Abstract
The aim of the present study was to evaluate the association between failed smoking cessation and occupation by age stratification among Korean males and provide quantitative evidence of factors associated with failed smoking cessation. The study comprised 3,127 male workers who had attempted smoking cessation during their life time. Data were obtained from the Korea National Health and Nutrition Examination Survey from 2010 to 2012. Participants were stratified by age into two subgroups comprising a younger group (19–40 yr) and an older group (41–60 yr). Multiple logistic regression analyses were used to estimate odds ratios (ORs) for failed smoking cessation. In the younger group, failed smoking cessation was related to the occupational fields “service and sales” and “manual work” compared to “office work” (OR: 2.10, 95% confidence interval (CI): 1.34–3.29; and OR: 1.47, 95% CI: 1.02–2.12, respectively). In the older group, the ORs of failed smoking cessation occupational categories “service and sales” and “manual work” [ref: office workers] were 0.58 (0.40–0.85) and 0.90 (0.66–1.24), respectively. Failed smoking cessation is associated with occupational categories and age stratification. Policy makers need to create tailored anti-smoking policy considering the occupation and the age of the subjects.
Keywords: Smoking cessation, Smoking cessation failure, Service and sales, Occupation, Age
Introduction
Increased awareness of smoking cessation has resulted in many countries focusing on political strategies and increased budgets for cessation programs including community-wide educational approaches1, 2, 3). These measures are more cost-effective than health care services4). Cessation policies require information on smoking properties including factors contributing to cessation failure for an appropriate approach.
Individual factors such as education, socioeconomic status, age, and motivation to quit as important causes of failed smoking cessation were the focus of previous studies5, 6, 7). However, few studies have described the role of occupation on smoking cessation. Workplace culture, job stress, and specific work-related characteristics are important determinants of smoking persistence8, 9). Compared with white collar workers, blue collar workers, including construction workers, often fail in their attempts to quit smoking8). Furthermore, subsequent studies focusing on smoking cessation and occupation mainly categorized occupation as manual and non-manual for comparative purposes10, 11). Higher smoking rates are found in service and sales workers as this section of the workforce requires intensive emotional labor and differs considerably from office work or manual work12). As the structure of the Korean industry has changed from secondary (i.e., manufacturing) to tertiary (e.g., service and sales), identifying the characteristics of service and sales workers for effective smoking cessation is of importance.
Acknowledging the various numbers of failed smoking cessation attempts and factors related to different occupations (office workers, service and sales, manual workers) may assist both employers and politicians in improving the efficacy of present strategies. In the present study, various rates and factors related to failed smoking cessation among male workers in diverse occupational groups were reported using data from the Korean National Health and Nutrition Examination Survey (KNHANES).
Subjects and Methods
Source of data
KNHANES is an annual national survey representing a non-institutionalized, civilian population in South Korea. It was conducted by the Korean Ministry of Health and Welfare and performed by the Korean Center for Disease Control and Prevention (KCDC). KNHANES comprises three surveys: a health interview, health examination, and nutrition survey. Trained interviewers collected data from the participants concerning level of education, economic activity, morbidity, medical use, and nutrition. Health behaviors including smoking and alcohol were recorded via self-administered questionnaires. The present study was based on data collected during KNHANES V, which was performed from 2010 to 2012 and involved 25,534 participants (approximately an average 80% of the participation rate). Further details are available from the “Guidelines for use of KNHANES V (2010–2012)” and previous published studies13, 14).
Study participants
Among the participants (n=25,534) from KNHANES V, 13,918 females (54.1%), 5,809 males aged <19 yr or >60 yr, 1,214 non-smoking males (never smoked during their life time), 496 males with no previous attempt to quit smoking, missing (n=567), and 403 unemployed participants or military soldiers were excluded from the study. Following exclusion, 3,127 male workers aged between 19 and 60 yr who had previously attempted to quit smoking were included in the study.
Verification of smoking status
Current smokers were defined as individuals who smoked either daily or occasionally. Failed smoking cessation was defined as subjects who attempted to quit smoking at some stage in their life time but failed (n=1,689, 54.0%).
General characteristics, socioeconomic status, and occupational category
The study population was categorized according to age into younger (19–40 yr) and older groups (41–60 yr). The occupational schema based on the Korea national coding system was used for categorization of occupations following interviews in which each participant’s occupation was obtained in detail. The categorical variable job comprised nine items that were classified into three subcategories: “administrator”, “professionals”, and “clerks” as “office work”; “service worker” and “salesperson” as “service and sales”; and “agricultural, forestry, and fishery workers”, “technicians”, “machinery operators”, and “laborers” as “manual work”.
Other variables were defined as follows: working hours were defined as the average number of weekly working hours including overtime with mealtime exclusion; regular walking was derived from the question “How often do you walk at least 30 min including commute, transit and exercise?” and defined as at least 30 min of walking at least five times a week. The question was required to be answer as accumulation minutes of a day; and alcohol intake was defined using the Alcohol Use Disorder Identification Test (AUDIT)15); An AUDIT score less than 8 was defined as “normal intake”, an AUDIT score between 8 and 15 as “heavy intake”, an AUDIT score between 16 and 19 as “very heavy intake”, and an AUDIT score ≥20 as “alcohol dependent”. Marital status was categorized as “married or cohabitating” or “separated or not married”. Perceived stress status was defined using the question “how much stress does the individual feel on a daily basis?” in the self-reported questionnaire using the Likert point scale, with the responses “very much” and “much” regarded as “much”, and “a little” and “little” regarded as “less”.
Socioeconomic positions were defined as follows: level of education was defined as highest level of education (“middle school or less”, “high school”, “university or more”); and household income was defined as family income in the “first, second, third, and fourth quartile”.
Statistical analyses
This study was a cross-sectional study. A pooled survey weight for the datasets from 2010, 2011, and 2012 was applied to function as the representative of the entire Korean population, followed by aggregation of the data. The variables including age, education, household income level, exercise, alcohol consumption, working hours, marital status, stress, and occupational category were evaluated. Data were analyzed using the Student’s t-test, Rao-Scott χ2 test, and survey logistic regression. Multiple logistic regression analysis was performed to estimate the odds ratios (ORs) for failed smoking cessation among Korean male workers. Statistical analyses were performed using SAS version 9.4 (Statistical Analysis System Institute, Cary, NC, USA). A p-value less than 0.05 was considered statistically significant.
Results
Demographic and occupational characteristics of the subjects with age stratification are depicted in Table 1. Both the younger and older groups showed significant differences for all variables with the exception of working hours. The number of manual workers among the eligible population was observed to increase in the older cessation attempt group.
Table 1. Demographic and occupational characteristics of the study participants based on age stratification.
| 19–40 yr | 41–60 yr | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | aweighted N | % (SE) | N | aweighted N | % (SE) | p-value | |||
| Age (yr, mean (SD)) | 33.7 (5.7) | 50.2 (5.7) | <0.001 | ||||||
| Occupational category | <0.001 | ||||||||
| office work | 626 | 1,790,405 | 43.8 (1.6) | 682 | 1,581,151 | 33.1 (1.3) | |||
| service and sales | 247 | 835,462 | 20.4 (1.5) | 271 | 753,249 | 15.8 (1.0) | |||
| manual work | 408 | 1,460,664 | 35.6 (1.6) | 893 | 2,438,088 | 51.1 (1.5) | |||
| Working hours (per 1 wk, mean (SD)) | 49.3 (14.2) | 48.7 (16.4) | 0.241 | ||||||
| Educational level | <0.001 | ||||||||
| middle school or less | 34 | 138,542 | 3.4 (0.6) | 454 | 1,184,364 | 24.8 (1.3) | |||
| high school | 487 | 1,767,530 | 43.3 (1.6) | 741 | 1,978,741 | 41.5 (1.4) | |||
| university or more | 760 | 2,180,459 | 53.3 (1.6) | 678 | 1,609,383 | 33.7 (1.5) | |||
| Household income status | 0.001 | ||||||||
| low | 67 | 251,915 | 6.2 (0.8) | 107 | 278,342 | 5.8 (0.6) | |||
| low medium | 348 | 1,101,819 | 27.0 (1.5) | 395 | 1,182,646 | 24.7 (1.3) | |||
| medium high | 480 | 1,519,025 | 37.1 (1.5) | 584 | 1,516,705 | 31.8 (1.2) | |||
| high | 386 | 1,213,772 | 29.7 (1.6) | 760 | 1,794,795 | 37.6 (1.5) | |||
| Regular walking | <0.001 | ||||||||
| less than 30 min or 5 d/wk | 759 | 2,256,644 | 55.2 (1.7) | 1,201 | 3,056,495 | 64.0 (1.4) | |||
| more than 30 min*5 d/wk | 522 | 1,829,887 | 44.8 (1.7) | 645 | 1,715,992 | 36.0 (1.4) | |||
| Alcohol intake | 0.001 | ||||||||
| normal | 439 | 1,370,339 | 34.1 (1.6) | 704 | 1,726,520 | 37.5 (1.4) | |||
| heavy | 512 | 1,665,024 | 41.4 (1.7) | 578 | 1,509,069 | 32.8 (1.3) | |||
| very heavy | 167 | 517,870 | 12.9 (1.1) | 250 | 662,531 | 14.4 (1.0) | |||
| alcohol dependent | 145 | 467,949 | 11.6 (1.1) | 249 | 699,900 | 15.2 (1.1) | |||
| Marital status | <0.001 | ||||||||
| married or cohabitating | 869 | 2,388,426 | 58.4 (1.8) | 1,736 | 4,395,870 | 92.1 (0.9) | |||
| separated or not married | 412 | 1,698,105 | 41.5 (1.8) | 110 | 376,618 | 7.9 (0.9) | |||
| Perceived stress | <0.001 | ||||||||
| less | 846 | 2,803,245 | 68.6 (1.5) | 1,368 | 3,579,025 | 74.9 (1.1) | |||
| much | 435 | 1,283,286 | 31.4 (1.5) | 478 | 1,193,463 | 25.1 (1.1) | |||
| Total | 1,281 | 4,086,531 | 100 | 1,846 | 4,772,488 | 100 | |||
All study participants were male.
SD: standard deviation; SE: standard error; yr: year; and hr: hour
a weighted N: weighted number in Korean National Health and Nutrition Examination Survey is representative of the Korean civilian noninstitutionalized census population
Demographic and occupational characteristics for specific occupation groups in regard to age are shown in Table 2. Mean age, daily working hours, level of education, household income, and marital status significantly differed (p<0.05) according to occupation between the younger and older groups. Although the variable perceived stress was significantly different among the job categories in the older group, it was not observed to be significant in the younger group (Table 2).
Table 2. Demographic and occupational characteristics of the study participants according to occupational category.
| 19–40 yr | 41–60 yr | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Occupational category | Occupational category | |||||||||||||||||||
| Office work | Service and sales | Manual work | p-value | Office work | Service and sales | Manual work | p-value | |||||||||||||
| aweighted N % (SE) | aweighted N % (SE) | aweighted N % (SE) | aweighted N % (SE) | aweighted N % (SE) | aweighted N % (SE) | |||||||||||||||
| Age (year, mean (SD)) | 33.1 (0.2) | 30.6 (0.7) | 32.6 (0.4) | <0.001 | 48.2 (0.3) | 49.7 (0.5) | 50.3 (0.2) | <0.001 | ||||||||||||
| Working hours (per 1 wk, mean (SD)) | 46.8 (0.8) | 50.1 (1.5) | 50.6 (1.0) | 0.004 | 45.7 (0.6) | 54.3 (1.5) | 50.8 (0.9) | <0.001 | ||||||||||||
| Education | <0.0001 | <0.001 | ||||||||||||||||||
| middle school or less | 9,383 | 0.5 (0.4) | 25,522 | 3.1 (1.2) | 103,637 | 7.1 (1.5) | 51,306 | 3.2 (0.9) | 156,747 | 20.8 (3.0) | 976,312 | 40.0 (1.8) | ||||||||
| high school | 306,550 | 17.1 (1.8) | 471,929 | 56.5 (3.4) | 989,051 | 67.7 (2.5) | 485,046 | 30.7 (2.4) | 340,642 | 45.2 (3.6) | 1,153,053 | 47.3 (1.8) | ||||||||
| university or more | 1,474,472 | 82.4 (1.8) | 338,011 | 40.4 (3.3) | 367,976 | 25.2 (2.7) | 1,044,799 | 66.0 (2.4) | 255,860 | 34.0 (3.2) | 308,723 | 12.7 (1.2) | ||||||||
| Household income | <0.001 | <0.001 | ||||||||||||||||||
| low | 80,008 | 4.5 (1.1) | 51,909 | 6.2 (1.8) | 119,998 | 8.2 (1.6) | 48,306 | 3.1 (0.8) | 23,025 | 3.1 (1.3) | 207,011 | 8.5 (1.0) | ||||||||
| low medium | 352,410 | 19.7 (1.9) | 263,734 | 31.6 (3.2) | 485,674 | 33.3 (2.6) | 211,341 | 13.4 (1.7) | 172,785 | 23.0 (3.2) | 798,521 | 32.8 (2.0) | ||||||||
| medium high | 723,294 | 40.4 (2.1) | 269,399 | 32.2 (3.3) | 526,332 | 36.0 (2.6) | 491,893 | 31.1 (2.1) | 217,729 | 28.9 (3.1) | 807,083 | 33.1 (1.8) | ||||||||
| high | 634,693 | 35.4 (2.2) | 250,420 | 30.0 (3.1) | 328,659 | 22.5 (2.6) | 829,611 | 52.5 (2.3) | 339,710 | 45.1 (3.5) | 625,474 | 25.7 (1.9) | ||||||||
| Regular walking | 0.533 | 0.086 | ||||||||||||||||||
| less than 30 min or 5 d/wk | 969,437 | 54.1 (2.5) | 492,187 | 58.9 (3.7) | 795,020 | 54.4 (2.8) | 1,063,594 | 67.3 (2.1) | 503,457 | 66.8 (3.5) | 1,489,445 | 61.1 (2.0) | ||||||||
| more than 30 min*5 d/wk | 820,968 | 45.9 (2.5) | 343,275 | 41.1 (3.7) | 665,644 | 45.6 (2.8) | 517,557 | 32.7 (2.1) | 249,792 | 33.2 (3.5) | 948,643 | 38.9 (2.0) | ||||||||
| Alcohol intake | 0.063 | 0.138 | ||||||||||||||||||
| normal | 675,976 | 38.1 (2.3) | 223,731 | 27.4 (3.2) | 470,632 | 32.9 (2.7) | 596,375 | 38.4 (2.2) | 228,445 | 31.8 (3.3) | 901,700 | 38.8 (1.9) | ||||||||
| heavy | 712,055 | 40.1 (2.3) | 370,249 | 45.3 (4.3) | 582,720 | 40.7 (2.9) | 559,198 | 36.0 (2.1) | 230,867 | 32.1 (3.6) | 719,004 | 31.0 (1.8) | ||||||||
| very heavy | 237,561 | 13.4 (1.6) | 101,828 | 12.5 (2.9) | 178,481 | 12.5 (2.0) | 190,260 | 12.3 (1.5) | 121,056 | 16.8 (2.6) | 351,214 | 15.1 (1.4) | ||||||||
| alcohol dependent | 147,985 | 8.3 (1.5) | 121,474 | 14.9 (2.6) | 198,489 | 13.9 (1.9) | 207,091 | 13.3 (1.5) | 1,389,078 | 19.3 (3.0) | 353,902 | 15.2 (1.7) | ||||||||
| Marital status | 0.001 | 0.003 | ||||||||||||||||||
| married or cohabitating | 1,149,254 | 64.2 (2.4) | 407,081 | 48.7 (3.8) | 832,092 | 57.0 (2.9) | 1,510,046 | 95.5 (1.1) | 704,042 | 93.5 (2.0) | 2,181,782 | 89.5 (1.3) | ||||||||
| separated or not married | 641,152 | 35.8 (2.4) | 428,381 | 51.3 (3.8) | 628,572 | 43.0 (2.9) | 71,105 | 4.5 (1.1) | 49,207 | 6.5 (2.0) | 256,306 | 10.5 (1.3) | ||||||||
| Perceived stress | 0.159 | <0.001 | ||||||||||||||||||
| less | 1,178,809 | 65.8 (2.2) | 571,846 | 68.4 (3.2) | 1,052,590 | 72.1 (2.4) | 1,043,231 | 66.0 (2.2) | 586,149 | 77.8 (2.8) | 1,949,645 | 80.0 (1.5) | ||||||||
| much | 611,596 | 34.1 (2.2) | 263,616 | 31.6 (3.2) | 408,074 | 27.9 (2.4) | 537,920 | 34.0 (2.2) | 167,100 | 22.2 (2.8) | 488,443 | 20.0 (1.5) | ||||||||
| Total | 1,790,405 | 100 | 835,462 | 100 | 1,460,664 | 100 | 1,581,151 | 100 | 753,249 | 100 | 2,438,088 | 100 | ||||||||
All study participants were male.
SD: standard deviation; SE: standard error; wk: week; and hr: hour.
aweighted N: weighted number in Korean National Health and Nutrition Examination Survey is representative of Korean civilian noninstitutionalized census population
The ORs prior to adjustment for the variables are demonstrated in Table 3 and adjusted ORs in Table 4. Among participants in the younger group, the adjusted OR for failed smoking cessation in “service and sales workers” was 2.10 (95% confidence interval (CI) 1.34–3.29) and in “manual workers” [ref: office workers] was 1.47 (1.02–2.12). The adjusted OR for failed smoking cessation among “service and sales workers” was observed to be significantly low in the older group (0.58, 95% CI 0.40–0.85). The adjusted ORs for “working hours”, “level of education”, “regular walking”, and “marital status” were not significant among the failed smoking cessation workers in both the younger and older groups. The adjusted ORs for “heavy”, “very heavy”, and “alcohol dependent” alcohol intake significantly differed in both age groups (p<0.05 each). The variable perceived stress was significant in the older group.
Table 3. Unadjusted association between demographic and occupational characteristics and failed smoking cessation.
| 19–40 yr | 41–60 yr | |||||
|---|---|---|---|---|---|---|
| Unadjusted | Unadjusted | |||||
| OR | 95% CI | OR | 95% CI | |||
| Occupational category | ||||||
| office work | 1.00 | (—) | 1.00 | (—) | ||
| service and sales | 2.34 | (1.54–3.56) | 0.63 | (0.45–0.88) | ||
| manual work | 1.56 | (1.15–2.10) | 1.01 | (0.79–1.29) | ||
| Working hours (per 1 wk) | 1.00 | (0.99–1.01) | 1.00 | (0.99–1.01) | ||
| Age | 0.97 | (0.94–0.99) | 0.96 | (0.94–0.98) | ||
| Education | ||||||
| university or more | 1.00 | (—) | 1.00 | (—) | ||
| high school | 1.23 | (0.94–1.61) | 1.06 | (0.80–1.39) | ||
| middle school or less | 3.80 | (1.31–11.02) | 1.25 | (0.96–1.62) | ||
| Household income | ||||||
| high | 1.00 | (—) | 1.00 | (—) | ||
| medium high | 0.96 | (0.70–1.32) | 1.17 | (0.91–2.31) | ||
| low medium | 1.61 | (1.10–2.35) | 1.49 | (1.08–2.06) | ||
| low | 1.74 | (0.86–3.52) | 1.45 | (0.91–1.52) | ||
| Regular walking | ||||||
| less than 30 min or 5 d/wk | 1.00 | (—) | 1.00 | (—) | ||
| more than 30 min*5 d/wk | 1.04 | (0.79–1.36) | 0.86 | (0.68–1.09) | ||
| Alcohol intake | ||||||
| normal | 1.00 | (—) | 1.00 | (—) | ||
| heavy | 1.55 | (1.12–2.13) | 1.70 | (1.30–2.21) | ||
| very heavy | 1.64 | (1.02–2.65) | 1.99 | (1.43–2.78) | ||
| alcohol dependent | 2.13 | (1.31–3.49) | 1.89 | (1.32–2.70) | ||
| Marital status | ||||||
| married or cohabitating | 1.00 | (—) | 1.00 | (—) | ||
| separated or not married | 1.48 | (1.11–1.97) | 1.56 | (0.99–2.47) | ||
| Perceived stress | ||||||
| less | 1.00 | (—) | 1.00 | (—) | ||
| much | 1.21 | (0.90–1.64) | 1.43 | (1.12–1.84) | ||
CI: confidence interval; OR: odds ratio.
Table 4. Multiple logistic regression analysis between demographic and occupational characteristics and failed smoking cessation.
| 19–40-yr-old men | 41–60-yr-old men | |||||
|---|---|---|---|---|---|---|
| adjusted aOR | 95% CI | adjusted aOR | 95% CI | |||
| Occupational category | ||||||
| office work | 1.00 | (—) | 1.00 | (—) | ||
| service and sales | 2.10 | (1.34–3.29) | 0.58 | (0.40–0.85) | ||
| manual work | 1.47 | (1.02–2.21) | 0.90 | (0.66–1.24) | ||
| Working hours (per 1 wk) | 1.00 | (0.99–1.01) | 1.00 | (0.99–1.01) | ||
| Age | 0.98 | (0.94–1.01) | 0.96 | (0.94–0.98) | ||
| Education | ||||||
| university or more | 1.00 | (—) | 1.00 | (—) | ||
| high school | 0.83 | (0.59–1.15) | 1.33 | (0.98–1.80) | ||
| middle school or less | 3.02 | (0.89–10.31) | 1.23 | (0.84–1.78) | ||
| Household income | ||||||
| high | 1.00 | (—) | 1.00 | (—) | ||
| medium high | 1.03 | (0.75–1.40) | 1.15 | (0.88–1.50) | ||
| low medium | 1.54 | (1.02–2.33) | 1.45 | (1.03–2.05) | ||
| low | 1.67 | (0.80–3.49) | 1.48 | (0.90–2.44) | ||
| Regular walking | ||||||
| less than 30 min or 5 d/wk | 1.00 | (—) | 1.00 | (—) | ||
| more than 30 min*5 d/wk | 0.95 | (0.71–1.27) | 0.85 | (0.66–1.09) | ||
| Alcohol intake | ||||||
| normal | 1.00 | (—) | 1.00 | (—) | ||
| heavy | 1.46 | (1.05–2.03) | 1.66 | (1.26–2.18) | ||
| very heavy | 1.65 | (1.00–2.70) | 2.09 | (1.48–2.95) | ||
| alcohol dependent | 1.80 | (1.08–3.00) | 1.82 | (1.28–2.60) | ||
| Marriage status | ||||||
| married or cohabitating | 1.00 | (—) | 1.00 | (—) | ||
| separated or not married | 1.26 | (0.87–1.81) | 1.29 | (0.81–2.07) | ||
| Perceived stress | ||||||
| less | 1.00 | (—) | 1.00 | (—) | ||
| much | 1.24 | (0.90–1.72) | 1.32 | (1.02–1.71) | ||
a Adjusted: Odds ratio and 95% confidence intervals estimated using multiple logistic regression adjusted for occupational category, working hours, age, level of education, household income, regular walking, alcohol intake, marital status, and perceived stress levels.
CI: confidence interval; OR: odds ratio.
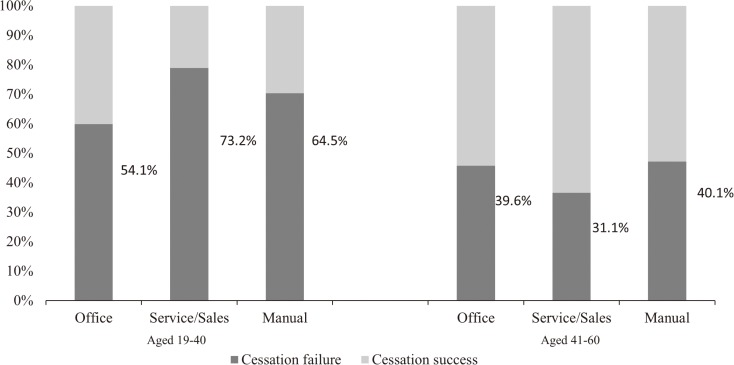
Based on the data from KNHANES V, the smoking cessation failure rate showed a difference in regard to age and job categories (Fig. 1). From the younger group 626 office workers, 247 service and sales workers, and 408 manual workers attempted to quit smoke. On the other hand, 682 office workers, 271 service and sales workers, and 893 manual workers attempted smoking cessation from the older group. Failed smoking cessation was higher in younger workers (range, 54.1–73.2%) than in older workers (range, 31.1–40.1%). In younger, the occupational field of “service and sales work” demonstrated the highest failure rates with significant differences between the various job categories. In older participants, attempts at cessation were more common and the failed cessation rate was generally low in the occupational category “service and sales work”, demonstrating the lowest failure rate among other occupational backgrounds (Fig. 1).
Fig. 1.
Age specific percentage of cessation failure workers by occupation categories, merged data from 2010–2012.
Discussion
From 2010 to 2012, failed smoking cessation among male workers varied in regard to occupational categories and age. While younger workers were found to be more likely to fail in their attempt to quit smoking in the occupations “service and sales” and “manual work”, older workers demonstrated a lower failure rate in the occupation category “service and sales”.
The current finding of different rates of successful cessation in association with occupation and age may be explained as a combinatory effect of working life per se and age. Older participants were more likely to succeed in smoking cessation than those in the younger group. This is consistent with data from the US National Health Interview Survey that was conducted from 2005 to 2012, in which cessation of smoking was found to be lowest among young adults aged 18–24 yr and highest among older adults aged ≥65 yr in each survey year16). This may be explained by the greater awareness of older adults of their health or as an inverse result of illness or developments of symptoms such as chronic obstructive pulmonary disease, cardiovascular disease, or aggregated dyspnea17). We observed a higher failure rate among older office workers that was found to differ to that from a previous study8). The aforementioned study did not focus on age, but primarily emphasized occupation or workplace policies as determinants of smoking, and demonstrated blue collar workers were at a higher risk of persistent smoking than white collar workers regardless of age. Age may have played a role in the discordance between the results in the previous8) and present study. Therefore, age stratification was applied to reduce the plausibility of underestimating the power of working life per se.
The present study demonstrates the different features of smoking cessation according to occupation via age. The higher failure rate of smoking cessation in specific occupational fields may be explained in a number of ways. First, service work usually requires emotional labor19) that results in the vulnerability of service workers to work-related stress20). Therefore, work-related stress derived from emotional service work may prevent service workers from ceasing smoking9). Second, some service workers, such as self-employed workers, have considerable unconstrained circumstances compared with office workers. These workers are able to control the length of their break, and therefore have increased opportunities to smoke. Third, young sales workers in Korea are more likely to be exposed to providing entertainment to customers and numerous business appointments that result in an increased likelihood to smoke and a failed cessation. Furthermore, sales workers tend to transit between many locations and have an increased opportunity to smoke during transit time despite attempting to cease smoking. Fifth, smoke-free programs are one of the most important advocates in the workplace, and their effectiveness has been proven over the past few decades8, 21, 22). However, fewer anti-smoking interventions are assumed to be available in the service and sales workplace compared with the office or manual workplace8).
Interestingly, older workers demonstrated an opposing characteristic, with a higher smoking cessation failure rate in office workers compared with service and sales workers and an almost identical risk in manual workers (Table 4). The reason that the older group in service and sales has a lower cessation failure rate not as in the younger group may be explained as follows. It is about the differences in working position thus different duty between the groups. The remaining older workers in service and sales field may be in stable position such as supervisors. They may have less emotional stress in reduction of providing entertainment for business purpose or of receiving customers directly. Thus, the minimized properties of service work among older workers would result in a lower OR. Table 2 shows the income is higher among older service and sales group participants than the younger group. When considering the income as one of the reflections of social status, older service and sales group participants are more likely to focus on their health as well as be in better social status compare to the younger group. Older office work group are also generally in stable position. The characteristics of older working groups’ position can be explained by psychosocial dimensions of the demand-control (Karasek) model18). The difference of cessation failure rate between older officer workers/manual workers and service and sales workers may rely on their demand intensity. Though the older office workers would usually have higher control compared to the younger office workers, large percentage of them would have a high demand at the same time as they are still employees attached to the firmed company system. On the otherhand, older sales and service workers may have less emotional stress in reduction of providing entertainment for business purpose or of receiving customers directly which can be explained as low strain job by the demand-control model. However, our paper has the limitation of combining workers from different occupational backgrounds into three representative occupations so the potential factors of failed cessation related to the specific work environment of each job may have been underestimated. Further studies classifying the occupation finely are required to know the difference of cessation failure factors in detail regard to the age and occupation. The results of this study indicate the importance of occupational categories and age in regard to smoking cessation.
We additionally analyzed the relationship between the smoking cessation failure and work hour by categorizing weekly work hour into “work hour ≤35”, “35<work hour ≤40”, “40<work hour” and had an interesting outcome. In both younger group and older group, we had found u shape pattern though it did not show the statistical significance. We had a modified u shape pattern in older group when we categorized weekly working hour more closely as “work hour ≤30” (OR 1.15, 95%Cl 0.74–1.77), “30<work hour ≤35” (1.99, 1.01–3.92) “35<work hour ≤40” (reference group), “40<work hour≤55” (1.11, 0.80–1.55), and “55<work hour” (1.28, 0.89–1.83). It showed similar pattern in younger group as well.
Socioeconomic status such as level of education and income is a well-established factor related to smoking cessation11, 23), that was found to be consistent in this KNHANES-based study. Financial stress is a factor that may explain the marked socioeconomic status differences in cessation rates24). Lack of self-efficacy may be another contributing factor that influences the cessation rate and is determined by a combination of low socioeconomic status and a number of other factors23).
Tobacco is associated with hazardous drinking habits or alcohol abuse25). In the present study, subjects who failed to quit smoking may be more likely to binge drink or vice versa. Our results also indicate perceived stress to be a barrier to smoking cessation in workers, although this was only found to be significant in the older group. As we were unable to identify whether the stress primarily originated from the participants’ work or personal life, detailed interpretation of the variable “perceived stress” was somewhat difficult. Further prospective studies should be performed to evaluate these relationships.
The present study has several limitations. First, as mentioned above, combining workers from different occupational backgrounds into three representative occupations may resulted in underestimation of each specific work environment feature. However, our aim of determining the features related to “service and sales” workers in terms of the cessation pattern was achieved in the present study. Another important limitation was that information concerning the period of smoking cessation attempts was unavailable. The participants’ occupation was a reflection of their current status that may lead to misclassification, as the participant may have attempted to cease smoking in their previous occupation. Despite the possibility of misclassification, we assumed that a change in the occupational category (office work/service and sales/manual work) was rather unlikely compared with a change in the occupation. Furthermore, the possibility of the gap between the time of attempt for smoking cessation and the variables is limitation of our study. Nevertheless, the average of starting smoking age were 18.6 (SD 2.7, younger group) and 19.5(SD 3.5, older group) while the average of smoking years of whom had succeeded quit smoking were 9.5 (SD 6.5, younger group) and 17.4 yr (SD 10.4, older group). And among the participants who were still smoking, 48.8 percent (SE 1.7) of the younger participants and 32% (SE 1.3) of the older participants tried smoking cessation during the past year. This information would minimize our limitation. Third, only male workers were considered, as female workers tend to conceal their smoking status due to cultural taboos that may pose difficulty when attempting to obtain reliable data, and, hence, in the identification of potential factors for failed cessation. This characteristic was observed by another study in Korea26). Despite validity provided by urine cotinine in the participants, we excluded women from analysis for reasons of accuracy. Fourth, In Korea, smoke-free policy has dramatically changed in recent years. The smoke-free zones have expanded recently. All the restaurants and bars became smoke-free from 2015 and within 10 m of every metro station became smoke-free zone since 2016. These smoke-free policies in the public place would have influenced the decision to stop smoking. The price of cigarettes may also have influenced the smoking as a pack of cigarette price in Korea was about 2,500 won (2.17 US $) before but increased to 4,500 won (3.91 US $) in 2015. Our study data was derived from 2010 to 2012 therefore does not reflect the recent change of smoking policy in Korea. With more recent data, we assume the overall cessation failure rate will drop down but still the difference according to the occupation and age would remain. Finally, a self-reported method was used for several variables. The details were difficult to access and may have resulted in a number of biases. However, as KNHANES V included bio-monitoring of urine cotinine (2,400 people annually from 2010 to 2011) for validation, the reliability of self-report contents was confirmed in terms of smoking patterns. Moreover, in a previous study, smoking-related data were shown to be highly reliable with a mean sensitivity of 87.5% and a mean specificity of 89.2%27).
Despite these limitations, our study has several strengths. First, the study demonstrated the importance of age stratification in conjunction with occupation. Occupational backgrounds with age stratification influence the smoking cessation failure rate, implying the importance of strategic approaches to occupational features on intervention programs. Second, the participants in the present study formed a large representation of the non-institutionalized adult Korean civilian population. Third, the present study investigated failed cessation attempts in an economically active male population, a target population for providing a workplace health promotion program.
In summary, the present study provides evidence that failed smoking cessation is strongly associated with occupational categories and age stratification. Quantitative evidence of major factors related to failed cessation is provided to support policy makers and community clinicians in the establishment of influential interventions aimed at reducing smoking in the workplace. Younger service and sales workers were found to be a vulnerable group to quit smoking so to access firstly with specific care. Providing stress management programs would be worthwhile. Also, the smoking cessation program for older office workers needs to be supported considering their age and their task characteristics. Further studies comprising focus group evaluations are required.
Acknowledgements
Contributors Youn-Mo Cho and Jun-Pyo Myong greatly contributed to the study concept and design, acquisition of data, analysis and interpretation of data, and drafting/revising the manuscript for important intellectual content, and approved the final version. Hyoung-Ryoul Kim, HyeEun Lee, and Jung-Wan Koo were involved in data analysis and interpretation and revised the manuscript.
Funding
This work was not supported by any specific funding.
Competing Interests
None declared.
Ethics Approval
The study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital, Korea and The Catholic University of Korea, Seoul, Korea (approval ID: KC15EISI0768).
References
- 1.Wong CC, Tsoh JY, Tong EK, Hom FB, Cooper B, Chow EA (2008) The Chinese community smoking cessation project: a community sensitive intervention trial. J Community Health 33, 363–73. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health and Welfare. No Smoke Guide. http://www.nosmokeguide.or.kr/mbs/nosmokeguide/ Accessed 9 March 2016 (in Korean).
- 3.U.S Department of Health and Human Services (2014) The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA. [Google Scholar]
- 4.Kahende JW, Loomis BR, Adhikari B, Marshall L (2009) A review of economic evaluations of tobacco control programs. Int J Environ Res Public Health 6, 51–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iliceto P, Fino E, Pasquariello S, D’Angelo Di Paola ME, Enea D (2013) Predictors of success in smoking cessation among Italian adults motivated to quit. J Subst Abuse Treat 44, 534–40. [DOI] [PubMed] [Google Scholar]
- 6.White M, Bush J, Kai J, Bhopal R, Rankin J (2006) Quitting smoking and experience of smoking cessation interventions among UK Bangladeshi and Pakistani adults: the views of community members and health professionals. J Epidemiol Community Health 60, 405–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kouketsu T, Gokan Y, Ishihara T, Tamaoki M, Gotoh T, Kobayashi S (2013) Factors associated with smoking continuation or cessation in men upon learning of their partner’s pregnancy. Nihon Koshu Eisei Zasshi 60, 212–21. [PubMed] [Google Scholar]
- 8.Ham DC, Przybeck T, Strickland JR, Luke DA, Bierut LJ, Evanoff BA (2011) Occupation and workplace policies predict smoking behaviors: analysis of national data from the current population survey. J Occup Environ Med 53, 1337–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Amelsvoort LG, Jansen NW, Kant I (2006) Smoking among shift workers: More than a confounding factor. Chronobiol Int 23, 1105–13. [DOI] [PubMed] [Google Scholar]
- 10.Kouvonen A, Kivimäki M, Virtanen M, Pentti J, Vahtera J (2005) Work stress, smoking status, and smoking intensity: an observational study of 46,190 employees. J Epidemiol Community Health 59, 63–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bosdriesz JR, Willemsen MC, Stronks K, Kunst AE (2015) Socioeconomic inequalities in smoking cessation in 11 European countries from 1987 to 2012. J Epidemiol Community Health 69, 886–92. [DOI] [PubMed] [Google Scholar]
- 12.Corsi DJ, Subramanian SV, Lear SA, Chow CK, Teo KK, Boyle MH (2013) Co-variation in dimensions of smoking behaviour: a multivariate analysis of individuals and communities in Canada. Health Place 22, 29–37. [DOI] [PubMed] [Google Scholar]
- 13.Korea Center for Disease Control and Prevention (The Guidelines for the use of Korea National Health and Nutrition Examination Survey V (2010–2012) (in Korean).
- 14.Myong JP, Kim HR, Choi SE, Koo JW (2013) Dose-related effect of urinary cotinine levels on bone mineral density among Korean females. Osteoporos Int 24, 1339–46. [DOI] [PubMed] [Google Scholar]
- 15.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction 88, 791–804. [DOI] [PubMed] [Google Scholar]
- 16.Agaku IT, King BA, Dube SR; Centers for Disease Control and Prevention (CDC) (2014) Current cigarette smoking among adults - United States, 2005–2012. MMWR Morb Mortal Wkly Rep 63, 29–34. [PMC free article] [PubMed] [Google Scholar]
- 17.Freund KM, D’Agostino RB, Belanger AJ, Kannel WB, Stokes J 3rd (1992) Predictors of smoking cessation: the Framingham Study. Am J Epidemiol 135, 957–64. [DOI] [PubMed] [Google Scholar]
- 18.Karasek RA Jr. (1979) Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 24, 285–308. [Google Scholar]
- 19.Leidner R. (1999) Emotional labor in service work. Ann Am Acad Pol Soc Sci 561, 81–95. [Google Scholar]
- 20.Wharton AS. (1993) The affective consequences of service work managing emotions on the job. Work Occup 20, 205–32. [Google Scholar]
- 21.Emmanuel SC, Phe A, Chen AJ (1988) The impact of the anti-smoking campaign in Singapore. Singapore Med J 29, 233–9. [PubMed] [Google Scholar]
- 22.Tanaka H, Yamato H, Tanaka T, Kadowaki T, Okamura T, Nakamura M, Okayama A, Ueshima H; HIPOP-OHP research group (2006) Effectiveness of a low-intensity intra-worksite intervention on smoking cessation in Japanese employees: a three-year intervention trial. J Occup Health 48, 175–82. [DOI] [PubMed] [Google Scholar]
- 23.Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M (2012) Socioeconomic status and smoking: a review. Ann N Y Acad Sci 1248, 107–23. [DOI] [PubMed] [Google Scholar]
- 24.Siahpush M, Borland R, Scollo M (2003) Smoking and financial stress. Tob Control 12, 60–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKee SA, Weinberger AH (2013) How can we use our knowledge of alcohol-tobacco interactions to reduce alcohol use? Annu Rev Clin Psychol 9, 649–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jung-Choi KH, Khang YH, Cho HJ (2012) Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob Control 21, 536–42. [DOI] [PubMed] [Google Scholar]
- 27.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S (1994) The validity of self-reported smoking: a review and meta-analysis. Am J Public Health 84, 1086–93. [DOI] [PMC free article] [PubMed] [Google Scholar]