Abstract
Introduction
Sudden unexpected deaths comprise the most important and worthy investigation case profiles in both neurology and forensic medicine. Epilepsy, which is one of the neuropathological causes of sudden unexpected deaths, is an important disorder having mysterious aspects. The aim of this study is to make common the points of view between neurology and forensic medicine experts and to discuss the features of the findings together with the related clinical hypotheses, leading to the differential diagnosis of sudden unexpected death in epilepsy (SUDEP) by presenting autopsy findings and available medical data of patients who had a prior diagnosis of epilepsy.
Methods
In Istanbul, the cases of 20334 autopsied patients who were referred to The Ministry of Justice Council of Forensic Medicine between 2007 and 2011 were identified from the complete forensic autopsy data of the city and were retrospectively reviewed. Patients who had a prior diagnosis of epilepsy were included. Both descriptive and inferential statistical analyses were performed through the parameters of demographical data, physical properties, incident features, macroscopic–microscopic autopsy findings, and cause of death initially for all cases and then separately for SUDEP cases.
Results
Among the 20334 patients, 112 were determined to have a prior diagnosis of epilepsy. A possible macroscopic and/or microscopic epileptic focus was present in 23 (20.5%) of these 112 cases. The cause of death was determined to be SUDEP in 40 (35.7%) cases, while it could not be determined in 28 (25%) cases. Among patients whose death cause was considered as SUDEP, the male-to-female ratio was 1.1:1, while the mean age was 31.5±13.9 years in males and 29.6±12.9 years in females. The presence of hypertrophy and myocardial scar tissue findings in the microscopic examination were significantly more frequent among patients determined to have died from cardiovascular diseases compared to patients in the SUDEP group (p=0.001 for each finding). Besides, in 40 SUDEP cases, 38 (95%) patients underwent toxicological analysis and no antiepileptic agent was detected in 21 (55.3%) of these.
Conclusion
It can be concluded that there is equality in gender distribution among SUDEP patients, that the young adult population has a slightly increased risk for SUDEP, and that the inconsistent use of antiepileptic medicines is a greater risk factor for SUDEP than polytherapy. Besides, it is important to emphasize that all clinical and postmortem parameters together should be considered for the differential diagnosis of SUDEP, particularly with cardiovascular diseases.
Keywords: Epilepsy, sudden unexpected death in epilepsy, autopsy, antiepileptics
INTRODUCTION
Sudden unexpected deaths comprise the most important and worthy investigation case profiles in both neurology and forensic medicine. Epilepsy, stroke, intracranial space-occupying lesions (tumors or colloidal cysts), infections (cerebral abscess or acute meningitis), and inflammatory or metabolic diseases affecting the nervous system are among the neuropathological causes of sudden unexpected deaths (1).
Epilepsy is caused by various reasons and is characterized by recurrent and unforeseen interruptions of normal brain function (2). Epileptic patients have an increased mortality risk compared to the normal population (3). In various studies, the mortality risk of epileptic patients has been reported to be 2–4-times higher than normal individuals (3,4,5,6).
Death can be a direct result of an epileptic attack itself or a result of secondary unnatural causes such as trauma or drowning in epileptic patients. Sudden and unexpected death of an epileptic patient includes deaths that do not occur as a consequence of a secondary cause. Sudden epileptic attacks have been reported to be responsible for 2–17% of deaths among epileptic individuals (7,8).
In the 1990s, sudden unexpected death in epilepsy (SUDEP) was defined using similar criteria in different reports. The common criteria in these reports can be listed as follows: sudden and unexpected character of death in the presence or absence of any witness, absence of any trauma or drowning history, no toxicological and anatomical diagnostic evidence explaining death in the autopsy, and exclusion of status epilepticus (SE) (9,10). The presence or absence of any finding indicating a seizure at the time or just prior to death is not considered as a criterion for the definition of SUDEP (3). Nashef et al. (11) described six categories to classify deaths of epileptic patients: definite SUDEP/definite SUDEP plus, probable SUDEP/probable SUDEP plus, possible SUDEP, near-SUDEP/near-SUDEP plus, not SUDEP, and unclassified.
The aim of this study is to present autopsy findings and available medical data of patients who had a prior diagnosis of epilepsy to make common the points of view among neurology and forensic medicine experts and to discuss the features of the findings together with the related clinical hypotheses, leading to the differential diagnosis of SUDEP.
METHODS
Sampling
In Istanbul, the cases of 20334 autopsied patients who were referred to The Ministry of Justice Council of Forensic Medicine between 2007 and 2011 were identified from the complete forensic autopsy data of the city and were retrospectively reviewed. Patients who had a prior diagnosis of epilepsy were included.
Data Collection Tools and Implementation
Autopsy findings and medical data were collected from autopsy reports and judicial documents available in the archive files. Although designed as a retrospective study with no identification data, it is out of the scope of the informed consent doctrine; all procedures in the study were performed after obtaining ethical and scientific approval of The Ministry of Justice Council of Forensic Medicine dated 12/03/2013, No. 132 and in line with the 1964 Helsinki declaration including its later amendments. For case classification, initially, all epileptic patients were evaluated through the parameters of demographical data, incident features, macroscopic–microscopic autopsy findings, and cause of death. Causes of deaths were classified in five groups as SUDEP, cardiovascular disease, other natural causes, unnatural causes, and undetermined. Then, SUDEP patients were separately evaluated through the same parameters. SUDEP criteria used in our study included sudden and unexpected death character regardless of the presence of a witness or its association with the attack, exclusion of SE, and other toxicological–anatomical causes of death.
Statistical Analysis
Collected data were analyzed through both descriptive (mean, standard deviation, median, frequency, rate, and minimum and maximum) and inferential (Fisher–Freeman–Halton and Yates’ continuity correction tests) statistic methods in NCSS 2007 (Kysville, Utah, USA). Significance was determined to be p<0.01 and p<0.05. Patients for whom cause of death could not be determined were excluded from inferential statistical analyses. Interpretations of the results were performed as SUDEP versus non-SUDEP patients, SUDEP versus cardiovascular disease patients, SUDEP versus all patients, or directly as a comparison with the literature according to the clinical feature of the parameter evaluated.
RESULTS
Among the 20334 cases of autopsied patients, 112 were found to have a prior diagnosis of epilepsy. At first, all 112 patients who had a prior diagnosis of epilepsy were used in the classification to see the general picture of epileptic patients through our parameters and to discuss the picture in comparison with SUDEP cases. Then, results of the SUDEP cases were calculated and separately presented.
Data for All Patients with a Prior Diagnosis of Epilepsy
Seventy-four (66.1%) patients were males, whereas 38 (33.9%) were females, a ratio of 1.9:1. The mean age was 34.2±15.8 (range 0–87; median 33) years, whereas it was 36.0±17.4 years in males and 30.9±11.4 years in females. When the annual incidence was evaluated, the highest number of cases (n=30, 26.8%) was observed in 2010.
Although not specific to epileptic attacks, findings such as abrasions, ecchymoses, or any scars on the anterior–lateral surfaces of the extremity joints or on the protruding areas of the head, froth at the mouth–nose, petechial bleeding foci in conjunctivas, and lacerations on the tongue were considered to be supportive details for a possible epileptic attack. These findings were observed in 63 (56.3%) cases. Detailed examination of the tongue was performed in 64 (57.1%) patients. Of these, old and new lacerations were found in 22 (19.6%) cases.
Findings obtained from the macroscopic and microscopic examination of the brain were classified in five main groups as yellow–brown plaques, space-occupying lesions, edema, infection, hemorrhagic areas, and insignificant findings. A possible epileptic focus was present in 23 (20.5%) cases. Of these, the focus was observed only macroscopically in seven (6.3%) cases, only microscopically in nine (8.0%), and both macroscopically and microscopically in seven (6.3%) (Table 1). In the macroscopic examination, edema was observed in 56 (50.0%) cases and findings suggestive of hemorrhage in 12 (12.5%), while no remarkable finding was observed in 36 (32.1%) cases. Likewise, the microscopic examination of the brain revealed edema in 26 (23.2%) cases, hemorrhage in 16 (14.3%), and infection in 5 (4.5%), while no diagnostic feature was found in 56 (50.0%) cases (Table 2). Examination of the lungs revealed hypoxic findings such as subpleural petechiae on the interlobar surfaces in 47 (42.0%) cases. Edema was observed in 77 (68.8%) cases and interstitial hemorrhage in 14 (12.5%) (Table 3).
Table 1.
Determination of an area suggestive of a possible epileptic focus in the macroscopic and microscopic examination of the brain
| Presence of an area suggestive of a possible epileptic focus | Macroscopic | Total | ||
|---|---|---|---|---|
| Yes | No | |||
| Microscopic | Yes | 7 | 9 | 16 |
| No | 7 | 0 | 7 | |
| Total | 14 | 9 | 23 | |
Table 2.
Potential epilepsy-related macroscopic and microscopic findings of the brain
| Macroscopic Evaluation | n | % |
|---|---|---|
| Epileptic suspicious area | 9 | 8.0 |
| Edema | 52 | 46.4 |
| Hemorrhage | 9 | 8.0 |
| Infection | 0 | 0.00 |
| Epileptic focus? +Edema | 3 | 2.7 |
| Epileptic focus?+Hemorrhage | 2 | 1.8 |
| Edema+Hemorrhage | 1 | 0.9 |
| Unremarkable | 36 | 32.1 |
| Total | 112 | 100 |
| Microscopic Evaluation | ||
| Epileptic focus suspicious area | 15 | 13.4 |
| Edema | 19 | 17.0 |
| Hemorrhage | 10 | 8.9 |
| Infection | 5 | 4.5 |
| Epileptic focus?+Edema | 1 | 0.9 |
| Edema+Hemorrhage | 6 | 5.4 |
| Unremarkable | 56 | 50.0 |
| Total | 112 | 100 |
Table 3.
Macroscopic and microscopic pulmonary findings supporting the diagnosis of SUDEP
| Macroscopic Evaluation | n | % |
|---|---|---|
| Subpleural petechiae | 16 | 14.3 |
| Edema | 39 | 34.8 |
| Interstitial hemorrhage | 4 | 3.6 |
| Subpleural petechiae+Edema | 28 | 25.0 |
| Subpleural petechiae+Edema+ Interstitial hemorrhage | 3 | 2.7 |
| Edema+Interstitial hemorrhage | 7 | 6.3 |
| Other | 15 | 13.4 |
| Total | 112 | 100 |
| Microscopic Evaluation | n | % |
| Edema | 63 | 56.3 |
| Hemorrhage | 15 | 13.4 |
| Edema+Hemorrhage | 12 | 10.7 |
| Other | 22 | 19.6 |
| Total | 112 | 100 |
In our department, the hearts were weighed as a whole without separately detaching any chamber. The ascending aorta and pulmonary artery were removed at the level of 2 cm above the valves. The inferior vena cava and each pulmonary vein were removed at the level of the pericardium border, and the superior vena cava was removed at the level of the right atrium border. The hearts were weighed after routinely opening the heart in the direction of blood flow to remove any possible postmortem clot. Heart weights obtained in this manner were over the expected values in 69 (61.6%) of the 112 cases according to the expected heart weight charts reported by Zeek et al. and Kitzman et al. (12,13). Histological examination of the hearts revealed hypertrophy in 41 (36.6%) cases, and findings from myocardial tissues are presented in Table 4.
Table 4.
Histological examination of myocardial tissues
| All cases (n=112) n (%) | SUDEP (n=40) n (%) | Cardiovascular Deaths (n=14) n (%) | p | ||
|---|---|---|---|---|---|
| Heart weight | |||||
| Normal | 43 (38.4) | 21 (52.5) | 0 (0,0) | a0.002** | |
| Overweight | 69 (61.6) | 19 (47.5) | 14 (100.0) | ||
| Hypertrophy | |||||
| Severe | 31 (27.67) | 7 (17.5) | 12 (85.7) | b0.001** | |
| Mild | 10 (8.92) | 4 (10.0) | 0 | ||
| Absent | 71 (63.39) | 29 (72.5) | 2 (14.3) | ||
| Fibrosis | |||||
| Severe | 26 (23.21) | 7 (17.5) | 4 (28.6) | b0.082 | |
| Mild–Moderate | 12 (10.71) | 2 (5.0) | 3 (21.4) | ||
| Absent | 74 (66.07) | 31 (77.5) | 7 (50.0) | ||
| Scar Tissue | |||||
| Focal | 5 (4.46) | 1 (2.5) | 2 (14.3) | b0.001** | |
| Moderate | 6 (3.35) | 0 | 4 (28.6) | ||
| Absent | 101 (90.17) | 39 (97.5) | 8 (57.1) | ||
| At least one finding | 62 (55.35) | 16 (40.0) | 14 (100.0) | a0.001** | |
| At least two findings | 26 (23.21) | 6 (15.0) | 10 (71.4) | b0.001** | |
| All findings together | 3 (2.68) | 0 | 1 (7.1) | b0.259 | |
Yates’ Continuity Correction Test
Fisher–Freeman–Halton Test
p<0.01
Toxicological analysis was not performed in seven (6.3%) cases according to our autopsy protocols, which mention that toxicological analysis is not mandatory if there is a long inpatient treatment after a battery or falling from a height incident. Among the 105 (93.8%) cases for which toxicological analysis was performed, antiepileptics were positive in 44 (41.9%) (Table 5). Only one antiepileptic agent (monotherapy) was detected in 35 cases, while multiple antiepileptic agents (polytherapy) were detected in nine cases (Table 6). Antiepileptics with ureit structure were the most frequently detected medicines (n=23) among 44 cases. Besides, only barbiturates were detected in four cases, only hydantoins were detected in five cases, and both barbirurates and hydantoins were detected in six cases.
Table 5.
Monotherapy–polytherapy status of all cases
| Cause of Death | No analysis | Not detected | Monotherapy | Polytherapy | Total |
|---|---|---|---|---|---|
| SUDEP | 2 | 21 | 12 | 5 | 40 |
| Cardiovascular | - | 11 | 2 | 1 | 14 |
| Other natural | 3 | 3 | 4 | 0 | 10 |
| Unnatural | 2 | 9 | 8 | 1 | 20 |
| Undetermined | 0 | 17 | 9 | 2 | 28 |
| Total | 7 | 61 | 35 | 9 | 112 |
Table 6.
Classification of antiepileptic agents detected in the toxicological analysis
| Treatment | All cases | Deaths caused by epilepsy | Deaths caused by cardiovascular disease | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| None | 61 | 58.1 | 21 | 55.3 | 11 | 78.6 | 0.437 * |
| Monotherapy | 35 | 33.3 | 12 | 31.6 | 2 | 14.3 | |
| Polytherapy | 9 | 8.6 | 5 | 13.2 | 1 | 7.1 | |
| Total (Patients with postmortem toxicological screening) | 105 | 100 | 38 | 100 | 14 | 100 | |
| Monotype antiepileptics | |||||||
| Agents with ureit structure | 15 | 42.9 | 2 | 16.7 | 2 | 100 | |
| Barbiturate analogs | 4 | 11.4 | 1 | 8.3 | - | - | |
| Hydantoins | 5 | 14.3 | 1 | 8.3 | 1 | 50 | |
| Barbiturates and Hydantoins | 6 | 17.1 | - | - | 1 | 50 | |
| Dibenzazepine analogs | 11 | 31.4 | 5 | 41.7 | - | - | |
| Valproic acid analogs | 5 | 14.3 | 2 | 16.7 | - | - | |
| New generation | 3 | 8.6 | 3 | 25.7 | - | - | |
| Benzodiazepines | 1 | 2.9 | - | - | - | - | |
| Total | 35 | 100 | 12 | 100 | 2 | 100 | |
| Combination of antiepileptics | |||||||
| Ureit-type drugs+Benzodiazepines | 3 | 33.33 | 2 | 40 | - | - | |
| Ureit-type drugs+Dibenzazepine analogues | 2 | 22.22 | 1 | 20 | - | - | |
| Ureit-type drugs+Valproic acid analogues | 2 | 22.22 | 1 | 20 | - | - | |
| Ureit-type drugs+New generation | 1 | 11.11 | 1 | 20 | - | - | |
| Dibenzazepine analogs+Valproic acid analogs+New generation | 1 | 11.11 | - | - | 1 | 100 | |
| Total | 9 | 100 | 5 | 100 | 1 | 100 | |
Fisher–Freeman–Halton Test
Classification based on the circumstances surrounding death revealed that a witness was present at the time of death in 52 (46.4%) cases, while 41 (36.6%) patients were found dead without any witness present at the time of death. Incidents resulting in death were not strongly suggestive of epilepsy (i.e., fall from a height, traffic accident, battery, hanging, suicide, intoxication, food aspiration, or burns) in 15 (13.4%) cases. No information about the incidence resulting in death could be acquired in four (3.6%) cases.
Data for Only SUDEP Cases
Classification based on the causes of deaths revealed that 40 (35.7%) patients were determined to have died from SUDEP, 14 (12.5%) from cardiovascular diseases, 10 (8.9%) from other natural diseases, and 20 (17.9%) from unnatural causes. The cause of death could not be determined in 28 (25%) cases (Figure 1).
Figure 1.
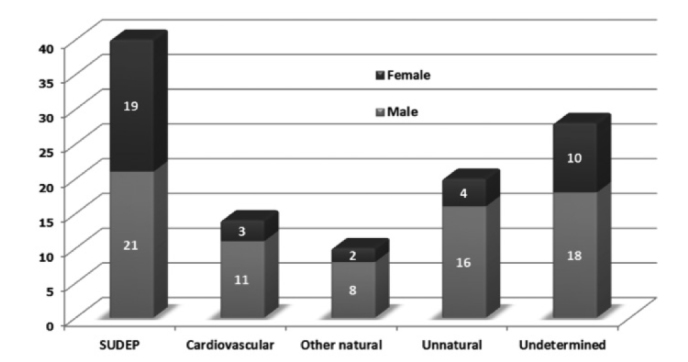
Causes of deaths determined through postmortem investigation
When patients determined to have died from SUDEP (n=40, 35.7%) were separately evaluated, the mean age was found to be 30.6±13.3 years (range 1–60 years; 31.5±13.9 years among 21 males and 29.6±12.9 years among 19 females). The mean age of patients determined to have died due to cardiovascular diseases (n=14, 12.5%) was found to be 44.4±13.1 years.
No information was obtained regarding the type of epileptic attacks, either from medical documentation or witness statements. Classification based on circumstances surrounding death for the SUDEP cases revealed that 21 (52.5%) patients were found dead without any witness present at the time of death. Of these, 18 (40%) were found at home, two (5%) were found outside, and one (2.5%) was found at the workplace. Of the 18 patients found at home, five were found dead on the bed. When the other 19 (47.5%) cases were evaluated, it was seen that there were insufficient data for three (7.5%) of these cases; the remaining 16 (40%) cases were reported to have died either at home or on the way to hospital due to their current illness. Thus, it was concluded that there was a witness to death in these 16 patients.
External examination findings supportive of a possible epileptic attack were observed in 29 (72.5%) SUDEP cases.
The macroscopic and microscopic examination of the lungs and the brain revealed brain edema in 24 (60%) and pulmonary edema in 37 (92.5%) SUDEP cases. All patients having brain edema (n=24, 60%) also had pulmonary edema. Solitary pulmonary edema was observed in 13 (32.5%) cases, and neither pulmonary nor brain edema was observed in three (7.5%).
In 19 (47.5%) SUDEP cases, the hearts were overweight, while the heart weights were statistically significantly higher among patients determined to have died from cardiovascular diseases than among those in the SUDEP group (p=0.002). Histological examination of these hearts revealed hypertrophy in 11 cases. Hypertrophy and other histological findings of myocardial tissues for patients determined to have died from SUDEP are presented in Table 4 together with the findings of the cardiovascular disease group. The presence of hypertrophy and myocardial scar tissue findings in the microscopic examination were significantly more frequent among patients determined to have died from cardiovascular diseases than among those in the SUDEP group (p=0.001 for each finding). Besides, the severe hypertrophy ratio was 85.7% among patients determined to have died from cardiovascular diseases, while the presence of at least one of the myocardial findings (i.e., microscopic hypertrophy, fibrosis, or myocardial scar tissue) and at least two myocardial findings together were significantly more frequent among patients determined to have died from cardiovascular diseases than among those in the SUDEP group (p=0.001 respectively).
In 21 (55.3%) SUDEP cases, toxicological analysis revealed no antiepileptic agent, while it was not performed in two cases. Active substances of antiepileptic agents were detected in 17 (44.7%) cases. In addition, there was no statistically significant difference between the treatment statuses of patients determined to have died from cardiovascular diseases and those from SUDEP. The distribution of treatment statuses and detected antiepileptic agents are presented in Table 5 and Table 6.
DISCUSSION
Cause of deaths related to epilepsy can be classified into three main categories: (I) exacerbation of an underlying disease (cerebrovascular diseases, intracranial space-occupying lesions, etc.) inducing epilepsy, (II) exacerbation of a previous disease that does not induce epilepsy (infections, etc.), and (III) epilepsy directly causing the death (SE, accidents occurring during an attack, etc.) (14,15,16). To consider an epileptic attack as SE, repeated and continuing seizures should be seen during 30 min and the patient should not regain consciousness between seizures (17,18). SE represents a significant proportion of epileptic deaths; however, as a cause of death, it is not considered in the category of SUDEP. According to Nashef and Brown (9), a sudden epileptic death, which is a category of sudden and unexpected death causes, is the sudden and unexpected death of an epileptic patient regardless of the presence of a witness or its association with the attack. Additionally, as a rule of thumb, no SE or other toxicological–anatomical cause of death has been identified in the postmortem examination of SUDEP cases (9,10). In 1999, Annegers and Coan (19) reviewed SUDEP and referred to the six SUDEP criteria established by an advisory committee that had convened in 1993. The criteria are as follows: (I) the victim suffered from epilepsy, defined as recurrent unprovoked seizures; (II) the victim unexpectedly died while in a reasonable state of health; (III) death occurred “suddenly” (within minutes) when known; (IV) death occurred during normal activities and benign circumstances; (V) an obvious medical cause was not found; and (VI) death was not the direct result of a seizure or SE. Annegers and Coan (19) described two terms concerning SUDEP regarding these criteria: definite SUDEP and probable SUDEP. If a patient meets all six criteria and there are adequate postmortem data to determine the cause of death as “due to epilepsy,” it should be categorized as “definite SUDEP.” If a case meets all six criteria but there are no postmortem data, it should be categorized as “probable SUDEP.” Friedman and Hirsch (20) also mentioned probable SUDEP and added yet another term, “possible SUDEP”, which they described as follows. If an autopsy is not performed and there is no known alternative explanation for death, death should be described as “probable SUDEP.” If an autopsy is not performed and there is a competing explanation for death, death should be described as “possible SUDEP.” Nashef et al. (11) wrote a review to combine the SUDEP definitions. According to their review, deaths of epileptic patients could be classified into six groups: definite SUDEP/definite SUDEP plus, probable SUDEP/probable SUDEP plus, possible SUDEP, near-SUDEP/near-SUDEP plus, not SUDEP, and unclassified.
Despite these newly suggested detailed classifications, the term SUDEP in our study was used without any further classifications to be able to compare our findings with those in the already available literature. According to this point of view, SUDEP diagnoses in different studies are presented as follows. Barrow et al. (21) reported the cause of death as epilepsy-related conditions in 41 of 83 (49.40%) cases of autopsied patients with histories of epilepsy, while epilepsy-related deaths were noted as SUDEP, foreign-body aspiration and accidents that occurred during the attack. In the cases of autopsied patients with histories of epilepsy, Kloster and Engelskjøn (22) reported the cause of death as SUDEP in 42 of 79 (53.1%), Antoniuk et al. (23) in 20 of 53 (37.7%), and Opeskin et al. (24) in 50 of 357 (14%). Besides, Swinghamer et al. (25) directly presented two cases of SUDEP, while Lear-Kaul et al. (3) presented 67 cases, Nilsson et al. (26) presented 57 cases, and Shields et al. (27) presented 70 cases. In our study, epilepsy was diagnosed as the cause of death in 40 of the 112 (35.7%) cases with a history of epilepsy. The cause was not detected in 28 (25%) cases.
Various risk factors have been suggested as causative factors in SUDEP cases. Major factors include being males, being between 20 and 39 years of age, having early-onset and a long duration of epilepsy, having frequent attacks, the presence of generalized tonic–clonic attacks, the requirement of polytherapy with antiepileptics, low compatibility for antiepileptic medicine use, carbamazepine therapy, amygdala sclerosis, alcoholism, an intelligence quotient below 70, and a history of head trauma (3,20,22,26,28,29,30,31).
In previous studies, the ratio of male deaths due to SUDEP has been reported as 62.9% of 154 cases by Langan (28), 72% of 67 cases by Lear-Kaul et al. (3), 59.6% of 57 cases by Nilsson et al. (26), 54% of 50 cases by Opeskin et al. (24), 62% of 42 cases by Kloster and Engelskjøn (22), and 70% of 20 cases by Antoniuk et al. (23). Many articles have identified the male gender as a risk factor for SUDEP (20,31,32). Distribution of all our cases based on gender revealed that there were 74 males and 38 females.
The gender distribution of only SUDEP cases was as follows: 21 (52.5%) males and 19 (47.5%) females. Although the male-to-female ratio was approximately 2:1 among all our cases, there was equality in gender distribution among the SUDEP cases, indicating a difference with the literature.
Our age distribution of patients with a history of epilepsy differs somewhat from previous studies. A majority of the patients were between 36 and 45 years of age in the study by Nilsson et al. (26) 54% of 50 cases by Opeskin et al. (24) Sudden epileptic deaths, however, should not be limited to only a specific age group. A review of death certificates of epileptic patients by Appleton (5) demonstrated that in Liverpool, 97 children under 15 years of age died due to epilepsy or indirect epilepsy-related circumstances in 1993. Nashef et al. (33) followed 601 patients and reported that the mean age of the cohort was 32.5 years and the mean age of 24 patients at the time of death was 35 (range 18–73) years. The mean age of the patients with a cause of death identified as sudden epileptic death was 28.6 years. The mean age was reported as 35.5 years in the study by Lear-Kaul et al. (3). In our study, the mean age of all our patients was 34.2 (range 0–87) years. The mean age was 36.0 years for males and 30.9 years for females. The mean age of only SUDEP patients was 30.6 (range 9–60) years. Among these patients, the mean age was identified as 31.5 years in males and 29.6 years in females. In light of these findings, it can be concluded that epileptic deaths can be encountered in every age group. The young adult population, however, has a slightly increased risk for SUDEP, although statistical significance could not be reached in the comparison of SUDEP and non-SUDEP groups because younger age predominance in the non-SUDEP group is an expected phenomenon due to the presence of unnatural deaths.
Attack type and frequency are also among the important risk factors in sudden epileptic deaths. Annegers and Coan (19) reported that the risk is higher for individuals with acquired epilepsy than for those with idiopathic epilepsy. Previous studies reported a history of generalized tonic–clonic attack in majority of sudden epileptic death cases (28). No information, however, was obtained regarding the type of epileptic attacks, either from medical documentation or witness statements of our study.
According to the classification based on the circumstances surrounding death, a great number of epileptic deaths were reported to have been discovered at the home of the patient. The percentages are as follows: 87% by Lear-Kaul et al. (3), 77.5% by Coyle et al. (34), and 73.7% by Nilsson et al. (26). Among patients found dead at home in the study by Lear-Kaul et al. (3), 57% were found in the prone position (3). Kloster and Engelskjøn (22) also reported that the prone position is the predominantly encountered position. Langan (28) reported that a majority of patients were found dead on the bed. In our study, 21 of 40 (52.5%) patients who died from SUDEP were found dead without any witness present at the time of death. Of these, in accordance with the literature, 18 (40%) were found at home, two (5%) were found outside, and one (2.5%) was found at the workplace. Of the 18 patients found at home, five were found dead on the bed. Because some of the crime-scene investigation reports did not provide adequate information, however, one could assume that the number of patients found dead on the bed was inaccurate. When the other 19 (47.5%) cases were evaluated, it was seen that there were inadequate data for three (7.5%) of these cases; the remaining 16 patients were reported to have died either at home or on the way to hospital due to their current illness. Thus, it is thought that there was a witness to the death of these 16 patients.
External examination findings evoking the possibility of an attack at the time of or prior to death can be supporting details for epilepsy-related death findings, although SUDEP diagnosis is independent from attacks and such external examination findings are not specific to epilepsy. Lear-Kaul et al. (3) reported that 39 (58%) SUDEP patients had findings suggesting a previous attack (bite on the tongue, superficial skin injury, etc.). Coyle et al. (34) reported that there were bite marks or lacerations on the tongue in only 11 (27.5%) SUDEP cases. Shields et al. (27) reported that they encountered findings that included petechiae on the skin, contusion on the tongue or lips, and hyperplasia of the gingiva. In our study, such external examination findings could be shown in 63 (56.3%) of all cases and in 29 (72.5%) of the SUDEP cases. In other words, if those 40 SUDEP cases were excluded, similar external examination findings would still be observed in 34 (47.2%) of the remaining 72 non-SUDEP cases. Thus, the presence of findings suggestive of an epileptic attack in the external examination would not support SUDEP diagnosis, and additional supportive findings would be necessary.
In many SUDEP cases, postictal respiratory arrest or terminal cardiac arrhythmias are believed to be the mechanism of death (3,8). Langan (28) demonstrated that respiratory arrest and hypoventilation were involved in the etiopathogenesis of SUDEP, with a study considering deaths that occurred in the presence of an eyewitness. Swinghamer et al. (25) noted that the mechanism of death in SUDEP cases could be respiratory problems, cardiac disturbances or the loss of postictal preventive reflex mechanisms, and respiratory arrest. Similarly, in animal studies, Johnston et al. (35,36) noted respiratory mechanisms involved in death. Various studies conducted with an epileptic patient population showed that rhythm disturbances are detected with the ECG recording. Prolonged QT interval, ST depression, downward T wave, bradiarrhythmias, ventricular fibrillation and asistolia, atrial fibrillation, premature atrioventricular depolarization, sinus tachycardia, and supraventricular tachycardia can be listed among these disturbances (3,37,38). Internal examination findings of the brain, lungs, and heart related to the above-mentioned disturbances are presented in different studies. Lear-Kaul et al. (3) reported that pathological findings in the brain, which could explain the symptoms, were found only in four (6.0%) cases. Other findings were listed as congestion in the organs in 16 (23.8%) cases, pulmonary edema in 10 (14.9%), and both organ congestion and pulmonary edema in 29 (43.2%). In addition to these findings, hepatosteatosis was observed in 19 (28.3%) cases, cirrhosis in six (8.9%), and bacterial infection in two (2.9%) (3). Antoniuk et al. (23) reported brain edema in seven (35%) cases, pulmonary edema in eight (11.9%), and both brain and pulmonary edemas in one (5%). Barrow et al. (21) reported pulmonary edema in all their cases. Thom et al. (39) reported acute neuronal damage with immunohistochemical staining (HSP-70 and c-Jun) in the hippocampus of SUDEP cases. Kloster and Engelskjøn (22) showed no descriptive cause in SUDEP; they reported that pulmonary and brain edemas are the most frequently noted findings in autopsy reports. Shields et al. (27) reported that in addition to pulmonary edema, they encountered petechiae on the organs. In patients with pathological brain findings, they noted squeals, suggesting a previous traumatic incident; cortical cerebral and hippocampal atrophies; venous hemangioma; leptomeningeal varicosis; and tumor. Coyle et al. (34) reported that they found left ventricular hypertrophy in nine (22.5%) cases and no cardiovascular abnormality in 21 (52.5%) cases. Macroscopic or microscopic findings suggesting a possible epileptic focus in the brain were found in only 23 (20.5%) of our cases. Of 72 non-SUDEP cases, brain edema was found in five (6.9%), pulmonary edema in 23 (31.9%), and both pulmonary and brain edemas in 36 (50%). These results indicate that pulmonary and brain edemas were frequently seen as pathological findings in both groups. The presence of these two findings cannot be assumed significant for SUDEP; additional supportive findings are necessary.
A review article by So (31) highlighted studies in three major domains of potential mechanisms for SUDEP: cardiac, respiratory and autonomic. So (31) stated that preexisting cardiac disease is an important consideration for the potential cardiac basis of SUDEP. According to Eastaugh et al. (40), the most common etiologic mechanisms believed to be responsible for SUDEP are malignant cardiac arrhythmia due to seizure and asphyxia after a seizure. A combination of these mechanisms could also lead to cerebral hypoperfusion, which is the third mechanism of death. Davis and McGwin (41) states that “individuals dying of SUDEP might have large hearts, making them more susceptible to sudden cardiac death should the autonomic nervous system initiate a dysrhythmia.” In their 15 year-retrospective study, they found that the overall mean heart weight was 380 g, with a range of 195 to 860 g and a standard deviation of 97.4 g. They also noted that there was no significant difference in the mean heart weight between SUDEP and epileptic patients who died of any cause other than epilepsy. In addition, Schuele et al. (42) stated that fatal arrhythmias are thought to be the mechanism underlying the cardiac causes of SUDEP. A prevailing hypothesis is that a lethal cardiac arrhythmia is caused by epilepsy-induced autonomic discharges to the heart. The two main potentially lethal arrhythmias implicated in SUDEP are ictal ventricular tachyarrhythmias and ictal bradycardia/asystole. In our study of 112 epileptic cases, the microscopic examination of overweight hearts (n=69, 61.60%) revealed that hypertrophy was severe in 31 (27.6%) cases and mild in 10 (8.9%). In the other 71 (63.3%) cases, there were no signs of hypertrophy in the histological examination. In 19 of 40 (47.5%) SUDEP cases, the hearts were overweight and histological examination revealed hypertrophy in 11 (27.5%; 7 severe and 4 mild) cases (Table 4).
Another important issue to consider when interpreting these results is that if there were enough adequate cardiovascular findings for diagnosing the cause of death as cardiovascular disease, SUDEP could have been disregarded by the pathologist. In our study, the cause of death was determined as cardiovascular disease in 14 of the 112 (12.5%) cases. Deeper investigation of 8 of these 14 (57.1%) cases revealed fresh external findings that could be associated with an attack. Although these external findings cannot prove any mechanism, there may be still a possibility of a death due to post-seizure arrhythmia. In their autopsy study, P-Codrea Tigaran et al. (32) reported that increased levels of deep and subendocardial fibrosis are observed in SUDEP cases compared with controls; this may reflect the result of repetitive sympathetic activation or recurrent hypoxemia from seizures. They found fibrotic changes in the deep and subendocardial myocardium in 6 of 15 (40%) patients for whom histological examination could be performed. They also found fibrotic changes in the conduction system in none of their cases (32). In our study, in all 14 patients with a diagnosis for cause of death as cardiovascular disease, the hearts were overweight and histological examination revealed severe hypertrophy in 12 (85.7%) cases, while the mean age was 44.4±13.1 (range 32–77, median 40–41) years. The presence of hypertrophy and myocardial scar tissue findings in the microscopic examination was significantly more frequent among patients determined to have died from cardiovascular diseases than among those in the SUDEP group (p=0.001 for each finding). A severe hypertrophy ratio of 85.7% among these cardiovascular cases was remarkable, while the presence of at least one of the myocardial findings (i.e., microscopic hypertrophy, fibrosis, or myocardial scar tissue) and at least two myocardial findings together were significantly more frequent among patients determined to have died from cardiovascular diseases than among those in the SUDEP group (p=0.001 respectively; Table 4) These statistical results support the above-mentioned opinion suggesting that the presence of classical cardiovascular findings predominantly leads the expert to determine the cause of death directly through cardiovascular explanations. However, when considered beyond the statistical point of view, severe fibrosis observed in seven of our SUDEP cases infers that there can also be a doubt in the cause of death of these seven SUDEP cases because they might have died from only cardiovascular problems but were diagnosed as SUDEP. On the other hand, as observed in the study by P-Codrea Tigaran et al. (32), fibrosis can be a result of epileptic attacks. Fibrosis and other cardiac findings also as results of attacks in many epileptic patients make the differential diagnosis between SUDEP and cardiovascular deaths more difficult; however, it is important to note that scar tissue was observed only in one of our SUDEP patients. With this point of view, deaths due to cardiovascular disease in young adults require a deep medical investigation to reveal underlying causes. A common trait in our cases was epilepsy. Cardiovascular pathologies, including conduction system abnormalities, should therefore not be undervalued when investigating the death of a patient with a history of epilepsy. The cardiac conduction system was evaluated in none of our patients, and the cause of death was established only to the final reason; underlying factors were not investigated. Verma and Kumar (43), Leestma (44), and Coyle et al. (34) also emphasized the same point, noting that when determining the cause of death in patients with a history of epilepsy, clinicians or pathologists typically discover very few findings and end their bureaucratic responsibilities with unsatisfying diagnoses such as asphyxia or heart failure. In addition, Leestma (44) emphasized being alert to the probability of SUDEP when investigating the deaths of patients with a history of epilepsy, suggesting the use of a structured checklist for lay investigators. For medical examiners, Verma and Kumar (43) and Leestma (44) suggested a deep and complete examination of the heart, lungs, and brain.
Some aspects of antiepileptic medicines are also defined as risk factors for SUDEP. These risk factors are reported as poor patient compliance, multiple antiepileptic agent use (3,26,29,30), and carbamazepine therapy (3). Antoniuk et al. (23) found that 13 (65%) patients were on antiepileptics, and of these, nine (45%) were on monotherapy (phenobarbital, carbamazepine or diphenylhydantoin) and four (20%) were on polytherapy (phenobarbital+carbamazepine or phenobarbital+diphenylhydantoin). Coyle et al. (34) reported that 10 (25%) patients were on carbamazepine and eight (20%) were on phenytoin. Kloster and Engelskjøn (22) found that a majority of their SUDEP patients were on carbamazepine, phenobarbital, or phenytoin. In our study, toxicological analysis was performed in 105 of the 112 (93.7%) patients with a history of epilepsy; of these patients, antiepileptic agents were detected in 44 (41.9%) and no antiepileptics were detected in 61 (58.1%). The ratio of being under medication was not significantly different between the SUDEP and cardiovascular disease groups. In 40 SUDEP cases, 38 (95%) patients underwent toxicological analysis and no antiepileptic agent was detected in 21 (55.3%) of these. In the other 17 (42.5%) patients, at least one antiepileptic agent was detected; a single agent was present in 12 (40%) of these patients, and multiple antiepileptic agents were detected in the other 5 (12.5%) patients. These results indicate that even though the patients were epileptic, 21 (55.3%) were not under antiepileptic medication at the time of death (Table 5, Table 6). This implies that the inconsistent use or disuse of antiepileptic medicines is a greater risk factor for SUDEP than polytherapy. Besides, in cases where antiepileptic medicines were used, therapies used should be assessed for their efficacy in the prevention of generalized tonic–clonic attacks and for their potential risk (45).
In conclusion, parameters such as sociodemographic features; medical antecedent; witness statements; external examination findings; histopathological findings including those from the examination of the cerebrum, cerebellum, and brain stem (i.e., yellow–brown plaques, space-occupying lesions, infections, or hemorrhage), those of the heart (i.e., cardiac overweight, conduction pathways, or coronary lumens), petechial bleeding foci on the visceral surfaces, particularly on interlobar surfaces of the lungs, and pulmonary edema as signs of possible hypoxia; and toxicological findings including the presence of an antiepileptic agent and type of antiepileptic therapy should be investigated together in the evaluation of the cause of death of epileptic patients because none of these factors could be proved to have a diagnostic value when presented alone. Additionally, for the differential diagnosis between SUDEP and cardiovascular deaths, cardiac findings should be carefully noted and considered in a detailed manner.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of f The Ministry of Justice Council of Forensic Medicine (Date: 12/03/2013, No: 132).
Informed Consent: Informed consent was not received due to the retrospective nature of the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.N.A.; Design - M.N.A., İ.E.M., D.O.M.; Supervision - S.K.; Resource - S.K.; Materials - M.N.A., D.O.M., S.K.; Data Collection and/or Processing - A.N.Ş., M.N.A., D.O.M., İ.E.M.; Analysis and/or Interpretation - M.N.A., İ.E.M.; Literature Search - İ.E.M., M.N.A.; Writing - İ.E.M. M.N.A.; Critical Reviews - İ.E.M.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Thom M. The autopsy in sudden unexpected adult death: epilepsy. Curr Diagn Pathol. 2007;13:389–400. https://doi.org/10.1016/j.cdip.2007.05.004. [Google Scholar]
- 2.Fisher RS, Boas WvE, Blume W, Elger C, Genton P, Lee P, Engel J. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE) Epilepsia. 2005;46:470–472. doi: 10.1111/j.0013-9580.2005.66104.x. https://doi.org/10.1111/j.0013-9580.2005.66104.x. [DOI] [PubMed] [Google Scholar]
- 3.Lear-Kaul KC, Coughlin L, Dobersen MJ. Sudden unexpected death in epilepsy: a retrospective study. Am J Forensic Med Pathol. 2005;26:11–17. doi: 10.1097/01.paf.0000154453.58795.18. https://doi.org/10.1097/01.paf.0000154453.58795.18. [DOI] [PubMed] [Google Scholar]
- 4.Hauser WA, Annegers JF, Elveback LR. Mortality in patients with epilepsy. Epilepsia. 1980;21:399–412. doi: 10.1111/j.1528-1157.1980.tb04088.x. https://doi.org/10.1111/j.1528-1157.1980.tb04088.x. [DOI] [PubMed] [Google Scholar]
- 5.Appleton RE. Sudden, unexpected death in epilepsy in children. Seizure. 1997;6:175–177. doi: 10.1016/s1059-1311(97)80002-7. https://doi.org/10.1016/S1059-1311(97)80002-7. [DOI] [PubMed] [Google Scholar]
- 6.Shorvon SD. The epidemiology and treatment of chronic and refractory epilepsy. Epilepsia. 1996;37(Suppl 2):1–3. doi: 10.1111/j.1528-1157.1996.tb06027.x. https://doi.org/10.1111/j.1528-1157.1996.tb06027.x. [DOI] [PubMed] [Google Scholar]
- 7.Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia. 2000;41(Suppl 2):7–12. doi: 10.1111/j.1528-1157.2000.tb01519.x. https://doi.org/10.1111/j.1528-1157.2000.tb01519.x. [DOI] [PubMed] [Google Scholar]
- 8.So EL, Sam MC, Lagerlund TL. Postictal central apnea as a cause of SUDEP: evidence from near-SUDEP incident. Epilepsia. 2000;41:1494–1497. doi: 10.1111/j.1528-1157.2000.tb00128.x. https://doi.org/10.1111/j.1528-1157.2000.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 9.Nashef L, Brown S. Epilepsy and sudden death. Lancet. 1996;348:1324–1325. doi: 10.1016/S0140-6736(05)65402-5. https://doi.org/10.1016/S0140-6736(05)65402-5. [DOI] [PubMed] [Google Scholar]
- 10.Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. 1997;38(Suppl 11):6–S8. doi: 10.1111/j.1528-1157.1997.tb06130.x. https://doi.org/10.1111/j.1528-1157.1997.tb06130.x. [DOI] [PubMed] [Google Scholar]
- 11.Nashef L, So EL, Ryvin P, Tomson T. Unifying the definitions of sudden unexpected death in epilepsy. Epilepsia. 2012;53:227–233. doi: 10.1111/j.1528-1167.2011.03358.x. https://doi.org/10.1111/j.1528-1167.2011.03358.x. [DOI] [PubMed] [Google Scholar]
- 12.Zeek PM. The weight of normal human heart. Arch Pathol. 1942;34:820–832. [Google Scholar]
- 13.Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD. Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc. 1988;63(2):137–146. doi: 10.1016/s0025-6196(12)64946-5. https://doi.org/10.1016/S0025-6196(12)64946-5. [DOI] [PubMed] [Google Scholar]
- 14.Nilsson L, Tomson T, Farahmand BY, Diwan V, Persson PG. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia. 1997;38:1062–1068. doi: 10.1111/j.1528-1157.1997.tb01194.x. https://doi.org/10.1111/j.1528-1157.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 15.Iivanainen M, Lehtinen J. Causes of death in institutionalized epileptics. Epilepsia. 1979;20:485–491. doi: 10.1111/j.1528-1157.1979.tb04830.x. https://doi.org/10.1111/j.1528-1157.1979.tb04830.x. [DOI] [PubMed] [Google Scholar]
- 16.Annegers J. Cardiac deaths in epilepsy. Epilepsia. 1997;38(Suppl 11):23–S25. doi: 10.1111/j.1528-1157.1997.tb06119.x. https://doi.org/10.1111/j.1528-1157.1997.tb06119.x. [DOI] [PubMed] [Google Scholar]
- 17.Lowenstein DH. Status epilepticus: An overview of the clinical problem. Epilepsia. 1999;40(Suppl 1):3–8. doi: 10.1111/j.1528-1157.1999.tb00872.x. https://doi.org/10.1111/j.1528-1157.1999.tb00872.x. [DOI] [PubMed] [Google Scholar]
- 18.Towne AR, Pellock JM, Ko D, DeLorenzo RJ. Determinants of mortality in status epilepticus. Epilepsia. 1994;35:27–34. doi: 10.1111/j.1528-1157.1994.tb02908.x. https://doi.org/10.1111/j.1528-1157.1994.tb02908.x. [DOI] [PubMed] [Google Scholar]
- 19.Annegers JF, Coan SP. SUDEP: overview of definitions and review of incidence data. Seizure. 1999;8:347–352. doi: 10.1053/seiz.1999.0306. https://doi.org/10.1053/seiz.1999.0306. [DOI] [PubMed] [Google Scholar]
- 20.Friedman D, Hirsch LJ. Sudden unexpected death in epilepsy - an overview of current understanding and future perspectives. Eur Neurol Rev. 2012;7:64–71. https://doi.org/10.17925/ENR.2012.07.01.67. [Google Scholar]
- 21.Barrow M, Roberts IS, Soilleux EJ. Sudden death in epilepsy: standards of reporting and the value of toxicological analysis. J Clin Pathol. 2011;64:1025–1028. doi: 10.1136/jclinpath-2011-200109. https://doi.org/10.1136/jclinpath-2011-200109. [DOI] [PubMed] [Google Scholar]
- 22.Kloster R, Engelskjøn T. Sudden unexpected death in epilepsy (SUDEP): a clinical perspective and a search for risk factors. J Neurol Neurosurg Psychiatry. 1999;67:439–444. doi: 10.1136/jnnp.67.4.439. https://doi.org/10.1136/jnnp.67.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antoniuk SA, Oliva LV, Bruck I, Malucelli M, Yabumoto S, Castellano JL. Sudden unexpected, unexplained death in epilepsy autopsied patients. Arq Neuropsiquiatr. 2001;59:40–45. doi: 10.1590/s0004-282x2001000100009. https://doi.org/10.1590/S0004-282X2001000100009. [DOI] [PubMed] [Google Scholar]
- 24.Opeskin K, Harvey AS, Cordner SM, Berkovic SF. Sudden unexpected death in epilepsy in Victoria. J Clin Neurosci. 2000;7:34–37. doi: 10.1054/jocn.1999.0137. https://doi.org/10.1054/jocn.1999.0137. [DOI] [PubMed] [Google Scholar]
- 25.Swinghamer J, Devinsky O, Friedman D. Can post-ictal intervention prevent sudden unexpected death in epilepsy? a report of two cases. Epilepsy Behav. 2012;24:377–379. doi: 10.1016/j.yebeh.2012.04.122. https://doi.org/10.1016/j.yebeh.2012.04.122. [DOI] [PubMed] [Google Scholar]
- 26.Nilsson L, Farahmand BY, Persson PG, Thiblin I, Tomson T. Risk factors for sudden unexpected death in epilepsy: a case-control study. Lancet. 1999;353:888–893. doi: 10.1016/s0140-6736(98)05114-9. https://doi.org/10.1016/S0140-6736(98)05114-9. [DOI] [PubMed] [Google Scholar]
- 27.Shields LBE, Hunsaker DM, Hunsaker JCI, Parker JCJ. Sudden unexpected death in epilepsy: neuropathologic findings. Am J Forensic Med Pathol. 2002;23:307–314. doi: 10.1097/00000433-200212000-00001. https://doi.org/10.1097/00000433-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Langan Y. Sudden unexpected death in epilepsy (SUDEP): risk factors and case control studies. Seizure. 2000;9:179–183. doi: 10.1053/seiz.2000.0388. https://doi.org/10.1053/seiz.2000.0388. [DOI] [PubMed] [Google Scholar]
- 29.Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, Walczak TS, Beghi E, Brodie MJ, Hauser A. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52:1150–1159. doi: 10.1111/j.1528-1167.2010.02952.x. https://doi.org/10.1111/j.1528-1167.2010.02952.x. [DOI] [PubMed] [Google Scholar]
- 30.Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol. 2008;7:1021–1031. doi: 10.1016/S1474-4422(08)70202-3. https://doi.org/10.1016/S1474-4422(08)70202-3. [DOI] [PubMed] [Google Scholar]
- 31.So EL. What is known about the mechanisms underlying SUDEP? Epilepsia. 2008;49:93–98. doi: 10.1111/j.1528-1167.2008.01932.x. https://doi.org/10.1111/j.1528-1167.2008.01932.x. [DOI] [PubMed] [Google Scholar]
- 32.P-Codrea Tigaran S, Dalager-Pedersen S, Baandrup U, Dam M, Vesterby-Charles A. Sudden unexpected death in epilepsy: is death by seizures a cardiac disease? Am J Forensic Med Pathol. 2005;26:99–105. [PubMed] [Google Scholar]
- 33.Nashef L, Fish D, Sander J, Shorvon S. Incidence of sudden unexpected death in an adult outpatient cohort with epilepsy at a tertiary referral centre. J Neurol Neurosurg Psychiatry. 1995;58:462–464. doi: 10.1136/jnnp.58.4.462. https://doi.org/10.1136/jnnp.58.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coyle HP, Baker-Brian N, Brown SW. Coroners’ autopsy reporting of sudden unexplained death in epilepsy (SUDEP) in the UK. Seizure. 1994;3:247–254. doi: 10.1016/s1059-1311(05)80171-2. https://doi.org/10.1016/S1059-1311(05)80171-2. [DOI] [PubMed] [Google Scholar]
- 35.Johnston SC, Horn JK, Valente J, Simon RP. The role of hypoventilation in a sheep model of epileptic sudden death. Ann Neurol. 1995;37:531–537. doi: 10.1002/ana.410370416. https://doi.org/10.1002/ana.410370416. [DOI] [PubMed] [Google Scholar]
- 36.Johnston SC, Siedenberg R, Min JK, Jerome EH, Laxer KD. Central apnea and acute cardiac ischemia in a sheep model of epileptic sudden death. Ann Neurol. 1997;42:588–594. doi: 10.1002/ana.410420409. https://doi.org/10.1002/ana.410420409. [DOI] [PubMed] [Google Scholar]
- 37.Opherk C, Coromilas J, Hirsch LJ. Heart rate and EKG changes in 102 seizures: analysis of influencing factors. Epilepsy Res. 2002;52:117–127. doi: 10.1016/s0920-1211(02)00215-2. https://doi.org/10.1016/S0920-1211(02)00215-2. [DOI] [PubMed] [Google Scholar]
- 38.Stöllberger C, Finsterer J. Cardiorespiratory findings in sudden unexplained/unexpected death in epilepsy (SUDEP) Epilepsy Res. 2004;59:51–60. doi: 10.1016/j.eplepsyres.2004.03.008. https://doi.org/10.1016/j.eplepsyres.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 39.Thom M, Seetah S, Sisodiya S, Koepp M, Scaravilli F. Sudden and unexpected death in epilepsy (SUDEP): evidence of acute neuronal injury using HSP-70 and c-Jun immunohistochemistry. Neuropathol Appl Neurobiol. 2003;29:132–143. doi: 10.1046/j.1365-2990.2003.00452.x. https://doi.org/10.1046/j.1365-2990.2003.00452.x. [DOI] [PubMed] [Google Scholar]
- 40.Eastaugh A, Thompson T, Vohra J, O’Brien T, Winship I. Sudden unexpected death, epilepsy and familial cardiac pathology. J Clin Neurosci. 2015;22:1594–1600. doi: 10.1016/j.jocn.2015.05.002. https://doi.org/10.1016/j.jocn.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 41.Davis GG, McGwin G. Comparison of heart mass in seizure patients dying of sudden unexplained death in epilepsy to sudden death due to some other cause. Am J Forensic Med Pathol. 2004;25:23–28. doi: 10.1097/01.paf.0000113930.53578.f8. https://doi.org/10.1097/01.paf.0000113930.53578.f8. [DOI] [PubMed] [Google Scholar]
- 42.Schuele SU, Widdess-Walsh P, Bermeo A, Lüders HO. Sudden unexplained death in epilepsy: the role of the heart. Cleve Clin J Med. 2007;74(Suppl 1):121–127. doi: 10.3949/ccjm.74.suppl_1.s121. https://doi.org/10.3949/ccjm.74.Suppl_1.S121. [DOI] [PubMed] [Google Scholar]
- 43.Verma A, Kumar A. Sudden unexpected death in epilepsy: some approaches for its prevention and medicolegal consideration. Acta Neurol Belg. 2015;115:207–212. doi: 10.1007/s13760-014-0362-3. https://doi.org/10.1007/s13760-014-0362-3. [DOI] [PubMed] [Google Scholar]
- 44.Leestma JE. Forensic considerations in sudden unexpected death in epilepsy. Epilepsia. 1997;38(Suppl 11):63–66. doi: 10.1111/j.1528-1157.1997.tb06132.x. https://doi.org/10.1111/j.1528-1157.1997.tb06132.x. [DOI] [PubMed] [Google Scholar]
- 45.Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, Walczak TS, Beghi E, Brodie MJ, Hauser WA. Do antiepileptic drugs or generalized tonic-clonic seizure frequency increase SUDEP risk? a combined analysis. Epilepsia. 2012;53:249–252. doi: 10.1111/j.1528-1167.2011.03354.x. https://doi.org/10.1111/j.1528-1167.2011.03354.x. [DOI] [PubMed] [Google Scholar]


