integrated lag screws a study in Asian population. Indian J Orthop 2015; 49: 436–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tella SH, Gallagher JC. Prevention and treatment of postmenopausal osteoporosis. J Steroid Biochem Mol Biol 2014; 142: 155–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shayesteh-Azar M, Karimi-Nasab MH, Sajjadi-Saravi M, et al. Comparison of surgical complications of intertrochanteric hip fractures between non-osteoporotic and osteoporotic patients. J Pak Med Assoc 2013; 63: 752–755. [PubMed] [Google Scholar]
- 12.Tasyikan L, Ugutmen E, Sanel S, et al. Short-term results of surgical treatment with cephalomedullary nails for basicervical proximal femoral fractures. Acta Orthop Belg 2015; 81: 427–434. [PubMed] [Google Scholar]
- 13.Makki D, Matar HE, Jacob N, et al. Comparison of the reconstruction trochanteric antigrade nail (TAN) with the proximal femoral nail antirotation (PFNA) in the management of reverse oblique intertrochanteric hip fractures. Injury 2015; 46: 2389–2393. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Cheng L, Jing J. The Asia proximal femoral nail antirotation versus the standard proximal femoral antirotation nail for unstable intertrochanteric fractures in elderly Chinese patients. Orthop Traumatol Surg Res 2015; 101: 143–146. [DOI] [PubMed] [Google Scholar]
- 15.Ruecker AH, Rupprecht M, Gruber M, et al. The treatment of intertrochanteric fractures: results using an intramedullary nail with integrated cephalocervical screws and linear compression. J Orthop Trauma 2009; 23: 22–30. [DOI] [PubMed] [Google Scholar]
- 16.Mereddy P, Kamath S, Ramakrishnan M, et al. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for the treatment of unstable proximal femoral fractures. Injury 2009; 40: 428–432. [DOI] [PubMed] [Google Scholar]
- 17.Paul O, Barker JU, Lane JM, et al. Functional and radiographic outcomes of intertrochanteric hip fractures treated with calcar reduction, compression, and trochanteric entry nailing. J Orthop Trauma 2012; 26: 148–154. [DOI] [PubMed] [Google Scholar]
- 18.Kashigar A, Vincent A, Gunton MJ, et al. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J 2014; 96–B: 1029–1034. [DOI] [PubMed] [Google Scholar]
- 19.Geller JA, Saifi C, Morrison TA, et al. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop 2010; 34: 719–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peskun C, McKee M, Kreder H, et al. Functional outcome of ipsilateral intertrochanteric and femoral shaft fractures. J Orthop Trauma 2008; 22: 102–106. [DOI] [PubMed] [Google Scholar]
- 21.Huny SH, Hsu CY, Hsu SF, et al. Surgical treatment for ipsilateral fractures of the hip and femoral shaft. Injury 2004; 35: 165–169. [DOI] [PubMed] [Google Scholar]
- 22.Niu E, Yang A, Harris AHS, et al. Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the united states? A survey of orthopaedic surgeons. Clin Orthop Relat Res 2015; 473: 3647–3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma KL, Wang X, Luan FJ, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res 2014; 100: 859–866. [DOI] [PubMed] [Google Scholar]
- 24.Aktselis I, Kokoroghiannis C, Fragkomichalos E, et al. Prospective randomised controlled trial of an intramedullary nail versus a sliding hip screw for intertrochanteric fractures of the femur. Int Orthop 2014; 38: 155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang P, Hu F, Shen J, et al. Proximal femoral nail antirotation versus hemiarthroplasty: a study for the treatment of intertrochanteric fractures. Injury 2012; 43: 876–881. [DOI] [PubMed] [Google Scholar]
- 26.Guerra MT, Pasqualin S, Souza MP, et al. Functional recovery of elderly patients with surgically-treated intertrochanteric fractures: preliminary results of a randomised trial comparing the dynamic hip screw and proximal femoral nail techniques. Injury 2014; 45(Suppl 5): S26–S31. [DOI] [PubMed] [Google Scholar]
- 27.Chen Y, Liu S, Lin P, et al. Comparative biomechanical study of reversed less invasive stabilization system and proximal femoral nail antirotation for unstable intertrochanteric fractures. Chinese Med J (Engl) 2014; 127: 4124–4129. [PubMed] [Google Scholar]
- 28.Liu JJ, Shan LC, Deng BY, et al. Reason and treatment of failure of proximal femoral nail antirotation internal fixation for femoral intertrochanteric fractures of senile patients. Genet Mol Res 2014; 13: 5949–5956. [DOI] [PubMed] [Google Scholar]
- 29.Chang SM, Song DL, Ma Z, et al. Mismatch of the short straight Cephalomedullary Nail (PFNA-II) with the anterior bow of the femur in an asian population. J Orthop Trauma 2014; 28: 17–22. [DOI] [PubMed] [Google Scholar]