Abstract
Purpose
The natural history of pleomorphic lobular carcinoma in situ (PLCIS) remains largely unknown.
Methods
A pathology database search (1995–2012) was performed to identify patients diagnosed with an LCIS variant. Patients with synchronous breast cancer and/or no evidence of pleomorphism were excluded. Original slides were re-evaluated by 3 pathologists to identify a consensus cohort of PLCIS. Borderline lesions with focal atypia were classified as LCIS with pleomorphic features (LCIS-PF). Clinical data were obtained from medical records.
Results
From 233 patients, we identified 32 with an LCIS variant diagnosis and no concurrent breast cancer. Following review, 16 cases were excluded due to lack of pleomorphism. The remaining 16 were classified as PLCIS (n=11) and LCIS-PF (n=5). 12/16 patients were treated with surgical excision +/− chemoprevention. Patients with a prior breast cancer history and those having mastectomy were excluded from outcome analysis. Among the remaining 7 patients with PLCIS/LCIS-PF, 4/7 (57%) developed ipsilateral breast cancer at a median follow-up of 67 months. Median age at the time of breast cancer diagnosis was 56 years old and median time from PLCIS/LCIS-PF to cancer diagnosis was 59 months (range, 45–66 months). The 4 cancers included 1 invasive lobular carcinoma (ILC), 1 microinvasive ILC, 1 invasive ductal carcinoma and 1 ductal carcinoma in situ.
Conclusions
We confirm that PLCIS in isolation is indeed a rare entity, further contributing to the difficulty in determining the actual risk conferred by this lesion. Long-term follow-up data on larger cohorts is needed to define standardized management and outcomes for patients with PLCIS.
Keywords: lobular carcinoma in situ, pleomorphic lobular carcinoma in situ, high risk lesion, breast cancer, recurrence
INTRODUCTION
Pleomorphic lobular carcinoma in situ (PLCIS) is a recently described morphologic variant of lobular carcinoma in situ (LCIS). It was first identified as a distinct entity by Eusebi et al in 1992[1]. Early studies primarily reported cases of PLCIS associated with invasive lobular carcinoma[2–4], but recent series have described the morphologic spectrum of PLCIS not associated with invasive breast cancer[5–9].
Histologically, PLCIS exhibits an architectural pattern similar to classic LCIS (LCIS-C), though there is usually marked acinar expansion in PLCIS as well as large, strikingly pleomorphic cells with an eosinophilic cytoplasm and a high nuclear grade. Comedo necrosis and calcifications are common in PLCIS with the solid growth pattern and high grade atypia. In some cases it is difficult to distinguish PLCIS from solid, high-grade ductal carcinoma in situ (DCIS) without the use of immunohistochemical stains, and, historically, many clinicians have recommended a more aggressive treatment than for classic LCIS[1,5,6,9]. As the name implies, the cells of pleomorphic apocrine LCIS—a subtype of PLCIS according to the WHO classification[10]—also have high grade nuclear atypia, but are characterized by abundant granular eosinophilic “apocrine” cytoplasm and prominent, central nucleoli[1,5,6,9].
In its pure form, PLCIS can also be difficult to distinguish from other LCIS variants. “Florid” LCIS/LCIS with comedo necrosis is composed of cells with the cytomorphology of classic LCIS (with type A or type B cells), but shows massively expanded acini with central necrosis of comedo type and calcifications[6,10]. In the past, some publications have also used the generic term of carcinoma in situ with mixed ductal and lobular features[10]. This is in part due to the variety of diagnostic criteria that have been used in prior reports, leading to significant inter-observer variability and poor diagnostic agreement between pathologists[11]. These challenges combined with the rarity of these lesions, have resulted in a lack of information on the natural history of PLCIS and consequently, no standardized treatment has been established.
Both classic LCIS and LCIS variants including PLCIS typically lack membrane E-cadherin and show diffuse cytoplasmic distribution of p120 catenin, a molecule of the E-cadherin–catenin cell adhesion complex[4,5,9,12–14]. Also, cells of PLCIS generally express estrogen receptor (ER), though some cases show a weaker expression than classic LCIS and some are ER negative, especially PLCIS with apocrine features[13,14]. Furthermore, PLCIS usually has a moderate to high proliferative rate, and may demonstrate HER2 protein overexpression and p53 positivity[13,14]. Molecular genetic data on PLCIS are limited. Even though PLCIS bares the distinctive molecular genetic changes of classic LCIS (gain of 1q and deletion of 16q along with E-cadherin inactivation), this variant may also show HER2 gene amplification, amplification of cyclin D1 gene, gain of 20q, loss of 17p and 13q[13,14].
Even though the histologic features, biomarker profile, and genomic instability demonstrated in PLCIS suggest a more aggressive phenotype than classic LCIS[12–14], clinical follow-up studies are needed to define the natural history, risk of subsequent invasive carcinoma, and most appropriate management of these lesions. We conducted a centralized pathology review at a single institution to identify and study cases of pure PLCIS. Herein, we examine the clinical, radiologic and histologic findings associated with PLCIS and report long-term clinical outcomes for patients treated with conservative surgery.
MATERIALS AND METHODS
Database search of surgical pathology reports in the Department of Pathology at Memorial Sloan-Kettering Cancer Center (MSKCC) from 1995 to 2012 was performed to identify surgical excision specimens with a final diagnosis of an LCIS variant or classic LCIS with any mention of atypia. To account for the different terms used over time to describe the morphologic variants of LCIS, the terms used for our search included PLCIS, apocrine PLCIS, LCIS with necrosis, large cells LCIS, florid LCIS, and also “carcinoma in situ with mixed ductal and lobular features”. We excluded from the study cases with synchronous DCIS or invasive breast cancer, either ipsilateral or contralateral. Cases with a previous history of DCIS or invasive breast cancer (at least 12 months prior to LCIS variant diagnosis) were included for descriptive purposes, but were not included in the outcomes analysis. All original H&E slides from the core biopsy and/or surgical excision specimens were re-evaluated without knowledge of the primary diagnosis by 3 pathologists (MDB, MM, DG) to identify a consensus cohort of pleomorphic LCIS. We excluded from the study cases for which only core biopsy slides were available for review. All patients had their surgical excision performed at MSKCC, except for one who had an initial excision done elsewhere and subsequently underwent re-excision and ultimately mastectomy at MSKCC. This study was approved by the Institutional Review Board of MSKCC, New York, NY.
Findings required for the diagnosis of PLCIS included acinar expansion and cellular dyshesion, increased nuclear size (>3–4x the size of a lymphocyte), moderate to marked nuclear pleomorphism (>2–3x variation in nuclear size), and loss of membranous E-cadherin by immunohistochemical staining[2,4,5,7]. Findings that were frequently associated with PLCIS but were not required for the diagnosis included: presence of comedo necrosis and calcifications, apocrine features, intracytoplasmic vacuoles, mitotic activity, nuclei eccentrically placed, nuclear membrane irregularity, conspicuous or prominent nucleoli, granular pattern of the chromatin, and apoptosis. We defined borderline lesions with focal atypia (i.e., only a few lobular units with atypical pleomorphic cells in a background of classic LCIS) that fulfilled some but not all of the required criteria for the diagnosis of PLCIS as LCIS with pleomorphic features (LCIS-PF).
Margin status was classified as positive (PLCIS cells at the inked margin, with or without obvious truncation of the lesion), negative (no PLCIS cells at the inked margin) or close (PLCIS present ≤1 mm from the inked margin).
For cases in which E-cadherin immunohistochemical staining had not been performed at the time of the original diagnosis, or the E-cadherin stained slide was not available, we retrieved the formalin-fixed paraffin-embedded archival tissue blocks and we performed immunohistochemistry (IHC) for E-cadherin, as well as ER and HER2 as previously described (Supplementary Table 1)[15,16].
Electronic medical records were reviewed for data collection including patient demographics, breast cancer risk factors, radiographic and pathologic findings, and treatment variables. The time to recurrence of PLCIS or new breast cancer events were defined from the date of the initial diagnosis of the LCIS variant. Differences in demographic and clinical variables by consensus pathology diagnosis were tested using the Pearson chi-square test, the t test or the Mann-Whitney test, as appropriate.
RESULTS
Patient Population
Our database quest over a period of 17 years identified 233 patients who underwent a breast surgical excision and received a final diagnosis of a variant of LCIS. Most patients (201/233; 86.3%) had synchronous invasive cancer or DCIS (either ipsilateral or contralateral) and were excluded from the study. We also excluded 11/233 (4.7%) patients with an outside pathology report describing a LCIS variant that was subsequently reviewed at MSKCC and classified as LCIS-C.
Thus the cohort selected for consensus pathology review included 21/233 (9.1%) patients diagnosed with a LCIS variant (Supplementary Figure 1). Following consensus pathology review, we excluded 5 (23.8%) patients because the surgical excision slides failed to show nuclear pleomorphism. The consensus review of the material from the remaining 16 patients resulted in 11 (68.8%) cases classified as pure PLCIS (including 2 apocrine PLCIS) and 5 (31.2%) cases classified as LCIS-PF.
The breakdown of the study consensus pathology diagnosis is illustrated in Figure 1; the original diagnosis and the pathology review classification are shown in Table 1.
Figure 1. Final diagnosis following consensus pathology review.
Cases for which the slides of the surgical excision failed to show nuclear pleomorphism in the lobular carcinoma in situ lesion and were thus categorized as classic lobular carcinoma in situ after pathology consensus review (A: H&E staining, 200x magnification); cases with the consensus pathology diagnosis of lobular carcinoma in situ with pleomorphic features (B: H&E staining, 200x magnification) and pleomorphic lobular carcinoma in situ (C: H&E staining, 200x magnification)
Table 1.
Original diagnosis and pathology review classification
| Original Diagnosis | Review Diagnosis | |
|---|---|---|
| PLCIS | LCIS-PF | |
| PLCIS N=6 |
5 | 1 |
| LCIS-PF N=5 |
1 | 4 |
| Large Cells LCIS N=1 |
1 | 0 |
| Florid LCIS N=1 |
1 | 0 |
| Carcinoma in situ with mixed ductal and lobular features N=3 |
3 | 0 |
|
Total N=16 |
11 (68.8%) | 5 (31.2%) |
Abbreviations: PLCIS, pleomorphic lobular carcinoma in situ; LCIS-PF; lobular carcinoma in situ with lobular features
Characteristics and Treatment of Patients Diagnosed with Pure PLCIS/LCIS-PF
The mean age at diagnosis of PLCIS/LCIS-PF was 55 years (yrs) (range 42–67). Patients with consensus diagnosis of PLCIS were older than those with LCIS-PF, (mean of 57yrs vs 49yrs; p=0.01). All cases presented with imaging abnormalities either on mammography or magnetic resonance imaging; suspicious or indeterminate calcifications were the most common presentation (9/16 cases; 56.3%).
In all, 5/16 (31.3%) patients had a previous history of breast cancer, either ipsilateral (1/5; 20.0%) or contralateral 4/5 (80%) to the LCIS variant. Prior breast cancers included DCIS (2/5; 40%), invasive ductal carcinoma (IDC) (2/5; 40%) and an invasive mammary carcinoma with mixed lobular and ductal features (1/5; 20%). The median time from prior cancer diagnosis to index LCIS variant diagnosis was 63 months (range, 10–76).
Following the PLCIS/LCIS-PF diagnosis, 4/16 (25%) patients underwent mastectomy. The remaining 12/16 (75%) patients had surgical excision alone, with (n=3) or without chemoprevention (n=9). Chemoprevention (CP) consisted of tamoxifen or raloxifene use for at least 6 months after diagnosis. None of the patients was offered radiation therapy at the time of original LCIS variant diagnosis. Two of the 4 patients who underwent mastectomy had originally been diagnosed with carcinoma in situ with mixed ductal and lobular features. The other two patients underwent bilateral prophylactic mastectomy for PLCIS and classic LCIS after one or more attempts at excision. None of these 4 patients had a previous history of breast cancer.
Among patients treated with local excision, 5/12 (41.7%) had positive final surgical margins (defined as PLCIS/LCIS-PF present at ink), 3/12 (25.0%) had close final margins (defined as PLCIS/LCIS-PF ≤ 1 mm from ink), and 4/12 (33.3%) had negative final margins (clearance >1 mm).
The mean and median follow-up time was 86 months (mos) and 68 months, respectively (range 34,189).
Clinical findings, type of surgery, and margin status are summarized in Table 2[16].
Table 2.
Characteristics of patients diagnosed with pure PLCIS/LCIS-PF and LCIS variant immunohistochemical profile
| Final Diagnosis | Total N=16 |
||
|---|---|---|---|
|
| |||
| PLCIS N=11 |
LCIS-PF N=5 |
||
| Imaging Presentation | |||
| Calcifications (MMG) | 7 | 2 | 9 (56.3%) |
| Enhancement (MRI) | 3 | 2 | 5 (31.2%) |
| Others (MMG or MRI) | 1 | 1 | 2 (12.5%) |
|
| |||
| Previous Breast Cancer | |||
| Yes | 3 | 2 | 5 (31.2%) |
| No | 8 | 3 | 11 (68.8%) |
|
| |||
| Type of Surgery | |||
| Excision | 8 | 4 | 12 (75%) |
| Mastectomy | 3 | 1 | 4 (25%) |
|
| |||
| Margins at Excision (N=12) | |||
| Positive | 2 | 3 | 5 (31.3%) |
| Negative | 3 | 1 | 4 (25%) |
| Close | 3 | 0 | 3 (18.7%) |
|
| |||
| Immunohistochemical Profile | |||
| E-Cadherin | Negative: 11 | Negative: 5 | Negative: 16 (100%) |
| Positive: 0 | Positive: 0 | Positive: 0 | |
|
|
|||
| Estrogen Receptor* | Negative: 2 | Negative: 0 | Negative: 2 (12.5%) |
| Positive: 9 | Positive: 5 | Positive: 14 (87.5%) | |
|
|
|||
| HER2** | Negative | Negative | Negative: 15 (93.7%) |
| Score 0: 0 | Score 0: 3 | ||
| Score 1+: 10 | Score 1+: 2 | ||
|
| |||
| Equivocal | Equivocal | Equivocal: 1 (6.3%) | |
| Score 2+: 1 | Score 2+: 0 | ||
|
| |||
| Positive | Positive | Positive: 0 | |
| Score 3+: 0 | Score 3+: 0 | ||
PLCIS, pleomorphic lobular carcinoma in situ; LCIS-PF; lobular carcinoma in situ with lobular features; MMG, mammography; MRI, magnetic resonance imaging; HER2, human epidermal growth factor receptor.
Estrogen receptor was regarded as positive if ≥1% of LCIS cells demonstrate positive nuclear staining by immunohistochemistry;
HER2/neu was scored on a 0 to 3+ scale using ASCO/CAP test guideline recommendations. (16). FISH for HER2 was not performed for the equivocal case.
Morphologic features of PLCIS/ LCIS-PF
The size of PLCIS/LCIS-PF as assessed by the largest microscopic focus in one slide ranged from 0.8 to 9.0 mm. Comedo type necrosis was identified in 6/16 (37.5%) cases. LCIS with classic morphology and comedo necrosis was present in 3/16 (18.8%) cases. (Figure 2). Classic LCIS coexisted with PLCIS/LCIS-PF in all cases. Microcalcifications were associated with PLCIS/LCIS-PF in all cases. In addition, 7/16 (43.8%) cases had microcalcifications in other lesions, including classic LCIS (4/16; 25%) and columnar cell change (1/16; 6.3%), or within normal mammary acini (2/16; 12.5%).
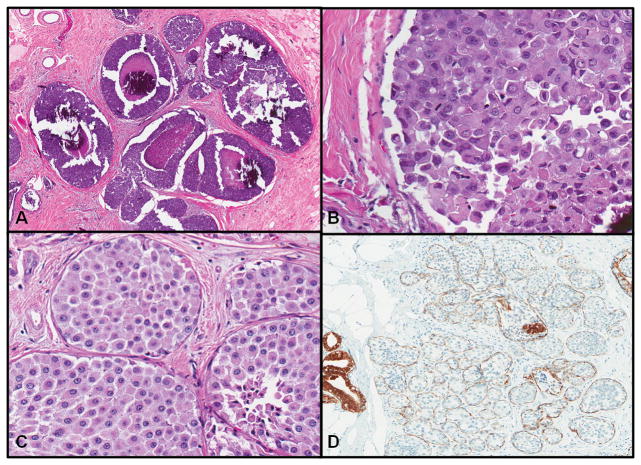
Figure 2. Pathologic and immunophenotypic findings associated with PLCIS.
Presence of acinar distension and comedo necrosis (A: H&E staining, 50x magnification), cellular dyshesion and marked nuclear pleomorphism (B: H&E staining, 200x magnification), apocrine differentiation (C: H&E staining, 200x magnification) and loss of E-cadherin (D: H&E staining, 100x magnification)
Complete membranous E-cadherin loss consistent with a lobular phenotype was documented in all PLCIS/LCIS-PF cases and there were no cases of aberrant E-cadherin expression (granular staining). Expression of ER was identified in 14/16 (87.5%) PLCIS/LCIS-PF cases and only 2/14 cases had low positive ER expression (nuclear staining in 1–10% of lesion cells). Most (15/16; 93.8%) had no HER2 overexpression by immunohistochemical staining (0 staining in 3 cases, 1+ staining in 12). One case was considered to be equivocal (score 2+); HER2 fluorescence in situ hybridization (FISH) was not performed (Table 2).
PLCIS/ LCIS-PF and Multicentricity
Classic LCIS is known for its multicentric and bilateral distribution, but information about the distribution of variants of LCIS is almost nonexistent. We sought to examine PLCIS distribution in mastectomy specimens available in our series. Of the 4 patients who underwent mastectomy at the time or immediately after the index diagnosis, 3 (75%) had several foci of PLCIS/LCIS-PF distributed in different quadrants of the breast (multicentric PLCIS/ LCIS-PF), whereas one patient had several foci of PLCIS in the same quadrant (multifocal). Two of the 4 aforementioned patients underwent bilateral mastectomies; classic LCIS was present in both breasts, whereas the PLCIS lesions were unilateral.
High-risk breast lesions histologically associated with PLCIS/LCIS-PF included atypical ductal hyperplasia (ADH, 2/16; 12.5%) and columnar cell lesions with atypia/flat epithelial atypia (FEA, 5/16; 31.3%). Other benign breast lesions were ductal hyperplasia of the usual type (3/16; 18.8%); radial scar (2/16; 12.5%); sclerosing adenosis (5/16; 31.3%); and columnar cell change without atypia (5/16; 31.3%).
New Events in Patients with Pure PLCIS/LCIS-PF
After we excluded 5 patients with a prior history of either ipsilateral or contralateral breast cancer (DCIS or invasive carcinoma), our outcome cohort consists of 11 patients with PLCIS/LCIS-PF and a median follow-up time of 67 mos, mean, 89 mos (range, 34–189 mos). Four (4/11, 36%) patients underwent mastectomy at the time of or shortly after the index diagnosis of PLCIS/LCIS-PF diagnosis. All 4 patients were clinically free of disease at the time of last follow-up.
Seven patients underwent breast surgical excision (+/− CP). Four of the 7 patients (57%) developed breast cancer (either DCIS or invasive carcinoma) ipsilateral to the PLCIS. Their median age at the time of breast cancer diagnosis was 56 years old (range, 46 –67). The median time from PLCIS/LCIS-PF to cancer diagnosis was 59 mos (range, 45–66mos). The 4 cancers included 1ILC, 1 microinvasive ILC, 1 IDC and 1 DCIS. None of the patients who developed carcinoma had a previous history of atypical epithelial lesions (ALH, ADH, FEA). In 2/4 patients (#P26 and #P224) the cancers developed in the same quadrant of the breast as the prior PLCIS lesion, which had been excised with close (<1mm) margins. In the remaining 2 patients, the margins of the index lesion in the original surgical excision specimen were positive (1 case) or close (1 case). At the time of surgery for cancer, PLCIS was histologically identified in the surgical specimen from all three patients with invasive carcinoma, while the patient with DCIS also harbored in situ carcinoma with mixed lobular and ductal features. The remaining 3 patients treated with excision did not take CP and 2/3 had their PLCIS/LCIS-PF removed with negative margins; all remain free of disease at a median follow-up of 50 mos after the diagnosis.
A summary of these findings is shown in Table 3.
Table 3.
Characteristics and outcomes of patients with pure PLCIS/LCIS-PF treated with conservative surgery
| Case # N=7 |
Original Diagnosis | Review Diagnosis | ER/HER2 Status | Treatment at Time of LCIS Variant | Margins at Excision Specimen | Ipsilateral Breast Cancer | Size, Grade and Type of the Breast Cancer | Time to Event or Length of Follow-Up (months) |
|---|---|---|---|---|---|---|---|---|
| P-026 | Large Cells LCIS | PLCIS | ER+ HER2: 1+ |
Excision + CP | Close (<1mm) | DCIS | 0.2 cm; Intermediate grade; Solid and cribriform pattern | 66 |
| P-190 | PLCIS | LCIS-PF | ER+ HER2: 1+ |
Excision only | Positive | ILC classic | Multifocal lesion (1mm to 1.5cm); Grade 3; 0/5 SLNs | 45 |
| P-197 | PLCIS | PLCIS | ER+ HER2: 1+ |
Excision only | Close (<1mm) | Microinvasive ILC | One focus < 1mm (detected on MR guided biopsy); Grade not reported; 0/4 SLNs | 63 |
| P-224 | Carcinoma in situ mixed features | PLCIS | ER+ HER2: 1+ |
Excision only | Close (<1mm) | IDC | 0.9 cm; Grade 3; 0/1 SLN | 56 |
| P-209 | Apocrine PLCIS | Apocrine PLCIS | ER+ HER2: 1+ |
Excision only | Negative | N/A | N/A | 60 |
| P-301 | LCIS-PF | LCIS-PF | ER+ HER2: 1+ |
Excision only | Negative | N/A | N/A | 50 |
| P-303 | PLCIS | PLCIS | ER+ HER2: 1+ |
Excision only | Positive | N/A | N/A | 42 |
Abbreviations: ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; PLCIS, pleomorphic lobular carcinoma in situ; LCIS-PF; lobular carcinoma in situ with lobular features; DCIS, ductal carcinoma in situ; ILC, invasive lobular carcinoma; CP, chemoprevention; N/A, not applicable; SLN, sentinel lymph node
DISCUSSION
In this study, we conducted a comprehensive search through archived pathology reports, slides, and tissue specimens to identify cases of PLCIS and study its natural history. Pure PLCIS not associated with a concurrent breast cancer (DCIS or invasive carcinoma) was confirmed by pathology review in only 16/233 (6.9%) cases of LCIS variants documented over a 17-year period at our institution, underscoring the rarity of this lesion. Furthermore, only 11 of the lesions met all the morphologic criteria for the diagnosis of PLCIS. The rarity of this lesion combined with the lack of standardized criteria used for the diagnosis creates significant challenges when attempting to study the natural history of PLCIS (Table 4)[5,17,7,8]. In addition, we demonstrated that synchronous DCIS/invasive breast carcinoma or prior history of breast cancer is often present in patients with PLCIS, further contributing to the difficulty in determining the actual risk conferred by this lesion and its appropriate management.
Table 4.
Natural history of PLCIS in distinct studies that included patients treated with breast conserving surgery
| PLCIS Series | Patients With PLCIS Treated With Excision | Follow-Up Time | Recurrent PLCIS | Ipsilateral DCIS or IBC | CBC |
|---|---|---|---|---|---|
| Sneige et al, 2002 (5) | 5 excision | 17 mos (mean) | 1 (12 mos) | - | - |
| Downs-Kelly 2011 (17) | 10 excision 6 excision + CP |
46 mos (mean) | 1 (19 mos) | - | - |
| Khoury et al, 2014 (7) | 17 excision 11 excision + CP 3 excision + RT |
55.5 mos (median) | 2 | 4 (3 ILC, 1 IDC) | - |
| Flanagan et al, 2015 (8) | 7 excision (+/−CP, +/−RT) | 4.1 yrs (mean) | - | - | - |
| De Brot et al, 2017 | 6 excision 1 excision + CP |
67 mos (median) | 3 (56 mos) | 4 (1 DCIS, 2 ILC, 1 IDC) | - |
Abbreviations: PLCIS, pleomorphic lobular carcinoma in situ; DCIS, ductal carcinoma in situ; IBC, invasive breast cancer; ILC, invasive lobular carcinoma; IDC, invasive ductal carcinoma; CP, chemoprevention; RT, radiotherapy; CBC, contralateral breast cancer; mos, months; yrs, years.
Even though PLCIS is characterized by several distinct morphologic features, there remains considerable variation in the histologic criteria used for the diagnosis of different variants of LCIS. We created a uniform method to identify cases of PLCIS using a consensus between 3 breast pathologists with standardized written criteria to define features of PLCIS. Using these standardized criteria, we were able to come to an agreement on 16 cases of PLCIS or LCIS-PF and re-categorize 5 lesions of PLCIS that were originally described as other variants of LCIS, including 3 lesions that were initially described as carcinoma in situ with mixed ductal and lobular features. Sullivan and colleagues[18] have also documented this re-categorization of lesions to PLCIS after a consensus review and E-cadherin staining, where among 75 cases of solid DCIS, 10 (13.3%) were reclassified as LCIS, including 9 variants (5 PLCIS, 4 LCIS with necrosis) and 1 classic LCIS. As distinct variants of LCIS have been recognized over the last years, separating LCIS variants from DCIS has increasingly become a concern because of implications for patient treatment with regard to margin status and radiation therapy. Furthermore, if strict criteria to diagnose PLCIS are not uniformly applied, we will likely continue to see cases of PLCIS being misclassified and its natural history will remain ill defined.
Consistent with previous reports, we also found that PLCIS typically presents as an imaging abnormality. The association of calcifications with LCIS variants, in particular PLCIS, has been previously described[5,7,12,19]. The rate of upgrade to carcinoma (invasive or DCIS) following the identification of PLCIS in a needle core biopsy specimen, ranges from 25% to 60% supporting routine excision of these lesions[18,17,20–22]. Flanagan and colleagues[8] reported that among 21 patients with pure PLCIS in a needle core biopsy, 33.3% had invasive carcinoma and 19% had DCIS at surgical excision. In our series we excluded 201/233 pts with a synchronous invasive cancer or DCIS (either ipsilateral or contralateral); the majority of whom (particularly in the later years of our study) also presented with a core biopsy diagnosis of an LCIS variant and were found to have cancer at surgical excision.
When DCIS or invasive breast carcinoma is not identified at surgical excision, there is a paucity of data addressing the need to obtain clear margins for PLCIS or LCIS variant lesions. Downs-Kelly et al[17] retrospectively investigated the influence of margin status on recurrence in 26 patients with PLCIS treated with conservative surgery at M.D. Anderson Cancer Center. In 6 of these cases there was also evidence of microinvasion or T1a cancer and these patients also received radiation therapy. In addition, 6 pts received chemoprevention. At a median follow-up of 33 mos they reported one case of recurrent PLCIS in a patient who was initially excised with positive margins. There were no subsequent cancers reported in this series.
In our series, at a median follow-up of 67 months, 4 of 7 patients with PLCIS/LCIS-PF and no prior history of ipsilateral or contralateral breast cancer treated with local excision developed breast cancer. All of the cancers were ipsilateral to the index PLCIS, which had been excised with either positive or close margins. PLCIS was also histologically identified in all but one patient. Interestingly, in 2/4 patients, the subsequent malignant lesion was found in the same quadrant of the breast as the previously diagnosed PLCIS and the original lesion had been excised with close margins. In the 3 patients treated with conservation who remain cancer free, 2 had their PLCIS removed with negative margins. Although admittedly we are reporting on a small number of cases, our findings continue to support the pragmatic recommendation that whenever possible an effort should be made to achieve negative margins.
Given the increased genomic instability reported for PLCIS[13], there is much speculation that the risk of subsequent breast cancer is higher than that conferred by a diagnosis of classic LCIS. In a recent publication from our group including 1,032 patients who chose surveillance after a diagnosis of LCIS-C, 150 patients developed 168 breast cancers at a median follow-up of 81 months, with an overall cumulative cancer incidence of 26% at 15 years[23]. In this study our outcome cohort includes only 7 patients with PLCIS/LCIS-PF treated with conservative surgery; of whom 4 (57%) developed breast cancer at a median follow-up of 67 months. The large disparity in the size of our pure PLCIS series as compared to our cohort of patients with classic LCIS makes it difficult to draw any definitive conclusions regarding the relative risk imparted by a diagnosis of PLCIS as compared to classic LCIS; and highlights the need for further work in this area.
When compared to other series of PLCIS, our rate of cancer development is noticeably higher than that reported by Khoury et al[7], which included 47 PLCIS cases collected from 3 different institutions over a 12-year period. After excluding 16 cases with concurrent or past history of breast cancer, the authors found that 4/31 (13%) remaining patients developed breast cancer and 2/31 (6%) recurred with PLCIS at a median follow-up of 55.6 months[7]. The differences in subsequent cancer events between our study and that of Khoury et al may be partially explained by the different methods of case ascertainment in the two studies. Our search started with all LCIS variants from a single institution and ultimately yielded 16/233 (6.9%) cases satisfying the pre-defined criteria for pure PLCIS or LCIS-PF. In contrast, the study by Khoury et al collected cases from 3 institutions with slightly different methodology: at one institution all PLCIS, C-LCIS and solid type DCIS cases were reviewed yielding 14/321 (4.4%) cases of PLCIS; whereas at the other two institutions cases of LCIS or any lobular neoplasia were reviewed yielding 4 and 29 cases respectively (denominator of cases reviewed is not reported) for a total of 47 cases. Notably in both series the number of patients available for the at risk analyses were smaller due to the frequent history of prior breast cancer in these populations. Finally, the study conducted by Flanagan et al reported no new ipsilateral breast cancer events in 7 patients with pure PLCIS who had been treated with excision (+/− CP or radiation) during a mean follow-up period of 4.1 years, including 4 patients with positive or close margins at definitive surgery[8]. The small numbers and limited treatment information in this series make it difficult to draw any conclusions about the impact of radiation.
Although all available studies are limited by their retrospective nature, various selection criteria and lack of uniform treatment standards, it is notable that rates of subsequent cancer appear to fall within a wide range with three available studies reporting no subsequent cancers and only our study and that of Khoury et al reporting subsequent malignancies after relatively long term follow-up (Table 4). In addition, although PLCIS is reported to demonstrate a weaker ER expression than LCIS-C, PLCIS cells are usually ER positive[4–7,12,13], a finding which we were able to replicate in our series where only 2/16 (12.5%) cases were negative for this marker. Such results point out that risk reduction with chemoprevention may still be a good option for patients diagnosed with PLCIS.
In conclusion, we confirm that PLCIS in isolation is indeed a rare lesion. In our series spanning over 17 years and with many different pathologists rendering the diagnosis over time, the term “pleomorphic” was sometimes inconsistently used. The natural history of PLCIS not associated with invasive carcinoma remains largely unknown. PLCIS almost always presents as an imaging abnormality and is typically found in association with classic LCIS. We recognize the limitations of our small cohort and the retrospective nature of this study; however our study is strengthened by our comprehensive search criteria and central pathology review which required a consensus diagnosis among 3 pathologists. We also report the longest follow-up time in the literature for patients treated with excision +/− chemoprevention. If we wish to move past anecdotal evidence and small retrospective cohort studies, ongoing discussion with pathologists to outline the diagnostic criteria of PLCIS, and long-term follow-up data on larger cohorts is needed to define standardized management and outcomes for patients with PLCIS.
Supplementary Material
Acknowledgments
Funding: This work was supported by the Susan G. Komen for the Cure Career Catalyst Award.
Footnotes
Compliance with Ethical Standards:
Conflict of Interest: The authors declare that they have no conflict of interests to declare.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Eusebi V, Magalhaes F, Azzopardi JG. Pleomorphic lobular carcinoma of the breast: an aggressive tumor showing apocrine differentiation. Hum Pathol. 1992;23:655–662. doi: 10.1016/0046-8177(92)90321-s. [DOI] [PubMed] [Google Scholar]
- 2.Bentz JS, Yassa N, Clayton F. Pleomorphic lobular carcinoma of the breast: clinicopathologic features of 12 cases. Mod Pathol. 1998;11:814–822. [PubMed] [Google Scholar]
- 3.Frost AR, Karcher DS, Terahata S, Siegel RS, Silverberg SG. DNA analysis and S-phase fraction determination by flow cytometric analysis of infiltrating lobular carcinoma of the breast. Mod Pathol. 1996;9:930–937. [PubMed] [Google Scholar]
- 4.Middleton LP, Palacios DM, Bryant BR, Krebs P, Otis CN, Merino MJ. Pleomorphic lobular carcinoma: morphology, immunohistochemistry, and molecular analysis. Am J Surg Pathol. 2000;24:1650–1656. doi: 10.1097/00000478-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Sneige N, Wang J, Baker BA, Krishnamurthy S, Middleton LP. Clinical, histopathologic, and biologic features of pleomorphic lobular (ductal-lobular) carcinoma in situ of the breast: a report of 24 cases. Mod Pathol. 2002;15:1044–1050. doi: 10.1097/01.MP.0000027624.08159.19. [DOI] [PubMed] [Google Scholar]
- 6.Fadare O, Dadmanesh F, Alvarado-Cabrero I, Snyder R, Stephen Mitchell J, Tot T, Wang SA, Ghofrani M, Eusebi V, Martel M, Tavassoli FA. Lobular intraepithelial neoplasia [lobular carcinoma in situ] with comedo-type necrosis: A clinicopathologic study of 18 cases. Am J Surg Pathol. 2006;30:1445–1453. doi: 10.1097/01.pas.0000213290.58283.82. [DOI] [PubMed] [Google Scholar]
- 7.Khoury T, Karabakhtsian RG, Mattson D, Yan L, Syriac S, Habib F, Liu S, Desouki MM. Pleomorphic lobular carcinoma in situ of the breast: clinicopathological review of 47 cases. Histopathology. 2014;64:981–993. doi: 10.1111/his.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flanagan MR, Rendi MH, Calhoun KE, Anderson BO, Javid SH. Pleomorphic Lobular Carcinoma In Situ: Radiologic-Pathologic Features and Clinical Management. Ann Surg Oncol. 2015;22:4263–4269. doi: 10.1245/s10434-015-4552-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dabbs DJ, Schnitt SJ, Geyer FC, Weigelt B, Baehner FL, Decker T, Eusebi V, Fox SB, Ichihara S, Lakhani SR, Palacios J, Rakha E, Richardson AL, Schmitt FC, Tan PH, Tse GM, Vincent-Salomon A, Ellis IO, Badve S, Reis-Filho JS. Lobular neoplasia of the breast revisited with emphasis on the role of E-cadherin immunohistochemistry. Am J Surg Pathol. 2013;37:e1–11. doi: 10.1097/PAS.0b013e3182918a2b. [DOI] [PubMed] [Google Scholar]
- 10.Lakhani SR, Ellis IO, SJS, Tan PH, Van de Vijver M. WHO Classification of Tumours of the Breast. 4. IARC Press; Lyon: 2012. [Google Scholar]
- 11.Gomes DS, Porto SS, Balabram D, Gobbi H. Inter-observer variability between general pathologists and a specialist in breast pathology in the diagnosis of lobular neoplasia, columnar cell lesions, atypical ductal hyperplasia and ductal carcinoma in situ of the breast. Diagn Pathol. 2014;9:121. doi: 10.1186/1746-1596-9-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Malley FP. Lobular neoplasia: morphology, biological potential and management in core biopsies. Mod Pathol. 2010;23(Suppl 2):S14–25. doi: 10.1038/modpathol.2010.35. [DOI] [PubMed] [Google Scholar]
- 13.Chen YY, Hwang ES, Roy R, DeVries S, Anderson J, Wa C, Fitzgibbons PL, Jacobs TW, MacGrogan G, Peterse H, Vincent-Salomon A, Tokuyasu T, Schnitt SJ, Waldman FM. Genetic and phenotypic characteristics of pleomorphic lobular carcinoma in situ of the breast. Am J Surg Pathol. 2009;33:1683–1694. doi: 10.1097/PAS.0b013e3181b18a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reis-Filho JS, Simpson PT, Jones C, Steele D, Mackay A, Iravani M, Fenwick K, Valgeirsson H, Lambros M, Ashworth A, Palacios J, Schmitt F, Lakhani SR. Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol. 2005;207:1–13. doi: 10.1002/path.1806. [DOI] [PubMed] [Google Scholar]
- 15.Morrogh M, Andrade VP, Giri D, Sakr RA, Paik W, Qin LX, Arroyo CD, Brogi E, Morrow M, King TA. Cadherin-catenin complex dissociation in lobular neoplasia of the breast. Breast Cancer Res Treat. 2012;132:641–652. doi: 10.1007/s10549-011-1860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF American Society of Clinical Oncology, College of American Pathologists. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013. doi: 10.1200/JCO.2013.50.9984. [DOI] [PubMed] [Google Scholar]
- 17.Downs-Kelly E, Bell D, Perkins GH, Sneige N, Middleton LP. Clinical implications of margin involvement by pleomorphic lobular carcinoma in situ. Arch Pathol Lab Med. 2011;135:737–743. doi: 10.1043/2010-0204-OA.1. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan ME, Khan SA, Sullu Y, Schiller C, Susnik B. Lobular carcinoma in situ variants in breast cores: potential for misdiagnosis, upgrade rates at surgical excision, and practical implications. Arch Pathol Lab Med. 2010;134:1024–1028. doi: 10.1043/2009-0300-OA.1. [DOI] [PubMed] [Google Scholar]
- 19.Georgian-Smith D, Lawton TJ. Calcifications of lobular carcinoma in situ of the breast: radiologic-pathologic correlation. AJR Am J Roentgenol. 2001;176:1255–1259. doi: 10.2214/ajr.176.5.1761255. [DOI] [PubMed] [Google Scholar]
- 20.Carder PJ, Shaaban A, Alizadeh Y, Kumarasuwamy V, Liston JC, Sharma N. Screen-detected pleomorphic lobular carcinoma in situ (PLCIS): risk of concurrent invasive malignancy following a core biopsy diagnosis. Histopathology. 2010;57:472–478. doi: 10.1111/j.1365-2559.2010.03634.x. [DOI] [PubMed] [Google Scholar]
- 21.Mahoney MC, Robinson-Smith TM, Shaughnessy EA. Lobular neoplasia at 11-gauge vacuum-assisted stereotactic biopsy: correlation with surgical excisional biopsy and mammographic follow-up. AJR Am J Roentgenol. 2006;187:949–954. doi: 10.2214/AJR.05.0710. [DOI] [PubMed] [Google Scholar]
- 22.Chivukula M, Haynik DM, Brufsky A, Carter G, Dabbs DJ. Pleomorphic lobular carcinoma in situ (PLCIS) on breast core needle biopsies: clinical significance and immunoprofile. Am J Surg Pathol. 2008;32:1721–1726. doi: 10.1097/PAS.0b013e31817dc3a6. [DOI] [PubMed] [Google Scholar]
- 23.King TA, Pilewskie M, Muhsen S, Patil S, Mautner SK, Park A, Oskar S, Guerini-Rocco E, Boafo C, Gooch JC, De Brot M, Reis-Filho JS, Morrogh M, Andrade VP, Sakr RA, Morrow M. Lobular Carcinoma in Situ: A 29-Year Longitudinal Experience Evaluating Clinicopathologic Features and Breast Cancer Risk. J Clin Oncol. 2015;33:3945–3952. doi: 10.1200/JCO.2015.61.4743. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.