TO THE EDITOR
Mediastinal gray-zone lymphoma lies intermediate between nodular-sclerosis classic Hodgkin’s lymphoma and primary mediastinal B-cell lymphoma (a subtype of diffuse large B-cell lymphoma), with overlapping clinical, histologic, and molecular features.1,2 Genetic characteristics shared among these tumors include frequent 9p24.1 copy-number alterations, which occur in approximately 61% of patients with mediastinal gray-zone lymphoma.3 The programmed death 1 (PD-1) pathway is proposed to play a key role in lymphomagenesis, providing escape from immune surveillance. We report three cases of refractory mediastinal gray-zone lymphoma that were successfully treated with PD-1 blockade.
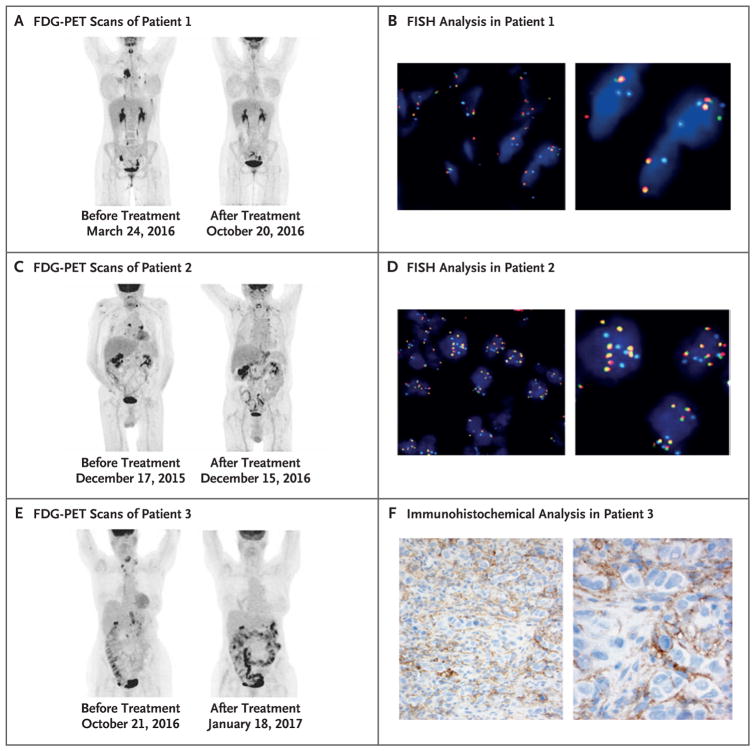
An 18-year-old woman (Patient 1) received a diagnosis of mediastinal gray-zone lymphoma after biopsy of a mediastinal mass showed an immunophenotype intermediate between diffuse large B-cell lymphoma and classic Hodgkin’s lymphoma (positive for CD20, CD30, and CD15). After a partial response to dose-adjusted etoposide, doxorubicin, and cyclophosphamide with vincristine and prednisone plus rituximab (DA-EPOCH-R), she had disease progression 6 weeks after salvage radiotherapy and had a complete metabolic response (i.e., normalization of an abnormal positron-emission tomographic scan) after treatment with pembrolizumab (Fig. 1A). After 235 days of treatment, she underwent allogeneic transplantation. Rearrangement of the genes encoding the PD-1 and PD-2 ligands (PD-L1/ PD-L2) was detected by fluorescence in situ hybridization (FISH) analysis (Fig. 1B).
Figure 1. 18F-Fluorodeoxyglucose (FDG) Positron-Emission Tomographic (PET) Response, 9p24.1 (PD-L1/PD-L2) Fluorescence In Situ Hybridization (FISH) Analysis, and PD-L1 Immunohistochemical Analysis.
Panels A, C, and E show maximum-intensity projection images from FDG-PET scans of three patients with refractory mediastinal gray-zone lymphoma who were treated with programmed death 1 (PD-1) blockade. As shown in Panel A, Patient 1 had a complete metabolic response after treatment with pembrolizumab, with no residual hypermetabolic uptake on post-treatment imaging. As shown in Panel C, Patient 2 had a complete metabolic response after treatment with pembrolizumab, with residual uptake in the neck and upper chest that was consistent with normal-variant brown fat. As shown in Panel E, Patient 3 had a complete metabolic response after treatment with nivolumab, with diffuse uptake in the bowel that was compatible with inflammation. Amplification and rearrangement of the PD-L1/PD-L2 locus was investigated by FISH with the use of a PD-L1/PD-L2 Break Apart probe (labeled with Spectrum Red and Spectrum Green) and a CEP 9 probe (labeled with Spectrum Aqua). Panel B shows rearrangement of the PD-L1/PD-L2 locus in Patient 1, with a split green signal suggesting the presence of an inversion within this region. Panel D shows amplification of the PD-L1/PD-L2 locus in Patient 2, with evidence of multiple fusion signals (69% of cells with ≥6 copies per cell, 20% with 3 to 5 copies, and 11% with ≤2 copies). In Panel F, immunohistochemical analysis in Patient 3 shows focal membranous expression of PD-L1 in the lymphoma cells, with additional expression seen on the small background cells surrounding the malignant lymphoma cells.
A 76-year-old man (Patient 2) received a diagnosis of mediastinal gray-zone lymphoma after biopsy of a subcarinal mass showed diffuse large B-cell lymphoma with an immunophenotype of classic Hodgkin’s lymphoma (positive for CD30 and PAX5 and negative for CD10, CD20, and CD15). After a partial response to DA-EPOCH-R, he had disease progression. He had a complete metabolic response after treatment with pembrolizumab and continues to be in remission on day 381 of treatment (Fig. 1C). Amplification of PD-L1/PD-L2 was detected by FISH, with 69% of cells having at least six copies per cell (Fig. 1D).
An 80-year-old woman (Patient 3) received a diagnosis of mediastinal gray-zone lymphoma after biopsy of an axillary lymph node showed an immunophenotype intermediate between diffuse large B-cell lymphoma and classic Hodgkin’s lymphoma (positive for CD20, CD30, and CD15). Despite a complete metabolic response to DA-EPOCH-R, she had a relapse and disease progression after treatment with brentuximab; a combination of rituximab, gemcitabine, and oxaliplatin; and mediastinal radiation. She had a complete metabolic response after treatment with nivolumab and continues to be in remission on day 161 of treatment (Fig. 1E). Immunohistochemical analysis showed focal membranous PD-L1 expression (Fig. 1F).
Genetic susceptibility to immune-checkpoint inhibition that is conferred by 9p24.1 copy-number alterations is best characterized in classic Hodgkin’s lymphoma. Near-uniform (97%) concordant copy-number alterations in PD-L1/PD-L2 have been shown in cases of classic Hodgkin’s lymphoma by means of FISH, with 2% having a translocation at this locus.4 Nivolumab5 and pembrolizumab have a high frequency of response in relapsed or refractory classic Hodgkin’s lymphoma but not in primary mediastinal B-cell lymphoma. Recent findings indicate that mediastinal gray-zone lymphoma may be more closely related to classic Hodgkin’s lymphoma than to primary mediastinal B-cell lymphoma.2 These findings suggest that PD-1 inhibitors may be therapeutically important for mediastinal gray-zone lymphoma, which is more resistant to treatment than classic Hodgkin’s lymphoma or primary mediastinal B-cell lymphoma.2
The high frequency of 9p24.1 copy-number alterations across mediastinal lymphomas suggests a disease-specific, genetically determined dependence on PD-1 for survival. These cases provide early evidence for using PD-1 inhibition in relapsed or refractory mediastinal gray-zone lymphoma, which warrants further testing.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
Contributor Information
Christopher Melani, National Cancer Institute, Bethesda, MD
Ajay Major, University of Colorado School of Medicine, Aurora, CO
Jeffrey Schowinsky, University of Colorado School of Medicine, Aurora, CO
Mark Roschewski, National Cancer Institute, Bethesda, MD
Stefania Pittaluga, National Cancer Institute, Bethesda, MD
Elaine S. Jaffe, National Cancer Institute, Bethesda, MD
Svetlana D. Pack, National Cancer Institute, Bethesda, MD
Zied Abdullaev, National Cancer Institute, Bethesda, MD
Mark A. Ahlman, National Institutes of Health, Bethesda, MD
Jennifer J. Kwak, University of Colorado School of Medicine, Aurora, CO
Rustain Morgan, University of Colorado School of Medicine, Aurora, CO
Rachel Rabinovitch, University of Colorado School of Medicine, Aurora, CO
Zenggang Pan, University of Colorado School of Medicine, Aurora, CO
Bradley M. Haverkos, University of Colorado School of Medicine, Aurora, CO
Jonathan A. Gutman, University of Colorado School of Medicine, Aurora, CO
Daniel A. Pollyea, University of Colorado School of Medicine, Aurora, CO
Clayton A. Smith, University of Colorado School of Medicine, Aurora, CO
Wyndham H. Wilson, National Cancer Institute, Bethesda, MD
Manali Kamdar, University of Colorado School of Medicine, Aurora, CO
References
- 1.Traverse-Glehen A, Pittaluga S, Gaulard P, et al. Mediastinal gray zone lymphoma: the missing link between classic Hodg-kin’s lymphoma and mediastinal large B-cell lymphoma. Am J Surg Pathol. 2005;29:1411–21. doi: 10.1097/01.pas.0000180856.74572.73. [DOI] [PubMed] [Google Scholar]
- 2.Wilson WH, Pittaluga S, Nicolae A, et al. A prospective study of mediastinal gray-zone lymphoma. Blood. 2014;124:1563–9. doi: 10.1182/blood-2014-03-564906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eberle FC, Salaverria I, Steidl C, et al. Gray zone lymphoma: chromosomal aberrations with immunophenotypic and clinical correlations. Mod Pathol. 2011;24:1586–97. doi: 10.1038/modpathol.2011.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roemer MG, Advani RH, Ligon AH, et al. PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol. 2016;34:2690–7. doi: 10.1200/JCO.2016.66.4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ansell SM, Lesokhin AM, Borrello I, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med. 2015;372:311–9. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]