Abstract
Context:
Trust in health care is of high intrinsic value. It also leads to positive outcomes such as better treatment adherence and disclosure of sensitive information. Therefore, there is a need to measure trust in health care objectively.
Aims:
To assess the psychometric properties of the Trust in Physician Scale in Tamil Nadu, India.
Settings and Design:
The study was conducted in a private tertiary hospital setting in Tamil Nadu by a cross-sectional survey design.
Methods:
The Trust in Physician Scale and General Trust Scale were administered to 288 participants in the waiting area of a tertiary care hospital in Tamil Nadu.
Statistical Analysis:
Descriptive statistics, exploratory factor analysis, and Cronbach's alpha statistics were used to assess the validity and reliability of the scale.
Results:
The respondents were predominantly men from rural areas, older than 35 years of age, and with lesser than 8 years of schooling. The questionnaire had acceptable internal consistency with Cronbach's alpha of 0.707 (95% confidence interval 0.654–0.755). Exploratory factor analysis divided the questionnaire into four domains. Seven items loaded into factor 1 which explained dependability and competence of the physician, two items loaded on factor 2, and one each in factors 3 and 4. The latter four items had very low item to total correlations and hence did not contribute much to the questionnaire.
Conclusions:
The Trust in Physician questionnaire needs to be modified to accurately measure the domains of trust in the context of the study area. More qualitative studies are required to understand the domains of trust in this cultural and social context.
Keywords: Internal consistency, reliability, Trust in Physician, validity
Introduction
Trust in Physician is an important construct which influences the dynamics of the doctor–patient relationship. Trust in the context of health care can be defined as an optimistic acceptance of the state of vulnerability of the patient, in which the patient believes that the health-care provider will act in his/her best interest.[1] Several researchers have studied trust in health care and have described its dimensions and determinants.[1,2,3]
Trust in health care has not only intrinsic value but also instrumental value. Trust leads to improved adherence to treatment, continuity of care with the provider, improved self-efficacy, better disclosure of sensitive information, and better self-reported health status.[4,5,6,7,8,9] Some studies have looked at interventions to promote trust in health care. Although the evidence is not supportive of any of the interventions, there is a possibility that trust could be potentially built by behavioral interventions.[10]
For this to be studied and operationalized, effective tools are needed for measuring trust. Several tools have been developed for measurement of trust in health care. Some of these tools measure trust in physician, some in health system as a whole and some in health insurers. These tools have been reported to have good psychometric properties.[11] All these tools have been developed in Western countries in developed settings. The characteristic feature of these developed country settings is the availability of robust health systems, wide coverage of health insurance, low out-of-pocket health expenditure, and high public investment in health care. Trust in health care in the low- and middle-income country settings is likely to be different. Availability and accessibility of health care to all people, especially the economically and socially marginalized, are still a steep task. Out-of-pocket expenditure is very high and public investment in health care is low. The validity and reliability of the tools to measure trust in these settings need to be assessed.
The Trust in Physician Scale by Anderson and Dedrick is one of the oldest scales for the measurement of trust. It was developed in 1990 as a tool to measure interpersonal trust between patient and physician and has eleven items. It has three-dimensional structure measuring physician dependability, confidence in physician knowledge and skills, and confidentiality and reliability of information received from the physician. The tool also has excellent psychometric properties.[12] Thom et al. modified this scale in 1999 and the modified tool also has good psychometric properties.[13] The objective of the present study is to test the psychometric properties of the modified Trust in Physician Scale in the tertiary hospital-based setting in Tamil Nadu, India. This would give an idea of the validity and reliability of this scale in the setting of developing countries.
Methods
The study was conducted in a medical college teaching hospital in Kancheepuram district of Tamil Nadu located in the southern part of India. The hospital has multiple specialties and caters to people in and around Kancheepuram district. Patients attending the hospital come from both urban and rural settings. Two questionnaires were used for data collection. One was the Trust in Physician Scale which has items assessing the level of Trust in Physician and the other General Trust Scale which assesses the general trust orientation of individuals.[12,14] Both these scales have statements which the respondent is asked to rate in a Likert scale of 1–5, where 1 stands for “strongly disagree” and 5 stands for “strongly agree.”
The study was conducted in two stages. In the first stage, the questionnaires were given to experts in the field of sociology, anthropology, psychology, and medical practice to assess the face and content validity of the items in the two questionnaires. During the second stage, the questionnaires were administered to patients in the tertiary hospital.
All adult patients aged 18 and above in the hospital waiting area who were waiting to see the doctors in the internal medicine, general surgery, and obstetrics and gynecology outpatient units were eligible to participate in the study. Patients who were in severe distress and in emergency situations were not included. The sample size was fixed at 310 based on previous studies on questionnaire validation and guidelines of sample size for survey research.[15] The tools were translated to Tamil, the local vernacular language. Then, it was back translated to English by an uninvolved third person to check validity of translation.
The overall Trust in Physician score and General Trust score were computed by adding the scores for individual items. The Trust in Physician score and General Trust score were categorized using the median score. People with high and low trust were those who scored above and below the median, respectively. Apart from this, demographic details were also collected from each participant.
Informed consent was obtained from the participants before the study. The respondents were provided adequate privacy for answering the questions and they were assured that their treatment in the hospital will be independent of the responses that they provide to the questionnaire. The researcher who was not part of the hospital treatment team administered the questionnaire in Tamil language and gave the respondents enough time to think and answer each question. After the respondent gave the answers, they were noted down by the researcher. The study was approved by the Institutional Review Board of the School of Public Health, SRM University, by expedited review process as the ethical risks involved were minimal.
The collected data were entered into Epi Info version 3.5.3 (CDC). Validation of the data entry was done by a random check of questionnaires and database for 10% of the sample. The data were exported to Statistical Package for Social Sciences (SPSS) version 17 (IBM) for further analysis and cleaned. Simple descriptive and frequencies were computed. Exploratory factor analysis was performed using principal component extraction and varimax rotation methods for the Trust in Physician Scale to study its dimensionality. Cronbach's alpha was calculated for assessing internal consistency of the Trust in Physician Scale. The association between the scores in the Trust in Physician Scale and the General Trust Scale was studied to test if there is a concurrence between the two measures.
Results
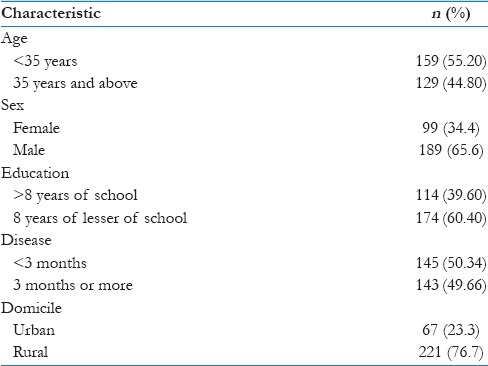
Out of 310 patients who were approached for the study, 288 responded (response rate 92.9%). Of the respondents, 55.2% were below 35 years of age and the rest were 35 years or above. Only 34.4% were women. Of the respondents, 39.6% had a graduate level education and the rest had only completed school. Those who had severe illnesses comprised 49.66% of the respondents, and the remaining had nonserious illnesses. Urban respondents comprised 76.7% and the remaining were from rural areas. These basic demographic details are depicted in Table 1.
Table 1.
Characteristics of the study population
Trust in Physician Scale
The mean Trust in Physician score was 44.2 (standard deviation [SD] 6.7) where the maximum possible score was 55 and minimum was 11. The scores were positively skewed and there were more in the high trust region and less respondents in the low trust region.
General Trust Scale
The mean general trust score was 66.5 (SD 12.1) where the maximum possible score was 150 and minimum 30. The scores had a normal distribution as assessed by the Shapiro Wilk's test.
Psychometric properties of Trust in Physician Scale
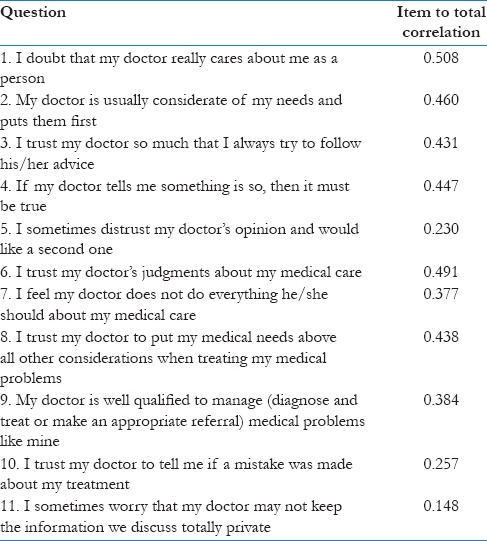
Content validity assessment by experts revealed an acceptable content validity of all items in the scale. The reliability of the scale was tested by computing Cronbach's alpha statistic which was 0.707 (95% confidence interval [CI] 0.654–0.755). The item-to-total correlation for each of the 11 items was calculated as a representation of how much the response to each item corresponded to the overall score in the scale. The item-to-total correlation statistics are shown in Table 2. The highest item-to-total correlation was observed for the item “I doubt that my doctor really cares about me as a person” with a correlation coefficient of 0.508 and the least was observed for the item “I sometimes worry that my doctor may not keep the information we discuss totally private” with a coefficient of 0.148.
Table 2.
Item to total correlation of the Trust in Physician Scale
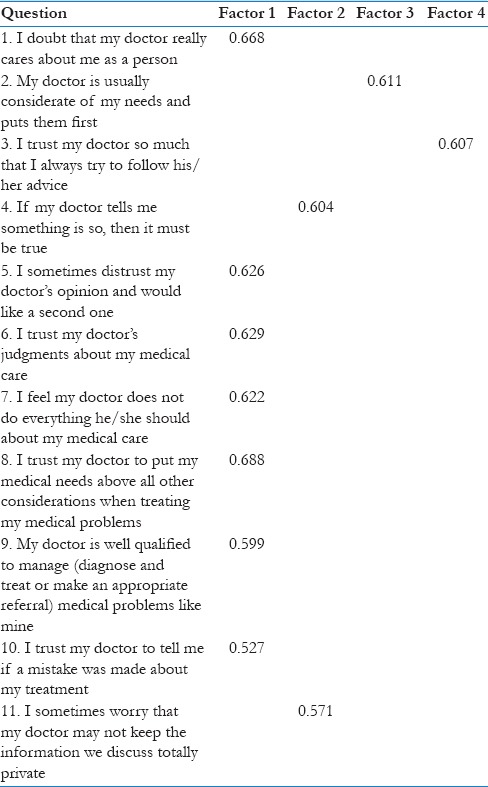
Exploratory factor analysis showed that a four-factor structure explained 59.7% of the overall variance. The factor model was statistically significant as shown by Bartlett's test of sphericity (P < 0.001) and the sampling was adequate as shown by the Kaiser–Meyer–Olkin test value of 0.809.
The factor matrix with the loadings is shown in Table 3. It shows that seven items loaded in factor 1, two items in factor 2, and one each in factors 3 and 4. The items which loaded on factor 1 were, “I doubt that my doctor really cares about me as a person,” “My doctor is usually considerate of my needs and puts them first,” “I trust my doctor to put my medical needs above all other considerations when treating my medical problems,” “I trust my doctor so much that I always try to follow his/her advice,” “If my doctor tells me something is so, then it must be true,” “I trust my doctor's judgments about my medical care,” “My doctor is well qualified to manage (diagnose and treat or make an appropriate referral) medical problems like mine.” The second factor had two items loaded on it, namely, “I sometimes worry that my doctor may not keep the information we discuss totally private” and “I trust my doctor to tell me if a mistake was made about my treatment.” Two items loaded separately into two separate factors these were, “I sometimes distrust my doctor's opinion and would like a second one” and “I feel my doctor does not do everything he/she should about my medical care.”
Table 3.
Factor loading matrix for the Trust in Physician Scale
Association between general trust and physician trust
The association between general trust score and physician trust score was studied. It was observed that those who had high general trust had a greater chance of having higher Trust in Physician (odds ratio 2.677; 95% CI: 1.660–4.318).
Discussion
This study was done to explore and validate the Trust in Physician Scale in the setting of a tertiary hospital in Tamil Nadu. Trust in Physician is a scarcely researched topic in the developing countries. However, the rising level of distrust in the health system among people in developing countries is evident.[16] In the private sector, the unregulated, irrational practices and the potential for exploitation and in the public sector the apathy of the providers lead to significant distrust among the public. Trust is highly relevant in primary care and family practice. The reason for this is that the primary physician is the first point of contact for the patient for any illness. If the patient develops a trusting relationship with their primary physician, it can lead to several benefits such as reduced need for second opinions, reduction in unnecessary investigations, and health care expenditure. It can also lead to better satisfaction of the patient. Some studies have shown that when the patients have high level of trust in their primary physician, they report better well-being and improvement of symptoms. They also report higher levels of satisfaction.[17] Especially for chronic noncommunicable diseases, there is increasing evidence that a trusting doctor–patient relationship will increase adherence to treatment as well as better clinical outcomes.[18] Therefore, there is a need for an increased awareness and exploration of trust as an instrumental value in health care. This study is one of the first few steps in the direction of development of a tool to measure Trust in Physician in the Indian context.
A previous study done in a similar hospital-based setting in Pune, India, explored the dimensions of a good doctor–patient relationship such as concordance, trust, and enablement. This study used the Trust in Physician Scale. It was reported that women had lower levels of Trust in Physician as compared to men. It was also reported that better doctor–patient concordance was associated with higher levels of trust.[19] Subsequently, qualitative studies in the Indian context have reported the dimensions and determinants of trust in physicians as unique from existing Western ideas.[20] Therefore, it is likely that the Trust in Physician Scale may not appropriately capture the construct in this context.
The sample of respondents was selected from patients attending a private tertiary hospital in Tamil Nadu. Since the patients were interviewed while they were in the waiting area of the respective outpatient departments, it is highly likely that the construct that was explored in the study was trust and not some other aspect of the doctor–patient relationship. Majority of the respondents were men with low levels of literacy (8 years of schooling or lesser) and from rural background. Therefore, it cannot be said that the findings of this validity research are applicable to all the people of Tamil Nadu.
The scale was found to have good face and content validity. The tool also had an acceptable internal consistency. The item to total correlation revealed that the item on confidentiality, second opinion, and disclosure of errors by the doctor had poor correlation with the overall score. Trust in Physician in the Indian context, especially in the sample with a lower level of literary, is likely to be implicit and unquestioning. There is a need to explore this aspect of unquestioning trust in physicians by qualitative studies.
Factor analysis to explore the dimensional structure of the questionnaire revealed that the questionnaire is best explained by a four-dimensional structure. The first dimension has seven items loaded on to it which together describe the competence and the dependability of the doctor. These two dimensions had been described separately in the original questionnaire but are clubbed together during this validation process. Two items pertaining to confidentiality and disclosure of medical errors by the doctor loaded together as one factor. It was previously described that these two items had poor correlation with the overall trust score. Therefore, this factor contributes little to the construct of trust in physician. Two other items loaded separately as two factors, one of them referring to seeking second opinion and other on doubt whether the doctor is doing all appropriate things for the patient's treatment. Again, it was previously noted that second opinion was poorly correlated to the overall trust score. Therefore, in essence, the factor structure of the questionnaire is one-dimensional with the majority of the important items loading into one factor.
Most of the important items relating to the physician's competence and dependability load onto one factor. Patients in the Indian setting view Trust in Physician largely based on the ability and dependability of the doctor. Other factors which were identified as important in the developed country setting such as confidentiality, need for second opinion, disclosure of mistakes in treatment, and concern whether the doctor is doing all appropriate treatments were not identified as important in the Indian context. This could imply that the Trust in Physician Scale needs to be modified for better applicability in the Indian setting. There is a need for qualitative exploration of the dimensions and determinants of trust in the Indian setting.
The major limitation of this study is that it was conducted in a hospital-based setting. It captures the dimensions of trust among patients who are visiting a particular tertiary care setting. The concepts of trust are likely to be different in a community setting. However, as discussed previously, the findings of this study can be generalized to a typical tertiary care facility in a developing country setting.
Conclusion
The development and validation of a modified tool for measuring trust in physicians is an important first step in making trust measurement a part of routine evaluation of performance of health systems. This would further lead to studies on interventions to promote trust and use its instrumental values for health system improvement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the intellectual contributions of Prof. Ch. Satish Kumar, Dean, School of Public Health.
References
- 1.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Q. 2001;79:613–39. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: Conceptual and measurement issues. Health Serv Res. 2002;37:1419–39. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balkrishnan R, Dugan E, Camacho FT, Hall MA. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41:1058–64. doi: 10.1097/01.MLR.0000083743.15238.9F. [DOI] [PubMed] [Google Scholar]
- 4.Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–20. [PubMed] [Google Scholar]
- 5.Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. J Fam Pract. 2005;54:344–52. [PubMed] [Google Scholar]
- 6.Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749–55. doi: 10.1001/archinte.165.15.1749. [DOI] [PubMed] [Google Scholar]
- 7.Ohya Y, Williams H, Steptoe A, Saito H, Iikura Y, Anderson R, et al. Psychosocial factors and adherence to treatment advice in childhood atopic dermatitis. J Invest Dermatol. 2001;117:852–7. doi: 10.1046/j.0022-202x.2001.01475.x. [DOI] [PubMed] [Google Scholar]
- 8.Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc Sci Med. 2009;68:1060–8. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 9.Mohseni M, Lindstrom M. Social capital, trust in the health-care system and self-rated health: The role of access to health care in a population-based study. Soc Sci Med. 2007;64:1373–83. doi: 10.1016/j.socscimed.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 10.McKinstry B, Ashcroft RE, Car J, Freeman GK, Sheikh A. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2006;3:CD004134. doi: 10.1002/14651858.CD004134.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Goudge J, Gilson L. How can trust be investigated? Drawing lessons from past experience. Soc Sci Med. 2005;61:1439–51. doi: 10.1016/j.socscimed.2004.11.071. [DOI] [PubMed] [Google Scholar]
- 12.Anderson LA, Dedrick RF. Development of the Trust in Physician scale: A measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67(3 Pt 2):1091–100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 13.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician scale. The Stanford Trust Study Physicians. Med Care. 1999;37:510–7. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Couch LL, Adams JM, Jones WH. The assessment of trust orientation. J Pers Assess. 1996;67:305–23. doi: 10.1207/s15327752jpa6702_7. [DOI] [PubMed] [Google Scholar]
- 15.Kotrlik JW, Higgins CC. Organizational research: Determining appropriate sample size in survey research appropriate sample size in survey research. Inf Technol Learn Perform J. 2001;19:43. [Google Scholar]
- 16.Peters DH, Muraleedharan VR. Regulating India's health services: To what end. What future? Soc Sci Med. 2008;66:2133–44. doi: 10.1016/j.socscimed.2008.01.037. [DOI] [PubMed] [Google Scholar]
- 17.Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: Relationship to patient requests. Fam Pract. 2002;19:476–83. doi: 10.1093/fampra/19.5.476. [DOI] [PubMed] [Google Scholar]
- 18.Farin E, Gramm L, Schmidt E. The patient-physician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. J Behav Med. 2013;36:246–58. doi: 10.1007/s10865-012-9419-z. [DOI] [PubMed] [Google Scholar]
- 19.Banerjee A, Sanyal D. Dynamics of doctor-patient relationship: A cross-sectional study on concordance, trust, and patient enablement. J Family Community Med. 2012;19:12–9. doi: 10.4103/2230-8229.94006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gopichandran V, Chetlapalli SK. Dimensions and determinants of trust in health care in resource poor settings – A qualitative exploration. PLoS One. 2013;8:e69170. doi: 10.1371/journal.pone.0069170. [DOI] [PMC free article] [PubMed] [Google Scholar]


