Abstract
Existing evidence on the association between built environment and cardiovascular disease (CVD) risk factors focused on the general population, which may not generalize to higher risk subgroups such as those with lower socio-economic status (SES). We examined the associations between distance to 5 public amenities from residential housing (public polyclinic, subsidized private clinic, healthier eatery, public park and train station) and 12 CVD risk factors (physical inactivity, medical histories and unhealthy dietary habits) among a study sample of low income Singaporeans aged ≥ 40 years (N = 1972). Using data from the Singapore Heart Foundation Health Mapping Exercise 2013–2015, we performed a series of logistic mixed effect regressions, accounting for clustering of respondents in residential blocks and multiple comparisons. Each regression analysis used the minimum distance (in km) between residential housing and each public amenity as an independent continuous variable and a single risk factor as the dependent variable, controlling for demographic characteristics. Increased distance (geographical inaccessibility) to a train station was significantly associated with lower odds of participation in sports whereas greater distance to a subsidized private clinic was associated with lower odds of having high cholesterol diagnosed. Increasing distance to park was positively associated with higher odds of less vegetable and fruits consumption, deep fried food and fast food consumption in the preceding week/month, high BMI at screening and history of diabetes, albeit not achieving statistical significance. Our findings highlighted potential effects of health-promoting amenities on CVD risk factors in urban low-income setting, suggesting gaps for further investigations.
Keywords: Cardiovascular risk, Urban health, Socioeconomic status, Singapore, Health promotion, Primary prevention
Highlights
-
•
We examined associations between access to 5 amenities and 12 CVD risk factors.
-
•
Only 2/60 associations were statistically significant.
-
•
Poorer access to train station was associated with lower odds of sports.
-
•
Poorer access to primary care was associated with lower high cholesterol diagnosis.
1. Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality worldwide, accounting for almost half of all non-communicable disease deaths (Laslett et al., 2012). Poor lifestyle behaviors (Cahill et al., 2014) such as physical inactivity and consumption of unhealthy diet are well known CVD risk factors that could lead to obesity and many associated diseases such as heart attack.
Adherence to healthy lifestyle has a substantial effect in reducing CVD morbidity and mortality (Chiuve et al., 2006, Odegaard et al., 2011, Åkesson et al., 2014) independent of pharmacological treatment (Chiuve et al., 2006), thus serving as a promising target for interventions. Based on the social ecological model of health promotion (Golden et al., 2015, McLeroy et al., 1988), such interventions should adopt a population approach by targeting multiple levels of influence including the institution, the community and the built environment to create a coherent and conducive setting for behavioral change. Therefore, while conventional interventions tend to focus on the knowledge, attitude and health literacy of individuals, researchers and policy makers are paying more attention to the influence of the environment.
Existing studies have examined the association between access to public amenities (such as public park (Bancroft et al., 2015, Sallis et al., 2016), public transportation (Sallis et al., 2016, Badland and Schofield, 2005), fast food restaurants (Reitzel et al., 2014) and primary care facilities (Wee et al., 2016)) and CVD risk factors (such as physical inactivity, obesity, unhealthy diet and lack of preventive health screening). However, most of them focused on the general population within the US or Europe as highlighted by recent systematic reviews (Papas et al., 2007, Ding and Gebel, 2012). This limits the generalizability of the findings to other settings and population subgroups such as individuals with lower socio-economic status (SES) who are known to have higher CVD risk (Clark et al., 2009) as well as poorer disease awareness, treatment and control (Wee & Koh, 2012). Besides fast food restaurants, there may also be other unhealthy food sources relevant in different cultural contexts. For instance, in Singapore, a multicultural island city state in South East Asia, hawker centers typically serve ready-to-eat street foods that contain more fat and fewer vegetables (Soon & Lam, 2008). They form an integral part of Singaporean's life and culture – almost half (49.3%) of adult Singaporeans dine at hawker centers six or more times per week due to busy lifestyle and affordable price (Soon et al., 2008, Health Promotion Board, 2004) – and are recognized as potential contributors to the rising rates of obesity in the country (Soon & Lam, 2008).
Our study examined the association between distance from residential housing to 5 health-promoting public amenities (public polyclinic, subsidized private clinic, healthier eatery, public park and train station) and 12 CVD risk factors (two variables on physical inactivity, five medical histories and five unhealthy dietary habits) among a low-income group living in subsidized rental flats in Singapore. The national median monthly household income of Singapore is $6000 (USD). Lower income individuals are defined as those with a monthly household income less than $1995 (USD) (Department of Statistics Singapore, 2016a) and are eligible to live in subsidized rental flats under the public housing scheme (Housing & Development Board Singapore, 2013). Our study addresses the evidence gap in urban low-income setting as well as local policy needs.
2. Methods
2.1. Hypotheses
Singapore has a total land area 719.7 sq.-km (approximately 65% the size of Hong Kong) with a population of 5 million. Primary care in Singapore is provided by public polyclinics and private general practitioners (GPs) (Khoo et al., 2014). Public polyclinics provide care at subsidized rates to all residents whereas within the private sector, the means-tested Community Health Assist Scheme (CHAS) scheme allows low and middle income Singaporean residents to receive subsidized medical and dental care from participating private GPs (CHAS clinics, hereafter addressed as “subsidized private clinics”) (Ministry of Health Singapore, 2016). Despite their small numbers compared to their private counterparts (18 polyclinics vs > 2000 GP clinics), the polyclinics manage 55% chronic disease patients in the country (Khoo et al., 2014). Access to primary care has been associated with favorable behaviors such as higher uptake of cardiovascular screening (Wee et al., 2016) and preventive care (Starfield et al., 2005) which are important for the management of CVD. Therefore we hypothesized that living further away from these amenities would be associated with higher CVD risk.
Healthier eateries are canteens or restaurants endorsed and funded by the Singapore Health Promotion Board to provide beverages lower in sugar and food lower in calories, use healthier ingredients, serve more fruits and vegetables and incorporate less deep fried food in their menus (Health Promotion Board, 2015). Thus, we hypothesized that living further away from healthier eateries is associated with higher CVD risk, especially those related to unhealthy dietary habits.
The number of parks (Sallis et al., 2016) and access to public transport (Sallis et al., 2016) in a residential area have been associated with higher physical activities. Singapore has a well-connected train network (144 mass rail transit and light rail transit stations) with 2.5 million passenger trips a day, which approximate to 36% total public transport utilization in 2014). (Authority, 2015) Thus we also hypothesized that longer distance away to a park and to a train station were associated with an increase in CVD risk (Sallis et al., 2016).
2.2. Data sources
We obtained the spatial data (shapfiles) from the Singapore Land Authority (SLA) website (Singapore Land Authority, 2016) (subsidized private clinics, healthier eateries, public parks) or identified the locations of the amenities based on official addresses published on websites (train stations, public polyclinic, residential flats).
We obtained individual level data between 2013 and 2015 from the Singapore Heart Foundation Health Mapping Exercise (HME), a door-to-door annual health screening program for low income residents living in public rental flats in Singapore. (Singapore Heart Foundation, 2012) Public rental flats are publicly administered residential flats providing affordable housing for those with low income. In addition to demographic characteristics of individuals who responded to the invitation to health screening program, the data contained 12 CVD risk factors. Specifically, physical inactivity (two variables) included walking < 30 min every day last week and participated in sports < once a week; medical histories (five variables) included hypertension, diabetes, high cholesterol, heart attack and high BMI; unhealthy dietary habits (five variables) included consumption of fast food in the past one month, consumption of deep fried food, vegetables, fruits in the past one week and frequency of dining at hawker center in the past one week. Besides body mass index (BMI) which were measured by trained volunteers at screening, all variables were self-reported.
We obtained ethics approval from the National University of Singapore Institutional Review Board.
2.3. Inclusion & exclusion criteria
We limited our analysis to respondents ≥ 40 years old given their higher risk of CVD. To simplify the analyses, we considered the first participation to the health screening program. In addition, we removed a small number of respondents (n = 40, 1.7%) with > 2 year differences between reported and calculated age based on year of birth as a criteria for poor recall. The final analysis sample contained 1972 respondents.
2.4. Statistical analysis
We investigated the associations between the minimum distances from the residential housing of each respondent to the 5 public amenities (public polyclinic, subsidized private clinic, healthier eatery, public park and train station) and 12 CVD risk factors. As respondents clustered in residential blocks, we performed a series of logistic mixed effect regression models, specifying the residential blocks as the random effect. Each regression analysis used the minimum distance (in km) between residential housing and each public amenity as an independent continuous variable and a single risk factor as the dependent variable, controlling for demographic characteristics (gender, age group, housing type, marital and employment status).
For consistency, all risk factors were represented as binary variables such that the regressions are predicting higher risks or undesirable outcomes, notably walking < 30 min every day last week, participated in sports < once a week and less regular consumption of vegetables (0–2 days in the past one week), less regular consumption of fruits (0–2 days in the past one week) and regular dining at hawker center (3–7 days in the past one week). We categorized respondents' age into four groups: 40–64; 65–74, 75–84, ≥ 85. Individuals ≥ 85 years old are considered the oldest old in literature (Campion, 1994, Dodge et al., 2008) and are beyond the life expectancy of Singaporeans (83 years old (Department of Statistics Singapore, 2016b)), therefore we did not divide the oldest age group further. We grouped BMI at screening into high or low based on World Health Organization's recommended cutoff for Asians (World Health Organization Expert Consultation, 2004), i.e. BMI ≥ 23. For all regressions, we reported results as odds ratios (OR) with 95% confidence intervals (95%CI).
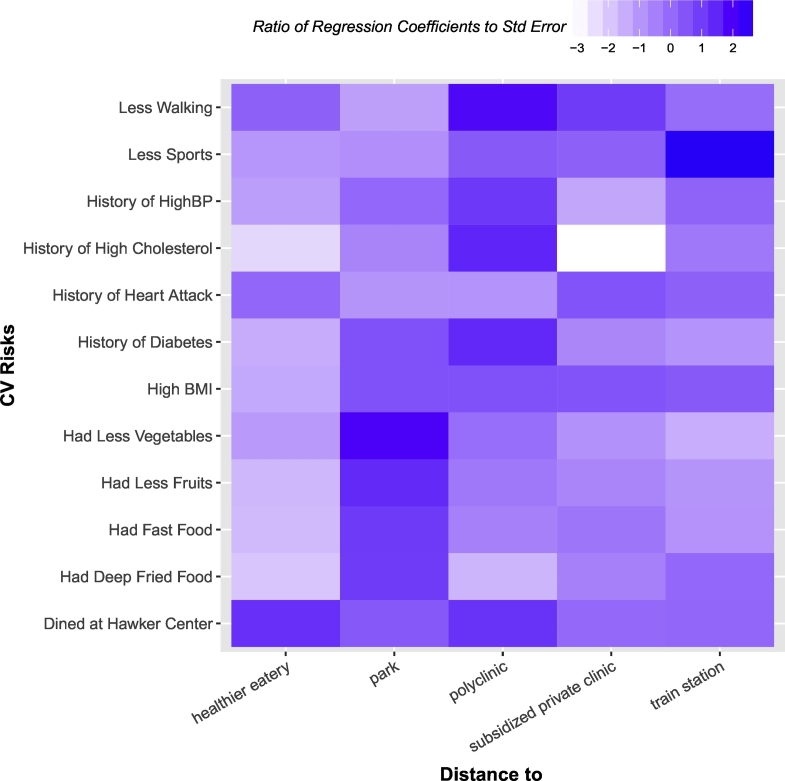
To visualize the relationship between the different amenities and risk factors, we generated a heatmap based on the ratio of regression coefficient to its standard errors. To account for multiple comparisons, we used the false discovery rate (FDR, defined as the expected proportions of false positives among total number of positive associations (Benjamini & Hochberg, 1995)). This has been recommended for health studies as an alternative to the Bonferroni adjustment to avoid the problem of inflated Type II error rates (Glickman et al., 2014). Unlike p-value, there is no conventional threshold for FDR. We set our FDR threshold at 0.20 based on previous literature in epidemiology (Loftfield et al., 2015, Patel et al., 2010).
We used QGIS 2.10.1 for processing the spatial data and R 3.2.4 for data processing and analysis.
3. Results
3.1. Sample characteristics
Table 1 describes the characteristics of the 1972 respondents. Most respondents were females (52.8%) within working age group (40–64 years old, 47%). On average, they lived within 0.5 km of a subsidized private clinic (0.23 ± 0.13 km) and a healthier eatery (0.39 ± 0.21 m); within 1 km of the nearest train station (0.70 ± 0.34 km). The distance from their residential housing to the nearest park and the nearest polyclinic were 1.07 ± 0.61 m and 2.57 ± 2.59 km respectively.
Table 1.
Characteristics of participants in Health Mapping Exercise 2013–2015.
| Variable | N | (%) |
|---|---|---|
| Demographic characteristics | ||
| Gender | ||
| Male | 931 | 47.2 |
| Female | 1041 | 52.8 |
| Age group | ||
| 40–64 | 926 | 47.0 |
| 65–74 | 517 | 26.2 |
| 75–84 | 399 | 20.2 |
| ≥ 85 | 130 | 6.6 |
| Marital status | ||
| Married | 467 | 23.7 |
| Single | 747 | 37.9 |
| Separated/Divorced | 258 | 13.1 |
| Widowed | 348 | 17.6 |
| Employment status | ||
| Yes | 443 | 22.5 |
| No | 1443 | 73.2 |
| Ethnic group | ||
| Chinese | 1208 | 61.3 |
| Malay | 553 | 28.0 |
| Indian | 183 | 9.3 |
| Others | 28 | 1.4 |
| Housing type | ||
| 1-Room | 1213 | 61.5 |
| 2-Room | 747 | 37.9 |
| Physical activities | ||
| Walked < 30 min every day last week | ||
| Yes | 494 | 25.1 |
| No | 1422 | 72.1 |
| Had sports < once a week | ||
| Yes | 1125 | 57.0 |
| No | 777 | 39.4 |
| Dietary habits | ||
| Ate deep fried food in the past one week | ||
| Yes | 1104 | 56.0 |
| No | 798 | 40.5 |
| How often did you eat at hawker center in the past one week? | ||
| 3–7 Days | 886 | 44.9 |
| 0–2 Days | 1027 | 52.1 |
| How often did you eat vegetables in the past one week? | ||
| 3–7 Days | 1548 | 78.5 |
| 0–2 Days | 377 | 19.2 |
| Ate fast food in the past one month? | ||
| Yes | 339 | 20.2 |
| No | 1498 | 76.0 |
| How often did you eat fruits in the past one week? | ||
| 3–7 Days | 1252 | 63.5 |
| 0–2 Days | 659 | 33.4 |
| Medical histories | ||
| Hypertension | ||
| Yes | 917 | 46.5 |
| No | 983 | 49.8 |
| Diabetes | ||
| Yes | 466 | 23.6 |
| No | 1418 | 71.9 |
| Heart attack | ||
| Yes | 169 | 8.6 |
| No | 1724 | 87.4 |
| High cholesterol | ||
| Yes | 798 | 40.5 |
| No | 1055 | 53.5 |
| Body mass index, kg/m2 | ||
| ≥ 23 | 955 | 48.4 |
| < 23 | 898 | 45.5 |
| Minimum distance to (Mean ± SD, km) | ||
| Train station | 0.70 ± 0.34 | |
| Healthier eatery | 0.39 ± 0.21 | |
| Park | 1.07 ± 0.61 | |
| Public polyclinic, | 2.57 ± 2.59 | |
| Subsidized private clinic (CHAS clinic) | 0.23 ± 0.13 |
Notes: Percentages may not add up to 100% due to missing data.
Abbreviations: Community Health Assist Scheme (CHAS).
3.2. Strength & direction of associations
Fig. 1 illustrates the associations between the distance from residential housing to public amenities and CVD risk factors from the regression analyses controlling for demographic characteristics without accounting for multiple comparisons. As all 5 amenities are suggested to be health-promoting (refer Methods), living further away from these amenities (indicating increasing geographical inaccessibility) should be positively associated with the CVD risk factors i.e. regression coefficient > 0.
Fig. 1.
The heatmap illustrates the associations between cardiovascular risk factors (y-axis) and distances to amenities (x-axis) among our study samples, after adjusting for demographic characteristics (gender, age group, housing type, marital and employment status). All CVD risk factors are binary. The heatmap presents the ratio of estimated coefficient to its standard error. Darker shade indicates higher odds of having a specific CVD risk factor as the distance to a specific amenity increases (suggesting inaccessibility to the amenity is a risk factor). In contrast, lighter shade indicates lower odds of having a specific CVD risk factor as the distance to a specific amenity increases (suggesting inaccessibility to the amenity is protective against the CVD risk factors). High BMI refers to BMI > 23 kg/m2. All risk factors were self-reported, except BMI which was measured by trained volunteers.
In the heatmap, a darker shade of blue reflects stronger evidence toward positive association, which suggests that geographical inaccessibility to the amenity is a risk factor. Two examples were the association between distance to train station and low participation (< once a week) in sports (Less Sports) and the association between distance to park and consumption of vegetables for 0–2 days in the past one week (Less Vegetable).
In contrast, a white color indicates a highly significant negative association and suggests that geographical inaccessibility to the amenity is protective against the CVD risk factor instead. One example is the association between subsidized private clinics and a history of high cholesterol.
3.3. Associations with FDR < 0.20
Only two associations in Fig. 1 fell below the pre-specified FDR < 0.20 cutoff, summarized in Table 2. An additional 1 km distance from residential block to the nearest train station was associated with higher odds of not participating in sports (OR 1.73; 95% CI 1.18–2.55). In contrast, an additional 1 km distance from a subsidized private clinic was associated with lower odds of having a history of high cholesterol (OR 0.27; 95% CI 0.12 - 0.61). The direction of association and statistical significance for the two regressions remained even after respondents with self-reported stroke and heart attack from analyses were excluded. Interestingly, our analysis found no association between distances to the public amenities with unhealthy dietary habits such as fast food consumption.
Table 2.
Distance measures significantly associated with cardiovascular risk factors among participants in Health Mapping Exercise 2013–2015.
| CVD risk | Amenities | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|---|
| Had sports less than once a week | Train station | 1.73 | 1.18–2.55 | 0.006 |
| History of high cholesterol | Subsidized private clinic | 0.27 | 0.12–0.61 | 0.002 |
4. Discussion
We used a systematic multiple outcome-exposure analysis approach to identify the association between distance to 5 health-promoting public amenities and 12 CVD risk factors among the population with low SES in the urban city state of Singapore. Accounting for multiple comparisons, our findings suggest that CVD risk factors among our study sample may be amenable by geographical access to health-promoting public amenities. This has implications in population health strategies to mitigate CVD risk factors among the socio-economically disadvantaged population living in the city state. To the best of authors' knowledge, our study is also the first in the Asian Pacific region to explore the associations between distance to public amenities and CVD risk factors.
Our results imply that those living closer to subsidized private clinics may have benefited from the free health screening under the subsidy scheme, which included cholesterol testing (Health Promotion Board, 2014). This may explain the reduction in the odds of a diagnosis of high cholesterol with increasing distance from a subsidized private clinic. Meanwhile, the associations for the other three medical histories (diabetes, hypertension and heart attack) did not achieve statistical significance although the odds ratios were in the favorable direction. As these diseases are often symptomatic unlike high cholesterol, patients may have sought healthcare to address their symptoms regardless of their access to a subsidized private clinic.
Our analysis also suggests that living further from the nearest train station is associated with higher odds of not exercising regularly (at least once a week). There are two plausible explanations. Those who resided further from a train station may have poorer access to sports and recreation activities compared to those who lived closer. They would also need to walk further to access the public transport and hence have less need or time to be active in sports (Badland & Schofield, 2005). The latter may be the case for our study samples as 72.1% respondents reported walking ≥ 30 min every day. Further studies may be required to explore the underlying reasons given its potential impact on urban design and health promotion.
Interestingly out of the 60 hypotheses, only two (3.3%) achieved statistical significance after accounting for multiple comparisons. It was possible that individual factors such as age, gender and employment status played a stronger role than access to public amenities among our socio-economically disadvantaged study samples. Several studies found that proximity to park was significantly associated with higher physical activities (Bancroft et al., 2015, Sallis et al., 2016). In our analyses, increasing distance (geographical inaccessibility) to park was positively associated with higher odds of less vegetable and fruits consumption, deep fried food and fast food consumption in the preceding week/month, high BMI at screening and a history of diabetes, although our analyses did not achieve statistical significance (results in Supplementary Table 1). Proximity to park and availability of park facilities may not necessarily translate to park use or park-based physical activities and the effect may vary across different demographic groups (Kaczynski et al., 2014). Similarly, we also observed a non-significant positive association between increasing distance to healthier eatery and higher odds of dining at hawker center. In the US, policies to increase access to healthy grocery stores and supermarkets in poorer neighborhoods have been shown to merely improve awareness without a change in dietary habits (Cummins et al., 2014), suggesting that having access to healthy food source alone may not be sufficient to reduce CVD risk although we could not discount any potential benefits which may take longer to manifest.
5. Limitations
As participation in HME was voluntary, the respondents may not be fully representative of all individuals with low SES in Singapore. Most individual data were self-reported by the respondents and may be subjected to recall and social desirability bias. In addition, our cross sectional design cannot establish causality. Besides distance to the nearest of each amenity, density of the amenities within certain radius from residential housing is also an alternative proxy of access (Bancroft et al., 2015, Reitzel et al., 2014). Nevertheless, due to the lack of local literature to guide assumptions on the travel radius to access each amenity and the small land area of Singapore, we considered the distance to the nearest amenity as a more meaningful proxy of access.
The adjustment for multiple comparisons may have introduced type II errors i.e. erroneously rejecting true associations between distance and risk factor. While combining related risk factors e.g. unhealthy dietary habits into a score variable may reduce the number of hypotheses, it would require the use of locally validated scales e.g. structured food frequency questionnaire validated against 24-h dietary recall interviews (Hankin et al., 2001) and biomarkers (Seow et al., 1998), which was not supported by our data. Nevertheless, by examining specific CVD risk factors our analysis highlighted two associations that may merit further investigations which would otherwise be impossible if the risk factors were aggregated into a score.
Due to the lack of income and education level data, we adjusted the regressions for housing type and employment status as proxies of SES (Housing & Development Board Singapore, 2013) as our respondents must undergo means testing to be eligible for the subsidized public housing and would therefore fall under the same income bracket. Our results assumed the geographical distributions of the amenities were static throughout 2013 to 2015 which may also not be true. Lastly, we estimated straight line distances from residences to the amenities. Nonetheless, given the extensive road and public transport network in Singapore, they likely does not differ much from the actual road distances, especially for subsidized private clinics and healthier eateries located within 200 to 400 m from the residences. There is also evidence that straight line distance is a valid proxy for traveling distance and time (Bliss et al., 2012).
6. Conclusion
Our results provide insights into the relationship of distance from residence to several public amenities with CVD risk factors among a sample of lower income Singaporeans. In particular, geographical inaccessibility to the nearest train station was associated with less regular participation in sports and living further from subsidized private clinics was associated with lower odds of having diagnosed high cholesterol. While not establishing causality, our findings may warrant further investigations to better target health-promoting activities among individuals with lower SES.
The following is the supplementary data related to this article.
Odds ratios (OR) and 95% confidence intervals (CI) for all 75 regression analyses.
Conflict of interest
The study involved no funding. The authors declare that they have no conflict of interest.
Transparency document
Transparency document.
Acknowledgments
Acknowledgment
We would like to our express our gratitude to the Singapore Heart Foundation Health Mapping Exercise Team for their support to this project. We would also like to thank Associate Professor Alex Cook from National University of Singapore for his technical advice.
Footnotes
The Transparency document associated with this article can be found, in online version.
Contributor Information
K.K. Lim, Email: limkk@u.duke.nus.edu.
Y.H. Kwan, Email: yuheng@u.duke.nus.edu.
C.S. Tan, Email: chuen_seng_tan@nuhs.edu.sg.
L.L. Low, Email: low.lian.leng@singhealth.com.sg.
A.P. Chua, Email: ai_ping_chua@juronghealth.com.sg.
H.Y. Tay, Email: hungyong@heart.org.sg.
S.Y. Chan, Email: phacsy@nus.edu.sg.
T. Ostbye, Email: truls.ostbye@duke-nus.edu.sg.
References
- Åkesson A., Larsson S.C., Discacciati A., Wolk A. Low-risk diet and lifestyle habits in the primary prevention of myocardial infarction in men. J. Am. Coll. Cardiol. 2014;64(13):1299–1306. doi: 10.1016/j.jacc.2014.06.1190. [DOI] [PubMed] [Google Scholar]
- Authority Singapore Land Transport. Singapore land transport statistics in brief. Dermatol. Sin. 2015 [Google Scholar]
- Badland H., Schofield G. Transport, urban design, and physical activity: an evidence-based update. Transp. Res. Part D: Transp. Environ. 2005;10(3):177–196. [Google Scholar]
- Bancroft C., Joshi S., Rundle A. Association of proximity and density of parks and objectively measured physical activity in the United States: a systematic review. Soc. Sci. Med. 2015;138:22–30. doi: 10.1016/j.socscimed.2015.05.034. [DOI] [PubMed] [Google Scholar]
- Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol. 1995;57(1):289–300. [Google Scholar]
- Bliss R.L., Katz J.N., Wright E.A., Losina E. Estimating proximity to care: are straight line and zipcode centroid distances acceptable proxy measures? Med. Care. 2012;50(1):99–106. doi: 10.1097/MLR.0b013e31822944d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill L.E., Pan A., Chiuve S.E. Fried-food consumption and risk of type 2 diabetes and coronary artery disease: a prospective study in 2 cohorts of US women and men. Am. J. Clin. Nutr. 2014;100(2):667–675. doi: 10.3945/ajcn.114.084129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion E.W. The oldest old. N. Engl. J. Med. 1994;330(25):1819–1820. doi: 10.1056/NEJM199406233302509. [DOI] [PubMed] [Google Scholar]
- Chiuve S.E., McCullough M.L., Sacks F.M., Rimm E.B. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006;114(2):160–167. doi: 10.1161/CIRCULATIONAHA.106.621417. [DOI] [PubMed] [Google Scholar]
- Clark A.M., DesMeules M., Luo W., Duncan A.S., Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat. Rev. Cardiol. 2009;6(11):712–722. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- Cummins S., Flint E., Matthews S.A. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014;33(2):283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Statistics Singapore . Singapore. 2016. Key household income trends 2015. [Google Scholar]
- Department of Statistics Singapore . Singapore. 2016. Population trends 2016. [Google Scholar]
- Ding D., Gebel K. Built environment, physical activity, and obesity: what have we learned from reviewing the literature? Health Place. 2012;18(1):100–105. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- Dodge H.H., Kita Y., Takechi H., Hayakawa T., Ganguli M., Ueshima H. Healthy cognitive aging and leisure activities among the oldest old in Japan: Takashima Study. J. Gerontol. A Biol. Sci. Med. Sci. 2008;63(11):1193–1200. doi: 10.1093/gerona/63.11.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glickman M.E., Rao S.R., Schultz M.R. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J. Clin. Epidemiol. 2014;67(8):850–857. doi: 10.1016/j.jclinepi.2014.03.012. [DOI] [PubMed] [Google Scholar]
- Golden S.D., McLeroy K.R., Green L.W., Earp J.A., Lieberman L.D. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health education & behavior: the official publication of the Society for Public Health Education. 2015;42:8s–14s. doi: 10.1177/1090198115575098. (1 Suppl) [DOI] [PubMed] [Google Scholar]
- Hankin J.H., Stram D.O., Arakawa K. Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr. Cancer. 2001;39(2):187–195. doi: 10.1207/S15327914nc392_5. [DOI] [PubMed] [Google Scholar]
- Health Promotion Board . Singapore. 2004. Report of the National Nutrition Survey. [Google Scholar]
- Health Promotion Board Subsidies for Health Screening and Follow-up FAQs. 2014. http://www.hpb.gov.sg/HOPPortal/health-article/HPB054805
- Health Promotion Board Healthier Dining Programme. 2015. http://www.hpb.gov.sg/HOPPortal/programmes-article/HPB063209
- Housing & Development Board Singapore . Singapore. 2013. Public housing in Singapore: residents' profile, housing satisfaction and preferences, HDB Sample Household Survey 2013. [Google Scholar]
- Kaczynski A.T., Besenyi G.M., Stanis S.A. Are park proximity and park features related to park use and park-based physical activity among adults? Variations by Multiple Socio-demographic Characteristics. TheIinternational Journal of Behavioral Nutrition and Physical Activity. 2014;11:146. doi: 10.1186/s12966-014-0146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo H.S., Lim Y.W., Vrijhoef H.J.M. Primary healthcare system and practice characteristics in Singapore. Asia Pacific Family Medicine. 2014;13(1):8. doi: 10.1186/s12930-014-0008-x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4129466/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laslett L.J., Alagona P., Jr., Clark Iii B.A. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology. J. Am. Coll. Cardiol. 2012;60:S1–S49. doi: 10.1016/j.jacc.2012.11.002. (25, Supplement) [DOI] [PubMed] [Google Scholar]
- Loftfield E., Shiels M.S., Graubard B.I. Associations of coffee drinking with systemic immune and inflammatory markers. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology. 2015;24(7):1052–1060. doi: 10.1158/1055-9965.EPI-15-0038-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Ministry of Health Singapore What Is CHAS? 2016. https://www.chas.sg/default.aspx
- Odegaard A.O., Koh W.-P., Gross M.D., Yuan J.-M., Pereira M.A. Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: the Singapore Chinese Health Study. Circulation. 2011;124(25):2847–2854. doi: 10.1161/CIRCULATIONAHA.111.048843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papas M.A., Alberg A.J., Ewing R., Helzlsouer K.J., Gary T.L., Klassen A.C. The built environment and obesity. Epidemiol. Rev. 2007;29(1):129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Patel C.J., Bhattacharya J., Butte A.J. An Environment-Wide Association Study (EWAS) on type 2 diabetes mellitus. PLoS One. 2010;5(5) doi: 10.1371/journal.pone.0010746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitzel L.R., Regan S.D., Nguyen N. Density and proximity of fast food restaurants and body mass index among African Americans. Am. J. Public Health. 2014;104(1):110–116. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Cerin E., Conway T.L. Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. Lancet. 2016 doi: 10.1016/S0140-6736(15)01284-2. (London, England) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seow A., Shi C.Y., Chung F.L. Urinary total isothiocyanate (ITC) in a population-based sample of middle-aged and older Chinese in Singapore: relationship with dietary total ITC and glutathione S-transferase M1/T1/P1 genotypes. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 1998;7(9):775–781. [PubMed] [Google Scholar]
- Singapore Heart Foundation 2012. http://www.myheart.org.sg/article/school-programmes/all/about/151 Health Mapping Exercise (HME)
- Singapore Land Authority OneMap. 2016. http://www.onemap.sg/index.html
- Soon G., Koh Y.H., Wong M.L., Lam P.W. Washington, US. 2008. Obesity prevention and control efforts in Singapore. [Google Scholar]
- Starfield B., Shi L., Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee L.E., Koh G.C. Individual and neighborhood social factors of hypertension management in a low-socioeconomic status population: a community-based case-control study in Singapore. Hypertension Research: Official Journal of the Japanese Society of Hypertension. 2012;35(3):295–303. doi: 10.1038/hr.2011.187. [DOI] [PubMed] [Google Scholar]
- Wee L.E., Cher W.Q., Sin D., Li Z.C., Koh G.C. Primary care characteristics and their association with health screening in a low-socioeconomic status public rental-flat population in Singapore - a mixed methods study. BMC Fam. Pract. 2016;17:16. doi: 10.1186/s12875-016-0411-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. (London, England) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Odds ratios (OR) and 95% confidence intervals (CI) for all 75 regression analyses.
Transparency document.