Abstract
Statement of the Problem:
Temporomandibular disorder (TMD) is a clinical term used for clinical signs and symptoms that affect the temporomandibular joints, masticatory muscles, and associated structures. Surgical and non-surgical treatments can be used for management of TMD. Non-surgical route is the main part of the treatment, since clinicians prefer non-aggressive treatment for TMD such as pharmacological and physical therapy. Low-level laser therapy (LLLT) and transcutaneous electrical nerve stimulation (TENS) are the main procedures in physical therapy.
Purpose:
The aim of this study was to evaluate the effectiveness of TENS and LLLT in treatment of TMD patients who did not respond to pharmacological therapy.
Materials and Method:
This clinical trial was performed on 45 patients who randomly received either TENS or LLLT for 8 sessions. LLLT was applied with diode laser (Ga-Al-As, 980nm, dose 5j/cm2) and TENS by using two carbon electrodes with 75 Hz frequency (0.75 msec pulse width). Helkimo index and visual analogue scale (VAS) were measured during the treatment period and throughout the follow-up sessions.
Results:
Significant reduction in the VAS and Helkimo index was observed in both TENS and LLLT group. There was no significant difference between the two methods during the treatment; however, TENS was more effective in pain reduction in follow-ups.
Conclusion:
This study justified the use of TENS therapy as well as LLLT in drug-resistant TMD. Both were useful in relieving the pain and muscles tenderness, although, TENS was more effective than LLLT.
Keywords: Transcutaneous Electrical Nerve Stimulation , Low Level Light Therapy , Temporomandibular Joint Disorders Syndrome , Pain , Laser , Temporomandibular Joint , Physical Therapy
Introduction
The clinical term of temporomandibular disorder (TM-D) refers to signs and symptoms that influence the temporomandibular joint (TMJ), masticatory muscles, and related structures.[1] Etiologic factors include parafunctional habits, as well as psychological and occlusal factors.[2-3] Patients with TMD suffer from orofacial pain, muscle tenderness, joint noises, limited mandibular movements, pain in TMJ, headache, and tinnitus.[4-5]
Diagnosis of TMD is based on clinical examination, history, and other methods such as questionnaires (research diagnostic criteria for TMD). Yet, clinical examination is the main part of TMD diagnosis. It consists of measurement of mandibular movements with digital caliper, palpation of masticatory muscles and TMJ, and the use of the stethoscope to assess the joint noises.[6]
Although both surgical and non-surgical treatments are employed to manage TMD, the non-surgical route is the first and main part. It consists of pharmacological therapy such as non-steroidal anti-inflammatory drugs (NSAIDs), antidepressants, and muscle relaxants. The second part includes occlusal and physical therapy such as low-level laser therapy (LLLT), transcutaneous electrical nerve stimulation (TENS) and ultrasound.[7-9]
TENS is one of the safest and most inexpensive modalities that are used to control both chronic and acute pain.[10-11] According to the gate control theory, the modulation of pain perception induced by TENS is attributed to the recruitment of Aβ afferent fibers in the posterior horn of the spinal cord which would prevent the activation of the pain conducted in thin fiber. Electrical stimulation inhibits the transmission of painful impulses through the spinal cord and stimulates the release of endogenous opioid by the brain.[12]
LLLT is used in different fields of medicine like dermatology and physical therapy.[13] It reduces histamine, PGE2 and substance P in the posterior horn of the spinal cord. It also elevates the level of acetylcholinesterase, lymphatic drainage, adenosine triphosphate, and beta-endorphin. That is the reason why this modality is suggested for chronic and acute pain reduction.[14]
Different studies used LLLT for TMD management. Cetiner et al.[15] Shirani et al.[16] and Carvalho et al.[9] used LLLT in TMD patients and reported positive effects especially in pain reduction. In contrast, some studies did not show any significant result.[7,17] Having compared the TENS and pharmacological therapy, Shanavas et al. justified the use of TENS therapy as an adjuvant modality in controlling the pain associated with TMD.[18]
A number of studies compared the effects of LLLT and TENS on patient with TMD. Nunez et al.[19] concluded that LLLT was more effective than TENS in improving the maximum vertical jaw opening. However, Keto et al.[20] showed both therapies to be effective in decreasing the symptoms of patients with TMD. Regarding the limited number of studies on the issue and absence of any similar study on drug-resistant patients, the current study aimed to compare the effects of TENS and LLLT on treatment of drug-resistant TMD patients.
Materials and Method
This clinical trial was performed on 45 patients with drug-resistant TMD who referred to the Department of Oral Medicine, in Shiraz Dental School, Iran. The related research protocol was approved by the Human Research Ethics Committee of Shiraz University of Medical Sciences (process number#IR.SUMS.REC.1394. 124). The informed consents were signed by all patients prior to beginning of the treatment. The exclusion criteria were having five or more missing posterior teeth (except for the third molars), parafunctional habits (bruxism, clenching, and so on), degenerative joint disorder, crepitus sound, and any kind of systemic disease. The enrolled patients were those with panoramic x-ray who used 1000 mg methocarbamol every 8 hours and 100 mg celecoxib every 12 hours for 10 days but did not feel better based on Visual Analog Scale (VAS) and clinical examination. Therefore, the patients discontinued the drugs 3 days before starting the new treatment and during the course of study. If any change was seen in condylar surface or joint space, the patients were referred to radiologist for better evaluation. The patients were examined based on Helkimo index,[21] in which the distance between the incisors was measured by a caliper (Insize, China) and considered as the maximum jaw opening. Ten muscles were palpated according to this index, including deep masseter, superficial masseter, posterior part of temporal, anterior part of temporal, insertion of temporal, lateral pterygoid, medial pterygoid, anterior digastric, posterior digastric and sternocleidomastoid muscles.[22] According to the block randomization, the patients were divided into two groups of TENS and LLLT. The TENS group received treatment for 8 sessions within two weeks (NEURDYN 710L; Iran). Carbone electrodes (6.5×4.5cm) were placed on the tender muscles with 75 HZ frequency and 0.75 millisecond pulse width for 20 minutes per session. The LLLT group received low-level laser therapy for 8 sessions within two weeks. For these patients, Gallium-Aluminum-Arsenide (Ga-Al-As) (Azor-2k-02, 980 nm) was applied on three regions of both sides including the posterior and anterior aspect of the joint, as well as the trigger points. Energy intensity was adjusted to 5 j/cm2 using the output power of 200 mw for 2.5 minutes. The pain intensity was assessed according to VAS and recorded in each session. The clinical evaluation of TMD was checked, using Helkimo index before and after the treatment (in the last session). The patients were followed up 4, 8, and 16 weeks after the treatment and VAS was recorded in these sessions. Data was analyzed by using SPSS software, version 18.0 (SPSS Inc.; IL, USA), and interpreted in form of mean, standard deviation (SD), and frequency (percentage). Paired t-test was used to compare Helkimo index before and after using each device. Student’s t-test was employed to compare the mean differences in Helkimo index and pain intensity (VAS) between the two devices at each time-point. Repeated measures ANOVA was used to assess the changes in pain scores (VAS) over time. p< 0.05 was considered to be significant.
Results
Out of 45 patients, 19 in the TENS and 15 in LLLT group completed the course of treatment. Table 1 represents the demographic data of patients of the two groups. Both groups were similar concerning the mean age and gender (p= 0.79 and p= 0.21, respectively).
Table 1.
Comparison of age and sex in LLLT and TENS group
| Group | Number | Female | Male | Mean age | p.Value (age) | p.Value (sex) |
|---|---|---|---|---|---|---|
| LLLT | 15 | 11 | 4 | 30.79 | 0.79 | 0.21 |
| TENS | 19 | 14 | 5 | 31.87 |
The pre-treatment Helkimo index was 12.20 in LLLT and 11.2 in TENS group, indicating no significant difference between the two groups (p= 0.39). This index decreased significantly in both groups after the treatment (p< 0.001) (Table 2); However, the difference between the two methods was not significant (p= 0.17) (Table 3).
Table 2.
Comparison of the pre- and post-treatment Helkimo Index in each group
| Group | Pre-treatment Helkimo Index (H1) | Post-treatment Helkimo Index (H2) | Differences (H1-H2) | p Value |
|---|---|---|---|---|
| LLLT | 12.20 | 9.07 | 3.13 | <0.001 |
| TENS | 11.21 | 7.00 | 4.21 | <0.001 |
Table 3.
Comparison of post-treatment Helkimo Index between the two groups
| Group | Mean differences (H2-H1) | p Value |
|---|---|---|
| LLLT | -3.13 | 0.17 |
| TENS | -4.21 |
The two groups were not significantly different in terms of pain reduction (VAS) during the treatment course (8 session); however their difference was significant in follow-up sessions (4, 8, 16 weeks after treatment) (Table 4). The VAS was significantly lower in TENS group than LLLT group throughout the follow-ups (p= 0.04, 0.02, 0.025, respectively).
Table 4.
Comparison of VAS between the groups during the treatment
| Group | VAS Mean | p Value | |
|---|---|---|---|
| 1 | LLLT | 7.200 | 0.883 |
| TENS | 7.105 | ||
| 2 | LLLT | 6.553 | 0.457 |
| TENS | 5.74 | ||
| 3 | LLLT | 6.367 | 0.152 |
| TENS | 5.184 | ||
| 4 | LLLT | 6.033 | 0.135 |
| TENS | 4.789 | ||
| 5 | LLLT | 5.867 | 0.059 |
| TENS | 4.263 | ||
| 6 | LLLT | 5.533 | 0.056 |
| TENS | 3.482 | ||
| 7 | LLLT | 5.300 | 0.089 |
| TENS | 3.842 | ||
| 8 | LLLT | 5.520 | 0.0059 |
| TENS | 3.632 | ||
| 9 | LLLT | 5.467 | 0.044 |
| TENS | 3.789 | ||
| 10 | LLLT | 5.633 | 0.027 |
| TENS | 3.816 | ||
| 11 | LLLT | 5.967 | 0.025 |
| TENS | 4.053 | ||
Fallow-up period included 9, 10 and 11 session.
According to Figure 1, the TENS method decreased the pain more rapidly than LLLT. The pain decreased significantly in the TENS group from the second session on (p= 0.016); whereas, in the LLLT group, significant decreased was noticed from the third session on (p= 0.007).
Figure1.
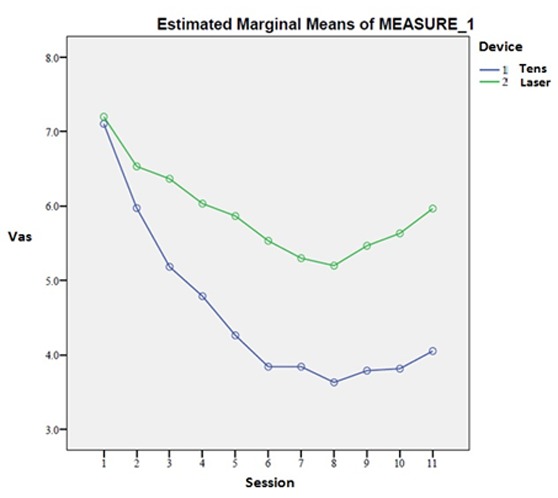
Comparison of VAS between LLLT and TENS group
Discussion
The present study compared the LLLT and TENS in TMD patients who did not respond to pharmacological treatments. Both methods significantly reduced the VAS and Helkimo index. Our result was similar to some previous studies[9,15,23-25] but different from those that reported no significant positive effect.[7,17] Such difference may be due to the sample selection and treatment protocol.
This study found no significant differences between the effectiveness of TENS and LLLT on pain reduction and Helkimo index during the treatment course. Few studies have compared the effectiveness of LLLT and TENS on TMD. Generally, the main results of the current study were similar to what were detected by Kato et al.[20] and Nunez et al.[19] Meanwhile, our findings proved the TENS method to be more effective than LLLT in reducing the pain in follow-ups. It was inconsistent with Nunez et al.’s[19] findings, which reported the LLLT to be more effective than TENS. It may be due to the laser technical differences such as type of the device, power density, or length of the treatment. Furthermore, in Nunez’s study,[19] the patients were evaluated only by their maximum opening score, while, we used a more precise clinical index (Helkimo index) and VAS for pain assessment.
The current study also found that the TENS reduced pain more rapidly than LLLT (after only two sessions). This effect might result from the delayed effect of laser therapy. The patient does not feel anything during LLLT, whereas, TENS creates a minor electrical shock. Therefore, the psychological effect of treatment may contribute to the better result of TENS on pain reduction.
In this study, we evaluated the effects of these two methods on patients who did not respond to pharmacological treatments. To the best of our knowledge, there existed no similar study on drug-resistant TMD patients. During the treatment course in this study, the patients did not use anti-inflammatory drugs; thus, the pain reduction effect of LLLT and TENS was evaluated per se. However, co-intervention by anti-inflammatory drugs was avoided only in some trials.[26] Moreover, selection of this group of patients eliminated the analgesic and muscle spasm effect of medicine, as well.
The equal number of sessions in both groups allowed comparing the effect of these methods in clinically similar situations, whereas, majority of trials continued the treatment for more sessions.[8-9,27-28]It can be declared that the longer duration for LLLT may better control the pain. Nonetheless, it is rational that shorter treatment course with desirable effect increases the cooperation of patients and is clinically more applicable.
Concerning the age and gender of patients with TMD, our results were consistent with those of previous studies; i.e., TMD was more prevalent in females aged 20-40 years old.[29-30]
In the present study, Helkimo index and VAS were measured in both groups, while most other studies measured only VAS or jaw movements.[8,16,19,31] Helkimo index evaluated the jaw movements, muscle tenderness and TMJ sounds, a comprehensive index involved many criteria. The results of Kulekcioglu’s study[30] showed that the pain (subjective criteria) reduced in both placebo and laser group in TMD patients; however, mouth opening (objective criteria) improved only in laser group. Therefore, in the current study, both objective (Helkimo index) and subjective (VAS) parameters were evaluated to rule out the psychological effects of treatments.
VAS decreased in LLLT group during the treatment similar to other studies.[9,15-16,31] In follow-ups, the VAS decreased significantly until 8 weeks. A similar study with the same result followed up the patients for 3 weeks,[26] but in the present study, the patients were followed up longer.
Generally, some patients may need further modalities such as occlusal splint. Moreover, painful and tender muscles delay the beginning of treatment. Application of TENS and LLLT can increase the patient’s cooperation and satisfaction.
Overall, this study found no significant difference between the two modalities, although TENS caused pain reduction to occur more rapid and persist longer, as well. Many of the current patients responded to pharmacological treatments; thus, the sample size was small. Results that are more reliable can be obtained through replication of these findings in a randomized placebo-control clinical trial with larger sample size. The patients did not cooperate for more follow-up sessions, although longer follow-up sessions could help in more precise evaluating the persistence of treatment.
Conclusion
With respect to the results of this study, it can be concluded that the use of TENS and LLLT is effective in TMD patients; so, they can be used as adjuvant therapy. In the present study, TENS caused a more rapid and long-lasting pain reduction. Longer administration of LLLT may be more effective in pain control, particularly during the follow-up period.
Acknowledgement
The authors would like to thank the Vice-chancellery of Shiraz University of Medical Sciences for supporting this research (Grant# 93-01-03-8636). This article is based on the thesis by Khadijeh Hajian from Shiraz School of Dentistry. The authors would also like to express gratitude to Dr. Vossoughi from Dental Research Development Center at Shiraz School of Dentistry for the statistical analysis.
Conflict of Interest:The authors of this manuscript certify no financial or other competing interest regarding this article.
References
- 1.Marini I, Bartolucci ML, Bortolotti F, Innocenti G, Gatto MR, Alessandri Bonetti G. The effect of diode superpulsed low-level laser therapy on experimental orthodontic pain caused by elastomeric separators: a randomized controlled clinical trial. Lasers Med Sci. 2015; 30: 35–41. doi: 10.1007/s10103-013-1345-y. [DOI] [PubMed] [Google Scholar]
- 2.de Godoy CH, Silva PF, de Araujo DS, Motta LJ, Biasotto-Gonzalez DA, Politti F, et al. Evaluation of effect of low-level laser therapy on adolescents with temporomandibular disorder: study protocol for a randomized controlled trial. Trials. 2013; 14: 229. doi: 10.1186/1745-6215-14-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu ZJ, Yamagata K, Kasahara Y, Ito G. Electromyographic examination of jaw muscles in relation to symptoms and occlusion of patients with temporomandibular joint disorders. J Oral Rehabil. 1999; 26: 33–47. doi: 10.1046/j.1365-2842.1999.00356.x. [DOI] [PubMed] [Google Scholar]
- 4.Frare J, Nicolau R. Análise clínica do efeito da fotobiomodulação laser (GaAs–904 nm) sobre a disfunção temporomandibular. Rev Bras Fisioter. 2008; 12: 37–42. [Google Scholar]
- 5.Okeson JP. Management of temporomandibular disorders and occlusion. 7th ed. Elsevier: Brazil; 2013. pp. 103–110. [Google Scholar]
- 6.de Godoy CH, Silva PF, de Araujo DS, Motta LJ, Biasotto-Gonzalez DA, Politti F, et al. Evaluation of effect of low-level laser therapy on adolescents with temporomandibular disorder: study protocol for a randomized controlled trial. Trials. 2013; 14: 229. doi: 10.1186/1745-6215-14-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Venancio Rde A, Camparis CM, Lizarelli Rde F. Low intensity laser therapy in the treatment of temporomandibular disorders: a double-blind study. J Oral Rehabil. 2005; 32: 800–807. doi: 10.1111/j.1365-2842.2005.01516.x. [DOI] [PubMed] [Google Scholar]
- 8.Emshoff R, Bösch R, Pümpel E, Schöning H, Strobl H. Low-level laser therapy for treatment of temporomandibular jointpain: a double-blind and placebo-controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105: 452–456. doi: 10.1016/j.tripleo.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Carvalho CM, de Lacerda, JA dos, Santos Neto, FP Cangussu, MC Marques, AM Pinheiro. Wave-length effect in temporomandibular joint pain: a clinical experience. Lasers Med Sci. 2010; 25: 229–232. doi: 10.1007/s10103-009-0695-y. [DOI] [PubMed] [Google Scholar]
- 10.Lee EW, Chung IW, Lee JY, Lam PW, Chin RK. The role of transcutaneous electrical nerve stimulation in management of labour in obstetric patients. Asia Oceania J Obstet Gynaecol. 1990; 16: 247–254. doi: 10.1111/j.1447-0756.1990.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 11.Mello LF, Nóbrega LF, Lemos A. Transcutaneous electrical stimulation for pain relief during labor: a systematic review and meta-analysis. Rev Bras Fisioter. 2011; 15: 175–184. [PubMed] [Google Scholar]
- 12.Orange FAd, Amorim MMRd, Lima L. Uso da eletroes-timulação transcutânea para alívio da dor durante o tra-balho de parto em uma maternidade-escola: ensaio clínico controlado. RBGO. 2003; 25: 45–52. [Google Scholar]
- 13.Wisneski LA, Anderson L. The scientific basis of integrative medicine. 2nd ed. CRCpress: USA: CRCpress: USA; 2009. pp. 308–312. [Google Scholar]
- 14.Eghbali F. Applying low level laser therapy in dentistry. 1st ed. Shayannemoodar: Iran; 2009. pp. 60–64. [Google Scholar]
- 15.Cetiner S, Kahraman SA, Yücetaş S. Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg. 2006; 24: 637–641. doi: 10.1089/pho.2006.24.637. [DOI] [PubMed] [Google Scholar]
- 16.Shirani AM, Gutknecht N, Taghizadeh M, Mir M. Low-level laser therapy and myofacial pain dysfunction syndrome: a randomized controlled clinical trial. Lasers Med Sci. 2009; 24: 715–720. doi: 10.1007/s10103-008-0624-5. [DOI] [PubMed] [Google Scholar]
- 17.Carrasco TG, Mazzetto MO, Mazzetto RG, Mestriner W Jr. Low intensity laser therapy in temporomandibular disorder: a phase II double-blind study. Cranio. 2008; 26: 274–281. doi: 10.1179/crn.2008.037. [DOI] [PubMed] [Google Scholar]
- 18.Shanavas M, Chatra L, Shenai P, Rao PK, Jagathish V, Kumar SP, et al. Transcutaneous electrical nerve stimulation therapy: An adjuvant pain control-ling modality in TMD patients- A clinical study. Dent Res J (Isfahan) 2014; 11: 676–679. [PMC free article] [PubMed] [Google Scholar]
- 19.Núñez SC, Garcez AS, Suzuki SS, Ribeiro MS. Management of mouth opening in patients with temporomandibular disorders through low-level laser therapy and transcutaneous electrical neural stimulation. Photomed Laser Surg. 2006; 24: 45–49. doi: 10.1089/pho.2006.24.45. [DOI] [PubMed] [Google Scholar]
- 20.Kato MT, Kogawa EM, Santos CN, Conti PC. TENS and low-level laser therapy in the management of temporomandibular disorders. J Appl Oral Sci. 2006; 14: 130–135. doi: 10.1590/S1678-77572006000200012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharma R. Pterygoid disjunction for internal derangement of temporomandibular joint. J Maxillofac Oral Surg. 2011; 10: 142–147. doi: 10.1007/s12663-011-0202-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helkimo M. Studies on function and dysfunction of the masticatory system. I. An epidemiological investigation of symptoms of dysfunction in Lapps in the north of Finland. Proc Finn Dent Soc. 1974; 70: 37–49. [PubMed] [Google Scholar]
- 23.Singh H, Sunil MK, Kumar R, Singla N, Dua N, Garud SR. Evaluation of TENS therapy and Placebo drug therapy in the management of TMJ pain disorders: A comparative study. J Indian Acad Oral Med Radiol. 2014; 26: 139–144. [Google Scholar]
- 24.Ganapathi M, Shashikanth MC, Sunil MK, Shambulin-gappa P. Transcutaneous Electrical Nerve Stimulation Therapy in Temporomandibular Disorder: A Clinical Study. Journal of Indian Academy of Oral Medicine and Radiology. 2011; 23: 46–50. [Google Scholar]
- 25.Linde C, Isacsson G, Jonsson BG. Outcome of 6-week treatment with transcutaneous electric nerve stimulation compared with splint on symptomatic temporomandibular joint disk displacement without reduction. Acta Odontol Scand. 1995; 53: 92–98. doi: 10.3109/00016359509005953. [DOI] [PubMed] [Google Scholar]
- 26.Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003; 49: 107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 27.Fikácková H, Dostálová T, Navrátil L, Klaschka J. Effectiveness of low-level laser therapy in temporomandibular joint disorders: a placebo-controlled study. Photomed Laser Surg. 2007; 25: 297–303. doi: 10.1089/pho.2007.2053. [DOI] [PubMed] [Google Scholar]
- 28.Kulekcioglu S, Sivrioglu K, Ozcan O, Parlak M. Effectiveness of low-level laser therapy in temporomandibular disorder. Scand J Rheumatol. 2003; 32: 114–118. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 29.Isacsson G, Linde C, Isberg A. Subjective symptoms in patients with temporomandibular joint disk displacement versus patients with myogenic craniomandibular disorders. J Prosthet Dent. 1989; 61: 70–77. doi: 10.1016/0022-3913(89)90112-1. [DOI] [PubMed] [Google Scholar]
- 30.Jensen R, Rasmussen BK, Pedersen B, Lous I, Olesen J. Prevalence of oromandibular dysfunction in a general population. J Orofac Pain. 1993; 7: 175–182. [PubMed] [Google Scholar]
- 31.de Medeiros JS, Vieira GF, Nishimura PY. Laser application effects on the bite strength of the masseter muscle, as an orofacial pain treatment. Photomed Laser Surg. 2005; 23: 373–376. doi: 10.1089/pho.2005.23.373. [DOI] [PubMed] [Google Scholar]


