Abstract
Purpose
Sedentary behavior has been identified as a major health risk. While interventions to reduce time spent sedentary have become increasingly prevalent, the vast majority of this work in adults has been focused on workplace sedentary behavior, and often pairs sedentary reduction interventions with increasing physical activity. As research designed to specifically decrease sedentary time that is not limited to the workplace becomes available, identifying strategies and approaches, along with feasibility and efficacy of these interventions, is warranted.
Methods
Electronic databases were searched for sedentary interventions with eligibility criteria including: (a) interventions designed to explicitly reduce sedentary behavior that were not limited to the workplace, (b) outcomes specific to sedentary behavior, (c) adults aged at least 18 years, and (d) written in English.
Results
A total of 767 full-text manuscripts were identified, with thirteen studies meeting all eligibility criteria. While intervention characteristics and methodological quality varied greatly among studies, ten of the thirteen studies observed a significant reduction in objectively measured sitting time post-intervention. In those studies that collected participant feasibility/acceptability data, all reported that the intervention was viewed as “favorable to very favorable,” would use again, and that participant burden was quite low, suggesting that these interventions were feasible.
Conclusion
Sedentary behavior interventions not limited to the workplace appear to be largely efficacious. While results varied with respect to the magnitude of the decrease in time spent sedentary, they are encouraging. However, due to the small body of evidence and the variability of study designs, our ability to make overarching statements regarding “best practices” at this time is limited. Well-controlled trials of longer duration with larger samples, using theoretically-based interventions with consistent prescriptions for limiting sedentary time are needed.
Keywords: sitting, health promotion, adults, behavior change
Sedentary behavior, defined as waking activities performed while sitting or reclining that do not substantially increase energy expenditure above resting (6), has gained increased attention in the research community as an important predictor of health outcomes. Prolonged time spent sedentary is associated with an increased risk of obesity, metabolic syndrome, type II diabetes, cancer, depression and anxiety disorders, and all-cause mortality (27–29). Further, there is evidence that the health consequences of accumulating large amounts of sedentary time may be independent of the risks associated with inadequate physical activity (8) and the benefits of achieving physical activity recommendations (24). As such, interventions specifically targeted at decreasing sedentary time are warranted.
Sedentary interventions conducted to date in adults have utilized a variety of approaches and techniques with varying levels of success in their feasibility and effectiveness, as documented in previous review papers (7, 13, 19, 25, 26 ). These reviews have addressed contexts including (a) worksite interventions specifically targeting sedentary time, (b) non-worksite interventions addressing physical activity and sedentary time, and (c) non-worksite interventions that addressed physical activity but also measured sedentary behavior as a secondary outcome. Given that adults spend much of their leisure time in sedentary pursuits (20), non-worksite interventions are of substantial public health importance. This is particularly true given that sedentary time increases as people age and retire from the workforce (20). Thus, information is needed regarding best practices specific to limiting sedentary time across domains. Further, reviews by both Gardner et al. (13) and Prince et al. (25) suggest that interventions focusing solely on sedentary time may be more efficacious for reducing sitting compared to those that target both physical activity and sedentary behavior. Until quite recently, however, few of these interventions had been published outside of the context of worksites. As such, this review focuses on interventions specifically designed to decrease sedentary time that are not limited to the workplace. The purpose of this review is to discuss the characteristics, strategies, and approaches of existing sedentary interventions as well as the associated feasibility, acceptability, and efficacy of these interventions.
Methods
Study Selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (21) statement guided this systematic review. Studies were eligible for inclusion if they met the specific a priori criteria related to study population, design, intervention, and outcomes as detailed below.
Study Population
Adults over the age of 18. As this was the only eligibility criteria designated for inclusion, both “healthy” populations and populations with defined comorbidities (specifically, those identified as overweight, obese, and/or diagnosed with diabetes) were included in this review.
Interventions
Interventions designed to explicitly reduce sedentary behavior; those attempting to reduce time spent sedentary by increasing physical activity, solely or in conjunction with limiting sedentary time were excluded.
Intervention location
Interventions that were not specifically designed to limit sedentary time in the workplace were included. Of note, interventions could still incorporate strategies to limit occupational sedentary behavior, but those could not be the focus of the intervention. Rather, interventions included here were specifically designed to limit sedentary time throughout the day, regardless of the setting.
Outcomes
All interventions that measured sedentary behavior as an outcome (primary or secondary) were included. As such, sedentary behavior could be quantified in a number of ways, including (but not limited to): total time (minutes) spent in sedentary activities (metabolic equivalents, [or METs] ≤ 1.5), number of breaks interrupting prolonged sitting time (typically defined as ≥30 minutes), sedentary time accrued in prolonged bouts (typically defined as ≥30 minutes), sit-to-stand transitions, and percentage of daily waking hours spent sedentary. Assessment of sedentary behavior could be either self-reported or objectively measured. Feasibility (including enrollment, retention, reach, acceptability, participant satisfaction, and preference of the intervention,) efficacy, and effectiveness outcomes were all included.
Study Design
There were no restrictions specifically placed on study design. All methodological approaches were included as long as all other eligibility criteria were met.
Other Inclusion Criteria
Studies had to be peer-reviewed, full-text articles and written in English.
Data Sources and Search Criteria
An electronic search was performed using the following databases: PubMed, Web of Science, Google Scholar, PsycINFO, and SPORTDiscus. The search strategy applied to these databases included “adult”, “intervention” studies (pre-post, quasi-experimental or randomized designs) to “reduce sedentary behavior”, “sedentary lifestyle”, or “sitting time”, and “health behavior.” No date limits were set. Complete search terms used for each database are provided online (see Appendix, SDC 1, search terms listed by database). Reference lists of recent sedentary behavior reviews and relevant studies were also individually cross-referenced by research staff to identify studies that may have been missed by the electronic searches (7, 13, 25).
Study Selection
Two reviewers independently screened all titles and abstracts for initial inclusion. After this initial review, full text of all articles determined to be eligible were screened for inclusion. An additional independent reviewer was consulted with any eligibility disagreements.
Data Extraction
Using the PRISMA checklist as a reference (21), data from the following categories were extracted:
General: Author, date
Study Population: Number of participants, baseline demographic characteristics (i.e., age, gender, health status)
Intervention: Characteristics of intervention including: setting, length, mode of intervention, mention of specific behavioral theory, technological component of intervention
Study Design & Analyses: Treatment allocation, specified eligibility criteria, if intention-to-treat analyses were used
Outcome measures: Primary outcomes, secondary outcomes, if point estimates and measures of variability were presented, feasibility, acceptability, measurement of sedentary behavior (objective vs. self-report)
Data Synthesis and Quality Assessment
The studies included in this analysis were quite diverse in regards to their methodological and analytical approaches, study design, population, and intervention characteristics. In keeping with recommendations by the PRISMA statement (21), we concluded that meta-analysis was not appropriate. Rather, we addressed the methodological merit of these works using two separate strategies. First, we used a quality rating adapted from the Delphi list (as described in Table 3 of Verhagen et al. (30)) to quantitatively analyze the randomized controlled trials in our study, as this metric has been used in previous sedentary behavior intervention reviews (7, 13). Briefly, the Delphi list consists of a series of criteria specific to the design of a study as it relates to the external and internal validity, validity of the outcome, and of the statistical model used (30). Criteria were given a score based on answers to the associated questions (“yes”=1, “no” or “don’t know” (insufficient information present) =0). A total quality score ranging from 0–7 was then generated for each study. A second reviewer independently scored each study. In instances where consensus was not met between reviewers, a third reviewer was consulted. Second, as the Delphi criteria were designed to specifically evaluate the methodological quality of randomized controlled trials, questions on the metric were not always applicable to the other study designs included in this review. Therefore, we describe the merit of non-randomized trials in the context of, and relation to, randomized controlled trials.
Interventions were also assessed based on characteristics likely to be important in changing behavior, including the use of behavioral theory in designing the intervention, as well as the total duration of the intervention. Additionally, we also assessed the use of objective measures of sedentary time, as well as integration of a technological component to the intervention. Finally, data regarding efficacy and effectiveness for reducing sedentary time, along with feasibility and acceptability data, were discussed when available.
Results
Study Characteristics & Design
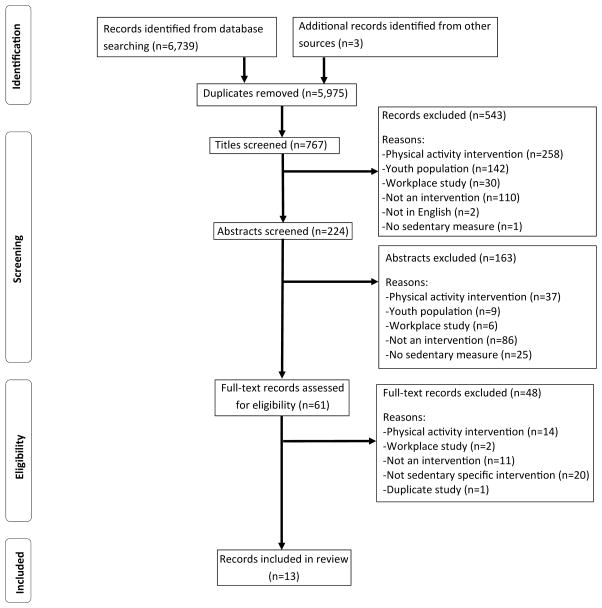
The results of our literature search using a PRISMA-style flow diagram (21) can be found in Figure 1. A total of 767 titles of full-text manuscripts were initially identified for eligibility assessment. After removing duplicate studies (n=1) and excluding studies from the analysis which: were in non-adult populations (n=151), were not interventions (n=207), specifically targeted physical activity (n=329), were workplace-based interventions (n=38), did not incorporate a measure of sedentary behavior (n=26), or were not written in English (n=2), thirteen studies met all eligibility criteria and were included in this review. Full study characteristics for these interventions are detailed in Table 1. Of the thirteen studies, seven were randomized controlled trials (1, 3, 9, 14, 16, 17, 22), five utilized a single-sample ‘pre-post’ design (4, 10, 11, 18, 23), and one used a quasi-experimental (non-randomized) design consisting of a post hoc addition to a larger observational study (15).
Figure 1.
Flow diagram of search results and reasons for exclusion
Table 1.
Study characteristics of non-worksite based interventions to reduce sedentary behavior
| Study | n | Study Population | Mean Age (SD); Percent Female | Intervention | Study Design | Duration/Follow-up Period | Measure of Sedentary Time | Behavioral Theory Used* | Tech Component of Intervention |
|---|---|---|---|---|---|---|---|---|---|
| Otten (22) | 36 | Overweight or obese adults ǂ | 42.6 (±13.3); 69% | Reduce TV time via electronic lockout system | RCT | 3 weeks/N/A | Sensewear armband | N/A | TV lockout system |
| Gardiner (11) | 59 | Healthy Older adults (≥60 yrs) | 74.3 (±9.3); 75% | Reduce sedentary time via goal setting/education, etc. | Pre-Post | 7 days/N/A | Actigraph | Social cognitive theory, behavioral choice theory | Review of accelerometer-assessed sedentary time from previous day |
| Fitzsimons (10) | 24 | Healthy Older Adults (≥60 yrs) | 68.0 (±6); 42% | Reduce sedentary time via education/Behavior Change Techniques | Pre-Post | 24 days/N/A/ | ActivPAL | Ecological model + “successful Behavior Change Techniques” | Incorporated visual sedentary time feedback from ActivPAL |
| Aadahl (1) | 166 | Healthy adults (Health 2010 participants) | 52.0 (±14.1); 53% | Reduce sedentary time via motivational counseling | RCT | 6 months (4 visits)/N/A | ActivPAL | Behavioral Choice Theory (goal-setting, self-efficacy, Motivational Interviewing) | N/A |
| Bond (4) | 30 | Overweight or obese adults ǂ | 47.5 (±13.5); 83% | Reduce sedentary time via real-time smartphone feedback, prompting, goal-setting; 3 strategies tested | Pre-Post | 4 weeks/N/A | Sensewear Mini armband | N/A | Smartphone app with onboard accelerometer |
| Biddle (3) | 187 | Overweight or obese young adults (18–40 yrs) w/>1 additional risk factor for DM ǂ | 32.8 (±5.6); 69% | Education workshop, self-monitoring tool (Gruve), motivational call | RCT | 12 months/N/A | Actigraph & ActivPAL | N/A | Self-monitoring wearable device (Gruve) |
| Judice (14) | 10 | Overweight or obese employed adults ǂ | 50.4 (±11.5); 50% | Education, goal setting, pedometer, PC screen prompts | Cross-over RCT | 1 week/N/A | Actigraph & ActivPAL | N/A | Pedometer; PC-based screen prompt |
| Lang (17) | 819 | Adult PA conference attendees | N/A;N/A | Point-of-decision-prompt | RCT | One hour session/N/A | Direct observation | N/A | N/A |
| Pellegrini (23) | 9 | Adults (21–70 yrs) w/DM | 53.1 (±10.7); 77% | Smartphone application w/haptic feedback | Pre-Post | 1 month/N/A | Actigraph & Shimmer | N/A | Smartphone app (visual and sensory feedback) with separate wearable accelerometer |
| Ellingson (9) | 30 | Healthy young adults (18–26) | 20.1 (±1.5); 50% | Reduce sedentary time w/real-time feedback via wearable technology | RCT-pilot | 5 Weeks/4-weeks | ActivPAL/Sedentary Behavior Questionnaire | Habit Theory of Behavior Change | Haptic feedback from ActivPAL |
| Kendzor (15) | 215 | Healthy adults | 43.9 (±12.9); 68% | Educational materials/Smartphone app w/daily messages | Quasi-Experimental (non-random) | 7 days/N/A | Actigraph & IPAQ | N/A | Smartphone app w/screen prompt |
| Kerr (16) | 30 | Non-working adults (50–70 yrs) | 60.4 (±5.9); 73% | Education, goal setting, “choice of other tools” | RCT-pilot | 2 Weeks/N/A | ActivPAL | Multiple Behavior Change strategies (self-monitoring, goal setting, feedback, etc.) | Multiple: Smartphone & PC app w/prompt; timers, watches, haptic feedback, branded bracelets, standing desks, etc. |
| Lewis (18) | 30 | Non-working older adults (≥60 yrs) | 71.7 (±6.5); 63% | 1-hr face-to-face Education/goal setting session |
Pre-post | 7 days/N/A | ActivPAL | Self-determination Theory | N/A |
While some of these interventions appear to be theoretically driven, there was no specific mention of behavioral theories. Thus, we did not want to make assumptions that these interventions were designed based on a particular behavioral theory.
Overweight/Obese participants = body mass index ≥25kg/m2. Abbreviations: N/A = Not Applicable; RCT = Randomized Controlled Trial; SD = Standard Deviation; w/ = with.
Samples
Sample sizes ranged from n=9 (23) to n=819 (17). Although only adults were included, some studies focused specifically on either younger (18–40 years) (3, 9) or older adults (≥60 years) (10, 11, 18); therefore, mean age ranged greatly between studies (mean ages: 20.1 years to 74.3 years). Further, five studies focused specifically on healthy adults (1, 9–11, 15), four on overweight and obese adults (BMI ≥25 kg/m2) (3, 4, 14, 22), and two on adults with either diabetes (23) or risk factors for diabetes (3). All studies included both males and females, although eight of the included 13 interventions had a majority (>50%) of female participants (1, 3, 4, 11, 15, 16, 18, 22, 23).
Methodological Quality Assessment for Randomized Controlled Trials
Strong inter-rater agreement (94%) was observed. Study characteristics for the randomized controlled trials (n=7) as they relate to the Delphi scale can be found in Table 2. While no trial received a score of 7 out of 7, four received a score of 6 out of 7 (1, 3, 16, 22), two scored a 4 out of 7 (9, 14), and one received a score of 2 out of 7 (17).
Table 2.
Quality ratings using criteria from the Delphi list (Verhagen et al., 1998) for randomized controlled trials of interventions to reduce sitting-time in non-workplace settings
| Criteria | Otten (22) | Aadahl (1) | Biddle (3) | Judice (14) | Lang (17) | Ellingson (9) | Kerr (16) | |
|---|---|---|---|---|---|---|---|---|
| 1a | Was a method of randomization performed? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 1b | Was the treatment allocation concealed? | Yes | Yes | Yes | ? | No | ? | Yes |
| 2 | Were the groups similar at baseline? | Yes | Yes | Yes | No | ? | Yes | Yes |
| 3 | Were the eligibility criteria specified? | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 4 | Was the outcome assessor blinded? | ? | Yes | ? | ? | No | No | No |
| 5* | Was the care provider/interventionist blinded? | - | - | - | - | - | - | - |
| 6* | Was the patient/participant blinded? | - | - | - | - | - | - | - |
| 7 | Were the point estimate and measures of validity presented for the primary outcome measures? | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8 | Did the analysis include an intention-to-treat analysis? | Yes | No | Yes | Yes | ? | No | Yes |
| Total score | 6 | 6 | 6 | 4 | 2 | 4 | 6 | |
Scoring: Y=yes=1, N=no=0,? =unclear=0; maximum score=7; Inter-rater agreement: 94%
These criteria were omitted from the final quality assessment score as they were thought to be inappropriate for application to sedentary behavior interventions. Blinding of interventionists and participants in this type of intervention is usually not possible and none of the studies included in this review fulfilled these criteria.
Methodological Quality Assessment for non- Randomized Controlled Trials
In regards to the non-randomized controlled trials reviewed in this analysis (n=6) (4, 10, 11, 15, 18, 23), it should be noted that these studies should be considered to have lower methodological quality to that of the randomized controlled trials. Specifically, we note that potential biases are likely to be greater for these studies when compared with the randomized trials, regardless of the latter’s score on the Delphi scale as described above. However, with regards to specific Delphi criteria, we did observe that all six studies had defined and specified eligibility criteria, had systematically collected outcome data and provided appropriate point estimates and validity measures for primary outcomes, with five (4, 10, 11, 18, 23) utilizing study designs that were prospective in nature.
Intervention Characteristics and Quality
All interventions included were intended to decrease time spent sedentary, whether discussed as a primary (n=12) or secondary outcome (n=1) (22). Of these, nine studies (1, 3, 4, 9, 10, 14, 16, 18, 23) also specifically incorporated adding breaks in prolonged sitting time with sit-to-stand transitions. However, the prescription/goals for sedentary time reduction, as well as the number of breaks in sedentary time, differed between studies. The majority of studies (n=8) did not utilize specific goals regarding time spent sedentary or number of breaks. Of the studies that did specifically give participants explicit time targets, they varied from reducing TV viewing time by 50% (22), interrupting sitting time every 20 (23), 30 (1, 4), or 60–120 minutes (4), accumulating 30 additional sit-to-stand transitions per day (16), to two (16) or three hours (14) of total daily sedentary reduction. The duration of these interventions also varied greatly among studies, ranging from one study utilizing a one-time, one hour session (17), four studies with interventions lasting one week (11, 14, 15, 18), and one study lasting 12 months (3).
With respect to the theoretical makeup of these interventions, six of the thirteen studies explicitly incorporated a behavioral theory into the design of the intervention (1, 9–11, 16, 18). While other studies appeared to be theoretically driven, there was no specific mention of use of behavioral theories. Thus, we chose not to make assumptions that these interventions were based on a particular theory and were therefore not included in our quality assessment. Six of the studies reviewed utilized a technological component as the basis of their intervention (3, 4, 14, 15, 22, 23), three (1, 17, 18) utilized behavior change techniques such as goal setting/education and point-of-decision-prompt, whereas four studies (9–11, 16) utilized both of these constructs. Those utilizing technology typically used a smartphone or PC-based application (4, 14–16, 23), while three studies used wearable technology designed to provide notification in the form of haptic feedback (alerting through vibration) (3, 9, 23) when subject had been sedentary for a prolonged, uninterupted time period (typically ≥30 minutes). Studies utilizing smartphone or PC-based technology differed by application, though all were designed to alert the participant in some fashion to prolonged time sedentary. Two studies made use of texting technology (15, 16), both in the form of daily text messages of support. Kendzor, et al. (15) tailored this message based on the amount of time sitting the previous day. One study employed the use of smartphone timers to alert participants that it was time for a break in sedentary time (16), while two others designed smartphone applications specific to their intervention (23, 4). Pellegrini et al (23) developed the NEAT! application which, when paired with the Shimmer accelerometer, delivered an audible or vibratory alert after 20 minutes of uninterrupted sedentary time. Bond et al (4) also developed an application (BMobile) that delivered activity prompts paired to the smartphone’s onboard accelerometer. One study using a PC application (14) provided hourly alerts to break-up their sitting time. This prompt encouraged participants to stand or walk for seven minutes every hour. If this prompt was ignored or postponed, after an additional five minutes, the computer screen would “lock” for seven minutes. Finally, one study (22) used a device that would electronically “lock out” the television after a certain amount of time spent watching. With regards to sedentary time, twelve of the studies employed an objective measure of sedentary time (see Table 1 for devices used) and one study used direct observation (17).
Feasibility & Acceptability of Intervention
Five of the thirteen studies specifically reported on the feasibility or acceptability of the intervention (Table 3) (4, 11, 16, 18, 23). One additional study referred to itself as a feasibility study (10), but did not describe findings regarding feasibility. In most studies, feasibility was typically measured objectively through enrollment, adherence, attendance, and retention, as well as through questionnaires or interviews regarding participant satisfaction, and/or acceptability. Due to the frequent use of enrollment, adherence, and retention rates as feasibility outcomes, we also included studies in the following results that provided information allowing us to calculate these rates, but did not specifically discuss them as “feasibility outcomes.” Enrollment varied greatly among studies, ranging from 29% enrollment of those initially contacted (23), through 97% of those contacted (18), with one study not providing this information (10). Conversely, reported retention rates were generally high among studies (86%–100%). In those studies that collected participant satisfaction/acceptability, all reported scores that suggest that participation in the intervention was viewed as “favorable to very favorable”, would use again, and that participant burden was quite low. Of those studies that specifically included and discussed feasibility data, all suggested that the interventions were feasible.
Table 3.
Major outcomes, feasibility, efficacy and effectiveness data for reducing sedentary time from non-worksite interventions to reduce sedentary time.
| Study | Primary Outcomes | Secondary Outcomes | Feasibility Data | Efficacy/Effectiveness Data for Reducing Sedentary Time |
|---|---|---|---|---|
| Otten (22) | Energy intake | Energy expenditure; total sleep; time spent in sedentary activities; time spent in PA | N/A | Sig. difference in daily sedentary time b/w intervention and control group (mean change (95% CI)): −3.8% (−6.3 to −1.3) vs. 1.1% (−3.2 to 5.4); p<.04) |
| Gardiner (11) | Program reach (participants enrolled/participants screened & eligible) and retention (% completed); total sedentary time/breaks in sedentary time, time spent in PA; participant satisfaction | N/A | Reach: 88%; retention: 100%; participant satisfaction: 97% rated 8 or higher/10 (median=9, range=7–10) | Sig. decrease in daily sedentary time pre- to post-intervention (3.2% (−4.18, −2.14); p<.01); Sig increase in breaks in sedentary time (4.0 (1.48, 6.52); p<.01) |
| Fitzsimonsp (10) | Objectively measured total sedentary time/breaks in sedentary time (pre- vs. post-intervention); subjective measures of sedentary time (incl. type) | N/A | Titled as feasibility study, but no feasibility outcomes discussed | Decrease in objectively measured sedentary time pre- to post-intervention (24 min/day; 2.2% daily reduction). No apparent diff in breaks in sedentary time pre- vs. post-intervention. Subjective data suggest participants under-reported changes in sedentary time. |
| Aadahl (1) | Objectively measured total sedentary time | Number of breaks in sedentary time; self-reported sitting time; weakly MVPA; anthropometrics; cardio biomarkers | *Enrollment a: 56%,* retention b: 90% | No sig. differences in objectively measured sitting time/standing breaks between groups; sig difference between groups re: self-reported leisure sitting/day (−0.81 (−1.4, −0.3) hrs/day); p<.01) |
| Bond (4) | Objectively measured total sedentary time | Time spent in PA; acceptability and preference of intervention | *Enrollment a:49% ; *retentionb :86% ; acceptability: 90% of subjects “agreed” or “strongly agreed” that intervention 1) significantly increased motivation to take PA breaks and 2) significantly decreased time sedentary due to intervention | Percent of waking hours spent sedentary was sig. decreased in all 3 conditions (3–6% decrease; p<.01); pairwise comparisons showed sig greater reductions in percent sedentary for the 3 min break in sedentary time after 30 continuous min sedentary vs. 12 min break after 120 min sedentary |
| Biddle (3) | Objectively measured total sedentary time | Self-report sedentary time; objectively and subjectively measured PA; biochemical, anthropometric, psycho-social & variables | *Enrollment a: 96%,* retention b: 71% | No sig differences in sedentary time (0.73% decrease in daily sed time; p>.05) |
| Judicep (14) | Objectively measured total sedentary time | Changes in stepping, standing, breaks in sedentary time (sit/stand transitions) and participant satisfaction | *Enrollment a: 33%;* retention b: 100%; intervention satisfaction: 60% of participants rated intervention extremely satisfying (score of 10 on a 1–10 scale; median: 9.5, min–max: 8–10). Seven of ten participants reported leisure-time to be the greatest domain to perform sedentary time changes | Participants in the intervention group had less daily sitting time (1.85 hrs (0.6–2.75)), more standing (0.77 hrs (0.06–1.48)), and more stepping (1.09 hrs (0.79–1.38)). No apparent changes in sit-to-stand transitions |
| Lang (17) | Number of conference attendees standing during presentations at an academic conference | N/A | N/A | Larger proportion of individuals in the intervention group (point-of decision prompting) stood during presentations than those in the control group (17% ±2% vs. 11% ±2%) |
| Pellegrinip (23) | Smartphone app usage & acceptability; anthropometric data; objectively measured total sedentary time | N/A | *Enrollment a: 29%;* retention b: 89%; acceptability: all participants agreed or strongly agreed that the app made them more aware of their sedentary time. 88% would use again. 88% helped to remember to break sedentary time. 50% stated the app was easy to use | Sedentary time decreased 8.1% (±4.5%) between baseline and one month [addition of outlier (n=1) attenuated the effect] |
| Ellingsonp (9) | Objectively measured total sedentary time | Changes in objectively measured PA and mood; participant perception of sedentary behavior | N/A | No differences in total minutes of time spent sedentary; participants receiving intervention decreased sitting time in prolonged bouts (≥30 min) and increased time spent in shorter bouts (<30 min). Perception: 27/28 participants were more aware of, and agreed with the importance of limiting, sedentary behavior post-intervention. 26/28 planned to limit sedentary time after completion of the study |
| Kendzor (15) | Objectively measured total sedentary time & PA | N/A | N/A | Significantly fewer minutes of sedentary time/day (B=−22.1; p<.05) |
| Kerrp (16) | Objectively measured total sedentary time, daily stepping time, number of sit-to-stand transitions | Feasibility and acceptability of intervention | Qualitative interviews suggested that the intervention was “acceptable and feasible,” as participants found wearing the device to be comfortable, the information presented to them to be helpful and understandable, as well as satisfied with the modes of intervention delivery and content. *Enrollment a (number eligible/number enrolled): 59%;* retentionb : 100% | Participants randomized to sitting time reduction group had a decrease (130 min/day) in daily sitting time, but no differences in sit-to-stand transitions; those randomized to increase in sit-to-stand transitions increased the number of transitions (13/day), but no change in total sitting time |
| Lewis (18) | Objectively measured total sedentary time and bouts of prolonged sitting (≥30 min); time spent watching TV; time spent in PA; participant satisfaction & burden; program uptake a & retentionb | N/A | Program uptake: 97%; program retention: 90%; participant satisfaction: overall program satisfaction was high (8.2±1.8 out of 10) and 8.2 ±2.2 would likely recommend the program; participant burden was rated as low (8.8±1.2 out of 10, with 10 representing ‘not time consuming at all). 96% of participants reported easy to wear | Participants significantly reduced their total daily sitting time (−51.5 min; p=.01), sitting time accrued in prolonged bouts (−53.9; p<.01), number of bouts of prolonged sitting (−0.8; p<.01), and % waking hours spent sitting (−5.3%; p=.01) |
=designated as pilot study.
=Feasibility data not officially presented, but can be calculated from information presented in the study.
=percent of participants eligible who were enrolled in study.
=Percent of participants enrolled in study who completed post-intervention assessment.
Efficacy/Effectiveness of Intervention
Data regarding the efficacy or effectiveness of the intervention to reduce time spent sedentary are presented in Table 3. Ten of the thirteen studies indicated a significant reduction in objectively measured sitting time post-intervention (4, 10, 11, 14–18, 22, 23) though in one study (23), this finding was attenuated when including outliers. With regards to significance, it should be noted that only five studies were appropriately powered (4, 11, 15, 18, 22), having included an a priori effect size estimate which they used to determine their sample size. In the seven studies to evaluate breaks in prolonged sitting time (≥30 min) or sit-to-stand transitions, four observed significantly favorable outcomes post-intervention (9, 11, 16, 18). The included interventions reported reductions in total daily sedentary time of a range between 0.7% (3) and 8.1% (22) or between 22 (15) and 130 (16) min/day (pre to post or compared to control, depending on design).
Discussion
This review is the first to focus specifically on non-worksite interventions to limit sedentary behavior in adults. We identified thirteen studies whose primary or secondary outcome was to reduce overall sitting time and/or increase the number of breaks in prolonged sitting time. Generally, regardless of the intervention characteristics, sedentary behavior interventions appear to be efficacious, as most reported significant findings for at least one sitting time-related outcome. While these results varied with respect to the reported decrease in time spent sedentary or increase in breaks, the results are encouraging. Additionally, studies that reported feasibility data suggest that these interventions are largely acceptable, easy to use and implement, satisfactory to participants, and able to enroll and retain participants.
While the efficacy results discussed here are generally favorable, it is important to note that these non-workplace sedentary behavior interventions vary widely with respect to study design, population, intervention duration, mode of delivery, and outcome measurement. Combined with the relatively small number of currently published studies, this variability limits the ability to draw strong conclusions regarding the most appropriate or efficacious approaches to modify sedentary time. However, as these studies collectively showed promising results for reducing sedentary time, there were some intervention characteristics that were shared among studies. First, it should be noted that seven of the thirteen studies reviewed utilized a randomized design. Of those, nearly all studies were of high methodological quality as determined by the Delphi criteria, with five of those seven reporting favorable significant findings. Further, with respect to the intervention components, interventions typically fell into one of three categories: use of technology to reduce sedentary time, use of specific behavior change techniques to limit sitting time, or a combination of the two. Interestingly, findings did not differ greatly by these intervention components among studies.
The interventions specifically based on a behavioral theory utilized various behavior models in their design, such that one particular behavioral theory could not be highlighted as more or less efficacious at limiting sedentary time than the others While the technological devices also varied among studies, they were designed to assist in alerting the user to accumulated sedentary behavior in the form of haptic feedback. This is an important finding, in that as the use of haptic feedback as a cue to action could be considered a form of self-monitoring, this approach to lifestyle behavior change has a strong theoretical foundation (5). Further, it is likely that the studies utilizing these approaches that did not explicitly state that their intervention was theory-based may have, in actuality, utilized these methods. Collectively, this suggests that coupling behavior change theory, specifically the use of a cue to action alert as a surrogate for self-monitoring, with a technological application may be a successful avenue to reduce non-work related sedentary time.
While the studies reviewed here have generally been considered to be of good methodological quality, the many differences among the studies made interpretation of these data difficult. Almost half of the studies used a pre-post experimental design (4, 10, 11, 15, 18, 23), which makes evaluating these studies in conjunction with RCTs a challenge. Further, sample sizes ranged greatly among studies, with eight of the thirteen studies self-titled as, or having small enough sample sizes (n<37) to be considered, pilot studies (Table 1). Of those, two studies reported findings on ten subjects or fewer (14, 23). To get a true idea of which intervention designs have the greatest potential, more work is warranted with appropriately powered samples. Additionally, the samples within these studies varied in age range and health status. While findings across studies are encouraging in that they suggest these interventions might be appropriate across varying populations, it adds to the challenge of highlighting the most appropriate intervention approach to limit sedentary behavior.
The duration of the intervention also widely differed among studies. One study conducted a single 1-hour session (17), four studies reported an intervention of only one week (11, 14, 15, 18), while others reported interventions as long as twelve months (3). While new literature suggests that there is considerable variation in the amount of time necessary to change behavior, successful habit formation likely occurs on the scale of weeks to months rather than days (12). Further, only one study (9) reported follow-up time points to attempt to measure if the potential change in behavior was maintained over time. While findings presented by the studies of shorter duration are comparable to those of longer duration, the varying degree of time spent in these interventions, the lack of follow-up data in the majority of studies, along with the differences in approach and mode of delivery, suggest that more work is needed to further identify the most promising duration of a sedentary behavior intervention.
There were also limitations in the analysis of the included studies. The majority of studies assembled here utilized objective measures of sedentary behavior, which are favorable to the often under-estimated self-report of sedentary time (2). However, the tools used in collecting these data (ActiGraph, ActivPAL, Sensewear Arm bands) differed among studies. Future reviews comparing data collected from the same measure will help generate a greater consensus with respect to best practices of sedentary interventions. Also of note, few studies utilized an intent-to-treat analysis (n=4), which could lead to a potentially biased estimate of the treatment effect. Future studies should be mindful with regards to analysis strategies to shed light on true efficacy practices.
Finally, it is important to note that this review is not without limitations. As stated previously, due to the diversity of the study designs, participants, and intervention techniques, we were unable to conduct a meta-analysis, which would have furthered our understanding regarding the magnitude of the effect of these interventions, Specifically, as there were few interventions dedicated to focusing on specifically lessening sedentary time versus increasing physical activity while also not focusing on sedentary reductions in the workplace, we chose to include all studies meeting our robust criteria in which to get a full snapshot of these practices. Unfortunately, the various study designs, having included both randomized control trials and non-randomized trials, as well as pilot studies and fully powered studies, hinder our ability to quantify and describe the efficacy and effectiveness across trials. It should also be noted that constraining our eligibility criteria to include only those articles that were published in English could have excluded relevant unpublished data or studies published in other languages. Due to these limitations, while our findings were encouraging, more work is necessary to further describe these outcomes.
Future Directions
While preliminary findings that non-worksite sedentary interventions appear to be both feasible and efficacious in the short-term are encouraging, much work remains to further our understanding of this topic. Larger, appropriately-powered trials are needed to test these interventions and give us a better idea as to how efficacious and effective these interventions might be. Further, longer duration interventions, as well as a period of follow-up, are strongly needed in order to examine true behavior change. It is imperative that we evaluate the long-term success of these interventions to discover if individuals adopt and maintain these behaviors or if they revert back to previous sedentary patterns post-intervention.
Not only do we require further work to provide necessary information regarding the efficacy of these interventions, but also studies to provide evidence on the appropriate “dose” of sedentary reduction or number of breaks (and timing of these breaks) to optimize health benefits. While observational, prospective trials continue to support a dose-response relationship between sedentary behavior and health, using these data to inform future interventions such that recommended doses of sedentary reduction are both optimized and comparable across studies is warranted.
More work is needed to assess the appropriate intervention strategies for particular populations. The populations investigated in this review varied from young to older adults and included both healthy and populations with defined comorbidities, including those identified as overweight, obese, and/or those who had diabetes. It is possible that different interventions will be more effective in specific populations depending on how and when they incorporate techniques to lessen sedentary time. For example, younger adults may be more amenable to a sitting time prescription in which total duration of sitting is reduced whereas older adults could experience greater success with an intervention that focused on increasing the frequency of standing breaks. Further, younger adults may be more amenable to technology-based interventions than their older counterparts. The ability to tailor intervention prescriptions to specific populations is likely to increase the effectiveness of the interventions.
As these interventions appear to be efficacious and favorable, there is a need for effectiveness studies that delineate their effects on objective markers of health. Mounting evidence suggests that there is increased cardio-metabolic risk associated with time spent sedentary. Physiological biomarkers can give us great insight into the mechanism by which limiting sedentary behavior is beneficial to health, especially in those with chronic disease, such as Type II diabetes or cancer. Greater understanding of the physiologic link between sedentary time and these health outcomes can help to shape future interventions.
Conclusions
In this first systematic review of interventions specifically designed to decrease sedentary time that are not limited to the workplace, our findings suggest that interventions to reduce sedentary time and/or increase breaks in long, interrupted periods of sedentary time show promise. As a whole, these interventions are feasible, acceptable, and generally efficacious, at least in the short term. However, due to the small body of evidence and the disparate nature of these works, our ability to make overarching statements regarding “best practices” at this time is not supported. Well-controlled trials of longer duration with larger samples, using theoretically-based interventions with consistent goals or prescriptions for limiting sedentary time and similar methods of measuring sedentary behavior are strongly warranted.
Supplementary Material
Acknowledgments
This research was supported by 1K07CA178870. The results of this study do not constitute the endorsement of the ACSM.
Footnotes
SDC1.docx—Appendix, Search Criteria
References
- 1.Aadahl M, Linneberg A, Moller TC, et al. Motivational counseling to reduce sitting time: A community-based randomized controlled trial in adults. Am J Prev Med. 2014;47(5):576–86. doi: 10.1016/j.amepre.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 2.Atkin AJ, Gorely T, Clemes SA, et al. Methods of measurement in epidemiology: Sedentary behaviour. Int J Epidemiol. 2012;41(5):1460–71. doi: 10.1093/ije/dys118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biddle SJ, Edwardson CL, Wilmot EG, et al. A randomised controlled trial to reduce sedentary time in young adults at risk of type 2 diabetes mellitus: Project STAND (sedentary time and diabetes) PLoS One. 2015;10(12):e0143398. doi: 10.1371/journal.pone.0143398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bond DS, Thomas JG, Raynor HA, et al. B-MOBILE--a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: A within-subjects experimental trial. PLoS One. 2014;9(6):e100821. doi: 10.1371/journal.pone.0100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of the literature. J Am Diet Assoc. 2011;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cart LRSM. Letter to the editor: Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 7.Chau JY, der Ploeg HP, van Uffelen JG, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med. 2010;51(5):352–6. doi: 10.1016/j.ypmed.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting--a health hazard. Diabetes Res Clin Pract. 2012;97(3):368–76. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 9.Ellingson LD, Meyer Jacob D, Cook Dane B. Wearable technology reduces prolonged bouts of sedentary behavior. Translational Journal of the American College of Sports Medicine. 2016;1(2):10–7. [Google Scholar]
- 10.Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, Mutrie N. Using an individualised consultation and activPAL feedback to reduce sedentary time in older Scottish adults: results of a feasibility and pilot study. Prev Med. 2013;57(5):718–20. doi: 10.1016/j.ypmed.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 11.Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults’ sedentary time. American Journal of Preventive Medicine. 2011;41(2):174–7. doi: 10.1016/j.amepre.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Gardner B, Lally P, Wardle J. Making health habitual: the psychology of ‘habit-formation’ and general practice. Br J Gen Pract. 2012;62(605):664–6. doi: 10.3399/bjgp12X659466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJ. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psycol Rev. 2015;10(1):89–112. doi: 10.1080/17437199.2015.1082146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Judice PB, Hamilton MT, Sardinha LB, Silva AM. Randomized controlled pilot of an intervention to reduce and break-up overweight/obese adults’ overall sitting-time. Trials. 2015;16:490. doi: 10.1186/s13063-015-1015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kendzor DE, Shuval K, Gabriel KP, et al. Impact of a mobile phone intervention to reduce sedentary behavior in a community sample of adults: A quasi-experimental evaluation. J Med Internet Res. 2016;18(1):e19. doi: 10.2196/jmir.5137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr J, Takemoto M, Bolling K, et al. Two-arm randomized pilot intervention trial to decrease sitting time and increase sit-to-stand transitions in working and non-working older adults. PLoS One. 2016;11(1):e0145427. doi: 10.1371/journal.pone.0145427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lang JJ, McNeil J, Tremblay MS, Saunders TJ. Sit less, stand more: A randomized point-of-decision prompt intervention to reduce sedentary time. Prev Med. 2015;73:67–9. doi: 10.1016/j.ypmed.2015.01.026. [DOI] [PubMed] [Google Scholar]
- 18.Lewis LK, Rowlands AV, Gardiner PA, Standage M, English C, Olds T. Small Steps: Preliminary effectiveness and feasibility of an incremental goal-setting intervention to reduce sitting time in older adults. Maturitas. 2016;85:64–70. doi: 10.1016/j.maturitas.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Martin A, Fitzsimons C, Jepson R, et al. Interventions with potential to reduce sedentary time in adults: Systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1056–63. doi: 10.1136/bjsports-2014-094524. [DOI] [PubMed] [Google Scholar]
- 20.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology. 2008;167(7):875–81. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Otten JJ, Jones KE, Littenberg B, Harvey-Berino J. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: A randomized controlled trial. Archives of Internal Medicine. 2009;169(22):2109. doi: 10.1001/archinternmed.2009.430. [DOI] [PubMed] [Google Scholar]
- 23.Pellegrini CA, Hoffman SA, Daly ER, Murillo M, Iakovlev G, Spring B. Acceptability of smartphone technology to interrupt sedentary time in adults with diabetes. Transl Behav Med. 2015;5(3):307–14. doi: 10.1007/s13142-015-0314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Physical Activity Guidelines Advisory C. Physical activity guidelines advisory committee report, 2008. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 25.Prince SA, Saunders TJ, Gretsy K, et al. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: A systematic review and meta-analysis of controlled trials. Obesity Reviews. 2014;15(11):905–19. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Bhaumik S. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. 2016;3:Cd010912. doi: 10.1002/14651858.CD010912.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: A review. Int J Behav Med. 2010;17(4):246–54. doi: 10.1007/s12529-010-9075-z. [DOI] [PubMed] [Google Scholar]
- 28.Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: A systematic review. BMC Public Health. 2015;15:513. doi: 10.1186/s12889-015-1843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: A systematic review of longitudinal studies, 1996–2011. American Journal of Preventive Medicine. 2011;41(2):207–15. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 30.Verhagen AP, de Vet HC, de Bie RA, et al. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–41. doi: 10.1016/s0895-4356(98)00131-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.