Abstract
Type 2 diabetes mellitus (T2DM) has shown to be associated with higher incidence of sleep disorders, which may be due to disease itself or because of secondary complications or associated comorbidities associated with diabetes. On the other hand, shorter sleep duration and erratic sleep behavior itself have been linked with higher incidence of obesity, metabolic syndrome, and T2DM. Assessment of sleep quality and sleep disorders as a part of the comprehensive medical evaluation is recommended based on emerging evidence suggesting a relationship between sleep quality and glycemic control in persons with T2DM. In this review, we attempt to summarize common sleep disorders associated with T2DM, their impacts on glycemic and other metabolic control, and various preventive and therapeutic strategies to tackle these problems.
Keywords: Metabolic syndrome, obstructive sleep apnea, sleep-disordered breathing, sleep disorders, type 2 diabetes
INTRODUCTION
Type 2 diabetes mellitus (T2DM) and sleep disturbances both are common health problems and detrimental to the each other. Sleep disturbances are common among individuals with diabetes. Persons with diabetes report higher rates of insomnia, poor sleep quality, excessive daytime sleepiness, and higher use of sleeping medications.[1] Sleep disturbances may be due to the disease itself or due to physical complications of disease such as peripheral neuropathy and polyuria. Assessment of sleep quality and sleep disorders is of paramount importance in persons with T2DM.[2]
On the other hand, sleep curtailment as well as erratic sleep behavior as a result of lifestyle choices, which is part and parcel of modern society, has been itself linked with higher risk of obesity, metabolic syndrome, and T2DM.[3]
PHYSIOLOGY OF SLEEP
Sleep is a complex behavioral and physiologic process and divided into rapid eye movement (REM) sleep and non-REM sleep. Although generally viewed as a passive condition, it is highly active and dynamic process. The later stages of non-REM sleep, Stages 3 and 4, also known as slow-wave sleep are most refreshing and restorative. Sleep is important not only for restoring brain functions but it also modulates a variety of metabolic, endocrine, and cardiovascular systems. Normally, during non-REM sleep, there is decrease in metabolic rate, sympathetic nervous system activity, blood pressure, and heart rate and increase in cardiac vagal activity.[4] However, this sleep physiology is disrupted in persons with sleep disorders including obstructive sleep apnea (OSA).[5]
DIABETES AND SLEEP DISTURBANCES
Sleep disorders are significantly more common in persons with diabetes as compared to those without diabetes. Multiple factors may contribute to insomnia in persons with diabetes including discomfort or pain associated with peripheral neuropathy, restless legs syndrome, periodic limb movements, rapid changes in blood glucose levels during night leading to hypoglycemic and hyperglycemic episodes, nocturia and associated depression.[6] Individuals with diabetes have a significantly increased risk of developing depression when compared to their nondiabetic counterparts and depression is one of the important factors contributing to poor sleep in this population. Furthermore, diabetes itself has multiple impacts on central nervous system causing alterations involving neurobehavioral and neurotransmitter functioning and autonomic functions, and can adversely affect endocrine functions, and hence itself cause sleep disturbances.[7]
SLEEP DISTURBANCES AND RISK OF OBESITY AND TYPE 2 DIABETES MELLITUS
Epidemiological data have suggested higher risk of obesity and T2DM in individuals with shorter sleep duration (<5–6 h/night) as well as those of poor sleep quality. Studies have also reported higher risk of obesity and T2DM in individuals with long sleep duration (≥9 h/day) also. The categories of sleep disturbances that contribute to obesity and T2DM include the following: (1) alterations of sleep duration, chronic sleep restriction, and excessive sleep; (2) alterations in sleep architecture; (3) sleep fragmentation; (4) circadian rhythm disorders and disruption (i.e., shift work); and (5) OSA.[3]
A recent systematic review and meta-analysis demonstrated sleep disturbances as significant risk factors for diabetes with effect sizes similar to those imparted by traditional risk factors. After adjustment for confounders, the risk of developing diabetes due to OSA, difficulty maintaining or initiating sleep was slightly less than the risk of having a family history of diabetes but greater than that of being physically inactive. Difficulty initiating sleep increased the risk of T2DM by 55%, while difficulty maintaining sleep increased its risk by 74%. Similarly, the risk of developing T2DM associated with insufficient (≤5 h/day) or excessive sleep duration (≥9 h/day) or performing shift work was comparable to that of being physically inactive. The authors concluded that sleep disturbances should therefore be systematically considered in guidelines for the screening as well as while making preventive strategies for T2DM.[8]
MECHANISM OF OBESITY AND GLYCEMIC DYSREGULATION WITH SLEEP DISTURBANCES
Sleep disturbance are associated with dysregulation of the neuroendocrine control of appetite. One of the important mechanisms linking weight gain with sleep deprivation is likely hyperactivity of orexin system. Orexin system is overactive during sleep deprivation which along with over activity of sympathetic nervous system leads to overfeeding. Furthermore, there is increase in circulating levels of ghrelin, hunger-promoting hormone as well a decrease in leptin, which is a satiety factor.[9]
VanHelder et al. showed that the insulin response to an oral glucose challenge was higher when comparing the total sleep deprivation condition to the normal sleep condition, suggesting an insulin resistant state that is induced by acute sleep deprivation.[10] Another study reported that a 1-week period of sleep restriction (only 4 h of sleep daily) in young, healthy subjects could produce a prediabetic state.[11] Acute sleep deprivation whether total or partial is associated with an elevation of evening cortisol concentration.[12] Spiegel et al. demonstrated impaired glucose tolerance with chronic sleep deprivation.[13]
Possible causes of impaired glucose metabolism in sleep disordered breathing (SDB) including OSA might be intermittent hypoxia and sleep fragmentation associated with them. Sleep fragmentation increases sympathetic activity, which can increase blood glucose levels by decreasing insulin sensitivity.[14] Furthermore, these episodes of respiratory disturbance may induce frequent arousal episodes and the consequent sleep loss may also facilitate the development of metabolic disturbances.[15]
DIABETES AND SLEEP APNEA
Sleep apneas are significantly more in persons with diabetes and correlate highly with obesity. In fact, a strong association exists between obesity, impaired glucose tolerance, insulin resistance, and SDB. Although OSA is most common type of SDB, central-type apneas and periodic breathing have been reported in patients with autonomic diabetic neuropathy.[16,17]
OSA is a sleep-related breathing disorder characterized by collapse of the upper airway leading to cessation of airflow in the setting of continued respiratory effort. The resultant hypoxia leads to frequent arousals causing sleep fragmentation and symptoms of excessive daytime sleepiness. The prevalence of OSA in the population with type 2 diabetes may be as high as 23%, and the prevalence of any SDB may be as high as 58%.[18] In obese participants enrolled in the Action for Health in Diabetes (Look AHEAD) trial, it exceeded 80%.[19] Common symptoms of OSA include loud snoring, frequent cessation of breathing during sleep, choking and gasping episodes during sleep, waking up sweating during sleep, morning headaches, feeling unfreshed in the morning after apparently adequate night sleep, excessive daytime sleepiness and lethargy, rapid weight gain, and cognitive deficits.[20]
OSA itself has been linked with increased risk of variety of negative health outcomes including endocrine dysfunction, insulin resistance, hypertension, and cardiovascular disease (CVD). One explanation for this overlap is the presence of shared risk factors such as obesity but an increasing number of studies show that these two conditions can be associated independent of obesity. OSA is associated with higher risk of CVD through various mechanisms such as hypoxia and oxidative stress, increased inflammatory markers such as interleukin-6, sympathetic overactivity, and dysregulation of lipid metabolism.[21]
OSA might also be a reason of ineffective treatment of type 2 diabetes. Studies have shown a robust graded relationship between the severity of OSA and poor glycemic control after controlling for the degree of adiposity and multiple other potential confounders.[22] Furthermore, data also support higher risk of development and progression of complications from long-standing T2DM in the setting of inadequately treated OSA. There is some evidence that the treatment of OSA by continuous positive airway pressure might correct some metabolic abnormalities in glucose metabolism; however, the evidence for a treatment effect on glycemic control is mixed.[21] OSA treatment by all means significantly improves quality of life and blood pressure control.[23]
EVALUATION OF SLEEP DISORDERS
Assessment of sleep quality, sleep disorders, and sleep hygiene is of paramount importance in persons with diabetes. In fact, the latest American Diabetes Association 2017 guidelines has specifically added new section and recommend assessment of sleep pattern and duration as part of the comprehensive medical evaluation in persons with diabetes based on emerging evidence suggesting a relationship between sleep quality and glycemic control.[2]
As discussed in previous sections, etiology of sleep disruption in diabetes is often multifactorial. Therefore, a detailed history, careful examination, and handful laboratory investigations will be required for successful evaluation and subsequent treatment of sleep disorders in this population. History should include difficulty falling or staying asleep, excessively sleepy during the day, history of snoring as told by spouse/family members, history of apneic episodes, and history of uncomfortable sensations in the legs in the evening that are relieved by movement. Keeping a sleep diary during the past 2-week period can provide a detailed assessment of sleep patterns. An evaluation for depression by simple clinical tools should be done in all patients. Majority of sleep disorders can be diagnosed with proper history and physical examination. However, when a diagnosis of sleep apnea is suspected, in addition an overnight polysomnogram is required for diagnosis. Once medical and psychiatric causes of insomnia are ruled out, a diagnosis of primary insomnia may be made.
MANAGEMENT OF SLEEP DISORDERS
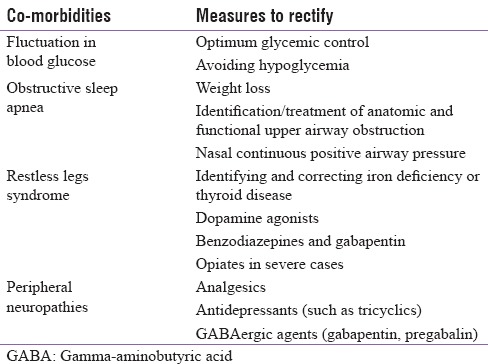
The management of sleep disorders is highly rewarding. Successful management of sleep disorders often requires a multifaceted approach including relief of symptoms and treatment of the common comorbid conditions. Behavioral approaches are very important in the management of insomnia, which include adherence to good sleep hygiene, sleep restriction, cognitive behavioral therapy, and relaxation therapies.[24,25] Some basic dos and don’ts for good sleep hygiene for persons with diabetes are summarized in Table 1. Common measures to rectify common comorbid conditions causing sleep problems in diabetes are summarized in Table 2. Some patients may benefit from pharmacologic therapies such as use of benzodiazepine receptor agonists and the newer hypnotic agents such as zolpidem and zaleplon.
Table 1.
Sleep hygiene - Dos and Don'ts for persons with diabetes
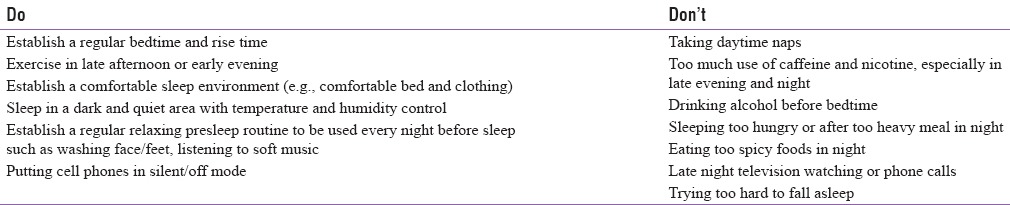
Table 2.
Associated comorbidities contributing to poor sleep in persons with diabetes and possible measures to rectify them
CONCLUSIONS
T2DM and sleep disorders are common problems that often coexist. There is a high prevalence of sleep disorders in people with T2DM which can be detrimental to their health, mood, and quality of life. Conversely, sleep disorders including OSA themselves predispose to higher risk of metabolic disorders including T2DM. All patients with T2DM should be screened for sleep disorders as a part of routine clinical practice and treated appropriately.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Skomro RP, Ludwig S, Salamon E, Kryger MH. Sleep complaints and restless legs syndrome in adult type 2 diabetics. Sleep Med. 2001;2:417–22. doi: 10.1016/s1389-9457(01)00110-1. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Comprehensive medical evaluation and assessment of comorbidities. Diabetes Care. 2017;40(Suppl 1):S25–32. doi: 10.2337/dc17-S006. [DOI] [PubMed] [Google Scholar]
- 3.Koren D, O’Sullivan KL, Mokhlesi B. Metabolic and glycemic sequelae of sleep disturbances in children and adults. Curr Diab Rep. 2015;15:562. doi: 10.1007/s11892-014-0562-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luyster FS, Strollo PJ, Jr, Zee PC, Walsh JK. Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep: A health imperative. Sleep. 2012;35:727–34. doi: 10.5665/sleep.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: A review. Nat Sci Sleep. 2013;5:27–35. doi: 10.2147/NSS.S34838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, et al. Diabetes and sleep disturbances: Findings from the Sleep Heart Health Study. Diabetes Care. 2003;26:702–9. doi: 10.2337/diacare.26.3.702. [DOI] [PubMed] [Google Scholar]
- 7.Mooradian AD. Diabetic complications of the central nervous system. Endocr Rev. 1988;9:346–56. doi: 10.1210/edrv-9-3-346. [DOI] [PubMed] [Google Scholar]
- 8.Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. doi: 10.1016/j.smrv.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.VanHelder T, Symons JD, Radomski MW. Effects of sleep deprivation and exercise on glucose tolerance. Aviat Space Environ Med. 1993;64:487–92. [PubMed] [Google Scholar]
- 11.Van Cauter E, Polonsky KS, Scheen AJ. Roles of circadian rhythmicity and sleep in human glucose regulation. Endocr Rev. 1997;18:716–38. doi: 10.1210/edrv.18.5.0317. [DOI] [PubMed] [Google Scholar]
- 12.Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865–70. [PubMed] [Google Scholar]
- 13.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 14.Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010;137:95–101. doi: 10.1378/chest.09-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Punjabi NM, Polotsky VY. Disorders of glucose metabolism in sleep apnea. J Appl Physiol. 2005;99:1998–2007. doi: 10.1152/japplphysiol.00695.2005. [DOI] [PubMed] [Google Scholar]
- 16.Bopparaju S, Surani S. Sleep and diabetes. Int J Endocrinol 2010. 2010:759509. doi: 10.1155/2010/759509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Das AK. RSSDI Textbook of Diabetes Mellitus. 3rd ed. New Delhi, India: Jaypee Brothers Medical Publishers (P) Ltd; 2014. Sleep and type 2 diabetes mellitus. [Google Scholar]
- 18.West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax. 2006;61:945–50. doi: 10.1136/thx.2005.057745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, et al. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32:1017–9. doi: 10.2337/dc08-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaw JE, Punjabi NM, Wilding JP, Alberti KG, Zimmet PZ. International Diabetes Federation Taskforce on Epidemiology and Prevention. Sleep-disordered breathing and type 2 diabetes: A report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res Clin Pract. 2008;81:2–12. doi: 10.1016/j.diabres.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 21.Nannapaneni S, Ramar K, Surani S. Effect of obstructive sleep apnea on type 2 diabetes mellitus: A comprehensive literature review. World J Diabetes. 2013;4:238–44. doi: 10.4239/wjd.v4.i6.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aronsohn RS, Whitmore H, Van Cauter E, Tasali E. Impact of untreated obstructive sleep apnea on glucose control in type 2 diabetes. Am J Respir Crit Care Med. 2010;181:507–13. doi: 10.1164/rccm.200909-1423OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 24.Sousa AD, Kalra S. Sleep hygiene and diabetes: Suggestions for primary care. J Pak Med Assoc. 2017;67:814–5. [PubMed] [Google Scholar]
- 25.Kumar S, Hari Kumar KV. Sleep hygiene and diabetes. J Pak Med Assoc. 2016;66:1665–8. [Google Scholar]


