Abstract
OBJECTIVE
Appendicitis is frequently diagnosed in the emergency department, most commonly using CT. The purpose of this study was to compare the diagnostic accuracy of contrast-enhanced MRI with that of contrast-enhanced CT for the diagnosis of appendicitis in adolescents when interpreted by abdominal radiologists and pediatric radiologists.
SUBJECTS AND METHODS
Our study included a prospectively enrolled cohort of 48 patients (12–20 years old) with nontraumatic abdominal pain who underwent CT and MRI. Fellowship-trained abdominal and pediatric radiologists reviewed all CT and MRI studies in randomized order, blinded to patient outcome. Likelihood for appendicitis was rated on a 5-point scale (1, definitely not appendicitis; 5, definitely appendicitis) for CT, the unenhanced portion of the MRI, and the entire contrast-enhanced MRI study. ROC curves were generated and AUC compared for each scan type for all six readers and then stratified by radiologist type. Image test characteristics, interrater reliability, and reading times were compared.
RESULTS
Sensitivity and specificity were 85.9% (95% CI, 76.2–92.7%) and 93.8% (95% CI, 89.7–96.7%) for unenhanced MRI, 93.6% (95% CI, 85.6–97.9%) and 94.3% (95% CI, 90.2–97%) for contrast-enhanced MRI, and 93.6% (95% CI, 85.6–97.9%) and 94.3% (95% CI, 90.2–97%) for CT. No difference was found in the diagnostic accuracy or interpretation time when comparing abdominal radiologists to pediatric radiologists (CT, 3.0 min vs 2.8 min; contrast-enhanced MRI, 2.4 min vs 1.8 min; unenhanced MRI, 1.5 min vs 2.3 min). Substantial agreement between abdominal and pediatric radiologists was seen for all methods (κ = 0.72–0.83).
CONCLUSION
The diagnostic accuracy of MRI to diagnose appendicitis was very similar to CT. No statistically significant difference in accuracy was observed between imaging modality or radiologist subspecialty.
Keywords: appendicitis, CT, MRI, pediatric
MDCT is well established for the accurate evaluation of acute, nontraumatic abdominal pain and is the most widely used imaging modality to diagnose appendicitis in the United States [1–5]. Routine preoperative imaging has been shown to significantly decrease negative laparotomy rates; one center reported a 90% reduction in unnecessary surgeries when CT was used regularly to confirm the diagnosis of appendicitis [6].
However, given the concern regarding the ionizing radiation exposure associated with CT scans, radiation-free imaging modalities, including ultrasound (US) and MRI, have been proposed as alternate first-line tests, especially for children. In fact, the American College of Radiology Appropriateness Criteria for right lower quadrant pain (suspected appendicitis) favors the use of US as the first imaging modality for evaluating children under 14 with suspected appendicitis [7]. Unlike MRI, US has the benefit of being widely available and has lower associated charges, yet its widespread adoption has been hindered by its highly variable performance caused by variation in the technical skills of sonographers as well as patient habitus and ability and willingness to lie still [8, 9]. Consequently, several studies have evaluated the use of MRI for the diagnosis of appendicitis, particularly when evaluating pregnant patients and children [10, 11]. Meta-analyses of these studies show that the diagnostic accuracy of MRI for the diagnosis of acute appendicitis is very similar to that of CT [12, 13].
At many institutions, general radiologists interpret imaging tests of children and young adults from the emergency department. However, studies have shown that clinically significant findings may be missed by readers who are not trained in pediatric radiology, even when evaluating something as seemingly straightforward as chest radiographs [14]. Cross-sectional imaging adds another layer of complexity, and although previous reports have presented the discrepancy rate of on-call radiology residents when compared with specialty-trained faculty radiologists [15], few have assessed the discrepancies between interpretations of differently trained subspecialty radiologists. One comparison found that many additional, previously unidentified injuries were found when the abdominal CT scans of pediatric trauma patients referred to a trauma center were reinterpreted by pediatric radiologists [16].
In light of this background, we aimed to assess two key issues in this study. Our primary goal was to determine and compare the diagnostic accuracy of a contrast-enhanced MRI protocol versus contrast-enhanced CT for the diagnosis of acute appendicitis in young patients. Our secondary goal was to determine the difference, if any, in the test accuracy of MRI and CT when interpreted by fellowship-trained pediatric radiologists versus fellowship-trained abdominal radiologists. We hypothesized that the test accuracy of MRI would be similar to that of CT but that the accuracy would be superior when images were interpreted by pediatric radiologists when compared with abdominal radiologists.
Subjects and Methods
Study Design
This study is a subanalysis of a prospective single-center study of patients presenting with acute nontraumatic abdominal pain to the emergency department of an academic tertiary care hospital conducted between February 2012 and August 2014. The study was compliant with HIPAA and was approved by the institutional review board of the University of Wisconsin-Madison. All subjects underwent contrast-enhanced CT for clinical care, followed immediately by contrast-enhanced MRI, which was performed for research purposes only. The imaging protocol has been reported [17]. Briefly, it includes unenhanced T2-weighted imaging, contrast-enhanced T1-weighted imaging, and DWI.
Patient Selection
Patients were eligible for study participation if they were 12–20 years old and had a CT ordered by the emergency department treatment team because of clinical concern for possible appendicitis. The reason for the lower age cutoff was to decrease the likelihood of needing sedation to undergo MRI. Exclusion criteria included standard contraindications to MRI (metallic implants, claustrophobia) or gadolinium-based contrast agents or the inability to provide informed consent or assent.
Study Procedure
After informed consent was obtained, CT was performed using our institution’s routine imaging protocol, which includes an oral contrast preparation for patients 18 years old or older, and no oral contrast material for patients younger than 18 years old. All patients received IV iodinated contrast material (Omnipaque 300, GE Healthcare); CT images were then acquired in the portal venous phase. Within 2 hours of completing CT, patients underwent research MRI, then went back to the emergency department to continue their care. If patients were not able to complete the study because of worsening clinical status or withdrawal by patient choice, the MRI was terminated and they were brought back to the emergency department. Image sets (MRI, CT) were assigned a randomly generated study identification number and were then kept in a de-identified study folder within our PACS for interpretation at a later time, subsequent to the index emergency department visit.
Image Analysis
Three attending, fellowship-trained academic radiologists (with 6, 5, and 2 years’ postfellowship experience) and three attending, fellowship-trained pediatric radiologists (with 4, 3, and 2 years’ postfellowship experience) independently reviewed all CT and MR images during separate sessions and in randomized order, without knowledge of the original CT interpretation or any clinical information about the patient other than the suspicion for appendicitis. Abdominal radiologists were involved in the parent study of this project and read approximately 200 examinations, whereas pediatric radiologists only read the images of patients who were 20 years old or younger. The randomized image interpretation list was different for each radiologist. Using standardized data reporting forms, CT and MR images were interpreted by each radiologist at different times to ensure that interpretation of one imaging type (MRI vs CT) was not influenced by the appearance of the other. Though MRI sequences (contrast-enhanced and unenhanced MRI) were read at the same time, radiologists were asked to first interpret unenhanced MRI using the data reporting form and then to complete another data reporting form for contrast-enhanced MRI to ascertain whether contrast enhancement was useful for rendering an interpretation. DWI was included in the unenhanced MRI sequences. Radiologists rated the likelihood of acute appendicitis on a 5-point Likert scale (1, definitely no appendicitis; 2, probably no appendicitis; 3, possible appendicitis or unsure; 4, probably appendicitis; 5, definitely appendicitis). They were also asked to record their interpretation time for the CT, unenhanced MRI, and contrast-enhanced MRI.
To determine the ground truth with regard to the presence of appendicitis, a trained data abstracter reviewed the electronic medical record of all patients enrolled. In patients who underwent appendectomy, findings from all surgical and pathologic reports were abstracted. For those who did not undergo appendectomy, data from all follow-up visits were abstracted to determine whether the patient subsequently received a diagnosis of appendicitis or another cause for their symptoms. Additionally, these patients underwent a follow-up telephone interview 1 month after their index emergency department encounter using a standard script. The purpose of the telephone interview was to assess whether patients were evaluated for the same symptoms subsequent to the index encounter, underwent interval appendectomy, or received a diagnosis of another cause for their abdominal pain. In addition, three of the nonreader authors (two radiologists and an emergency physician) served as an expert panel to review all abstracted data and render a determination regarding the ground truth (appendicitis or not) for each patient, which served as the reference standard.
Statistical Analysis
Using the reference standard detailed already and the radiologists’ scores for the likelihood of appendicitis, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) as well as positive and negative likelihood ratios for CT, unenhanced MRI, and contrast-enhanced MRI were calculated. A score of 4 (probably appendicitis) or 5 (definitely appendicitis) was considered a positive test result, whereas a score of less than 4 (1, definitely no appendicitis; 2, probably no appendicitis; 3, possible appendicitis or unsure) was considered a negative test result for the presence of appendicitis. ROC curves for the likelihood of appendicitis using each imaging modality were generated and their corresponding AUCs were calculated. The Cohen kappa statistic was used to determine the interrater reliability of each image type. Mean image interpretation times were also calculated. Results are reported for all six radiologists combined as well as stratified by radiologist type (abdominal vs pediatric radiologists), with their respective 95% CIs.
Results
Patient Characteristics
During the study period, we enrolled a total of 230 patients for our parent study. Of these, 48 patients were in the age range that was of interest for this study (12–20 years old; mean age ± SD, 17.1 ± 2.46 years; 28 female [58.3%], 20 male [41.7%]). All MRI examinations were technically adequate, showing that image quality was not a limitation for the purposes of making or excluding diagnoses. Mean time between CT and MRI scans was 54 ± 35 minutes. The prevalence of appendicitis in this cohort of children and young adults was 27% (13/48).
Diagnostic Accuracy
Data from and analysis of the main study determined that a score of 4 was the optimal threshold for determining test positivity. Using this cutoff value, summary sensitivity and specificity of each image type for all radiologists were as follows: for unenhanced MRI, 85.9% (95% CI, 76.2–92.7%) and 93.8% (95% CI, 89.7–96.7%); for contrast-enhanced MRI, 93.6% (95% CI, 85.6–97.9%) and 94.3% (95% CI, 90.2–97%); and for CT, 93.6% (95% CI, 85.6–97.9%) and 94.3% (95% CI, 90.2–97%), respectively. We found no statistically significant difference in either the sensitivity or the specificity of unenhanced MRI, contrast-enhanced MRI, or CT for the diagnosis of appendicitis.
Broken down by radiologist type, the sensitivity and specificity of unenhanced MRI for abdominal radiologists were 84.6% (95% CI, 69.5–94.1%) and 89.5% (95% CI, 82–94.7%) compared with 87.2% (95% CI, 72.6–95.7%) and 98.1% (95% CI, 93.3–99.8%) for pediatric radiologists. For contrast-enhanced MRI, sensitivity and specificity for abdominal radiologists were 100% (95% CI, 91–100%) and 91.4% (95% CI, 84.4–96%) and 87.2% (95% CI, 72.6–95.7%) and 97.1% (95% CI, 91.9–99.4%) for pediatric radiologists. For CT, abdominal radiologists had a sensitivity and specificity of 94.9% (95% CI, 82.7–99.4%) and 92.4% (95% CI, 85.5–96.7%) compared with 92.1% (95% CI, 79.1–98.4%) and 96.2% (95% CI, 90.5–99%) for pediatric radiologists. Table 1 reports PPVs, NPVs, and likelihood ratios. Using the McNemar test to evaluate for differences in test accuracy when comparing pediatric to abdominal radiologists, the only statistically significant difference observed was in the accuracy of contrast-enhanced MRI (p = 0.006). The remaining comparisons were not statistically significant.
TABLE 1.
Comparison of Test Characteristics Between Modalities
| Test Characteristic | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Positive LR | Negative LR | AUC |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Unenhanced MRI | 85.9 | 93.8 | 83.8 | 94.7 | 13.9 | 0.15 | 0.93 |
| 95% CI | 76.2–92.7 | 89.7–96.7 | 73.8–91.1 | 90.7–97.3 | 8.1–23.7 | 0.09–0.26 | 0.89–0.97 |
| Pediatric radiologists | |||||||
| Mean | 87.2 | 98.1 | 94.4 | 95.4 | 45.8 | 0.13 | 0.93 |
| 95% CI | 72.6–95.7 | 93.3–99.8 | 81.3–99.3 | 89.5–98.5 | 11.5–181.6 | 0.06–0.3 | 0.87–0.99 |
| Range | 76.9–100 | 97.1–100 | 90.9–100 | 91.9–100 | 26.9-∞ | 0–0.24 | 0.86–1 |
| Abdominal radiologists | |||||||
| Mean | 84.6 | 89.5 | 75 | 94 | 8.1 | 0.17 | 0.93 |
| 95% CI | 69.5–94.1 | 82–94.7 | 59.7–86.8 | 87.4–97.8 | 4.6–14.4 | 0.08–0.36 | 0.88–0.97 |
| Range | 76.9–100 | 85.7–94.3 | 71.4–83.3 | 91.1–100 | 6.7–13.5 | 0–0.26 | 0.90–0.95 |
| Contrast-enhanced MRI | 93.6 | 94.3 | 85.9 | 97.5 | 16.4 | 0.07 | 0.94 |
| 95% CI | 85.6–97.9 | 90.2–97 | 76.6–92.5 | 94.4–99.2 | 9.4–28.5 | 0.03–0.16 | 0.91–0.97 |
| Pediatric radiologists | |||||||
| Mean | 87.2 | 97.1 | 91.9 | 95.3 | 30.5 | 0.13 | 0.94 |
| 95% CI | 72.6–95.7 | 91.9–99.4 | 78.1–98.3 | 89.4–98.5 | 9.9–93.7 | 0.06–0.3 | 0.89–0.99 |
| Range | 69.2–100 | 94.3–100 | 86–100 | 89–100 | 16.2–00 | 0–0.31 | 0.89–1 |
| Abdominal radiologists | |||||||
| Mean | 100 | 91.4 | 81.3 | 100 | 11.7 | 0 | 0.96 |
| 95% CI | 90–100 | 84.4–96 | 67.4–91.1 | 96.2–100 | 6.3–21.8 | 0–0 | 0.94–0.99 |
| Range | 100–100 | 88.6–94.3 | 76–87 | 100–100 | 8.8–11.7 | 0–0 | 0.95–0.98 |
| Contrast-enhanced CT | 93.6 | 94.3 | 85.9 | 97.5 | 16.4 | 0.07 | 0.97 |
| 95% CI | 85.6–97.9 | 90.2–97 | 76.6–92.5 | 94.4–99.2 | 9.4–28.5 | 0.03–0.16 | 0.94–0.99 |
| Pediatric radiologists | |||||||
| Mean | 92.3 | 96.2 | 90 | 97.1 | 24.2 | 0.08 | 0.96 |
| 95% CI | 79.1–98.4 | 90.5–99 | 76.3–97.2 | 91.8–99.4 | 9.2–63.6 | 0.03–0.24 | 0.92–1 |
| Range | 94.6–100 | 91.4–100 | 80–100 | 94.4–100 | 10.8-∞ | 0–0.16 | 0.94–1 |
| Abdominal radiologists | |||||||
| Mean | 94.9 | 92.4 | 82.2 | 98 | 12.5 | 0.06 | 0.98 |
| 95% CI | 82.7–99.4 | 85.5–96.7 | 68–92 | 92.9–99.8 | 6.4–24.3 | 0.01–0.21 | 0.95–1 |
| Range | 84.6–100 | 88.6–94.3 | 73–86.7 | 93.9–100 | 7.4–17.5 | 0–0.17 | 0.94–1 |
Note—PPV = positive predictive value, NPV = negative predictive value, LR = likelihood ratio.
The interrater reliability (κ) was 0.72 (95% CI, 0.56–0.89) for unenhanced MRI, 0.78 (95% CI, 0.62–0.95) for contrast-enhanced MRI, and 0.83 (95% CI, 0.67–1) for CT. Table 2 shows the examination scoring by modality for each reviewer.
TABLE 2.
Examination Scoring for Each Reviewer and Modality
| Score | Abdominal Radiologist | Pediatric Radiologist | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 1 | 2 | 3 | 1 | 2 | 3 | |
|
| ||||||
| Unenhanced MRI | ||||||
| 1 | 8 | 8 | 8 | 16 | 30 | 32 |
| 2 | 22 | 22 | 18 | 14 | 5 | 2 |
| 3 | 6 | 4 | 4 | 6 | 2 | 1 |
| 4 | 2 | 8 | 2 | 4 | 3 | 2 |
| 5 | 10 | 6 | 16 | 8 | 8 | 11 |
| Contrast-enhanced MRI | ||||||
| 1 | 14 | 16 | 10 | 24 | 33 | 32 |
| 2 | 17 | 14 | 19 | 10 | 5 | 2 |
| 3 | 2 | 2 | 2 | 0 | 0 | 1 |
| 4 | 3 | 2 | 1 | 4 | 1 | 0 |
| 5 | 12 | 14 | 16 | 10 | 9 | 13 |
| Contrast-enhanced CT | ||||||
| 1 | 23 | 22 | 23 | 28 | 35 | 33 |
| 2 | 7 | 8 | 7 | 5 | 1 | 0 |
| 3 | 3 | 3 | 3 | 0 | 0 | 2 |
| 4 | 3 | 3 | 2 | 3 | 1 | 1 |
| 5 | 12 | 12 | 13 | 12 | 11 | 12 |
Note—Scores were assigned according to a 5-point Likert scale: 1, definitely no appendicitis; 2, probably no appendicitis; 3, possible appendicitis or unsure; 4, probably appendicitis; 5, definitely appendicitis.
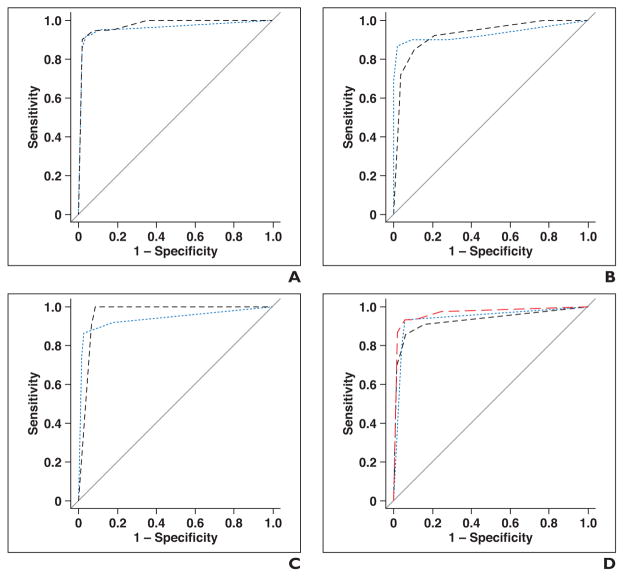
ROC Curve Analysis
The ROC curves and respective AUCs are depicted in Fig. 1. There was no statistically significant difference between the AUCs when comparing the various imaging test types. The point estimate for AUC was greatest for CT at 0.97 (95% CI, 0.94–0.99); it was 0.93 (95% CI, 0.89–0.97) for unenhanced MRI and 0.94 (95% CI, 0.91–0.98) for contrast-enhanced MRI.
Fig. 1.
ROC curves.
A, ROC curve for contrast-enhanced CT for abdominal radiologists (black dashed line, AUC = 0.98 [95% CI, 0.95–1.0]) and pediatric radiologists (blue dotted line, AUC = 0.96 [95% CI, 0.92–1.0]). Diagonal line represents line of reference.
B, ROC curve for unenhanced MRI for abdominal radiologists (black dashed line, AUC = 0.93 [95% CI, 0.88–0.97]) and pediatric radiologists (blue dotted line, AUC = 0.93 [95% CI, 0.87–0.99]). Diagonal line represents line of reference.
C, ROC curve for contrast-enhanced MRI for abdominal radiologists (black dashed line, AUC = 0.96 [95% CI, 0.94–0.99]) and pediatric radiologists (blue dotted line, AUC = 0.94 [95% CI, 0.89–0.99]). Diagonal line represents line of reference.
D, Composite ROC curve depicting accuracy of each imaging type when accounting for all six reviewers is also presented. Black dashed line represents unenhanced MRI (AUC = 0.93 [95% CI, 0.89–0.97]), blue dotted line represents contrast-enhanced MRI (AUC = 0.98 [95% CI, 0.91–0.97]), and red dashed line represents contrast-enhanced CT (AUC = 0.97 [95% CI, 0.94–0.99]). Diagonal line represents line of reference.
Interpretation Time
For CT, mean interpretation time for abdominal radiologists was 3.0 min (95% CI, 2.4–3.6 min) compared with 2.8 min (95% CI, 2.2–3.4 min) for pediatric radiologists (p = 0.57; mean for all reviewers, 2.9 min). Interpretation time for unenhanced MRI was 1.5 min (95% CI, 0.9–2.2 min) for abdominal radiologists compared with 2.3 min (95% CI, 1.7–2.9) for pediatric radiologists (p = 0.074; mean for all reviewers, 1.9 min). For contrast-enhanced MRI, abdominal radiologists needed a mean time of 2.4 min (95% CI, 1.8–3.0 min), compared with 1.8 min (95% CI, 1.1–2.4 min) for the pediatric radiologists (p = 0.132; mean for all reviewers, 3.1 min). No statistically significant difference was seen in the interpretation times of the different modalities when comparing radiologist types. When comparing interpretation time of imaging types (i.e., CT vs unenhanced MRI, CT vs contrast-enhanced MRI, and contrast-enhanced MRI vs unenhanced MRI), all comparisons revealed statistically significant differences (unenhanced MRI vs contrast-enhanced MRI for pediatric radiologists, p = 0.002; otherwise, p < 0.001).
Relevant Examples
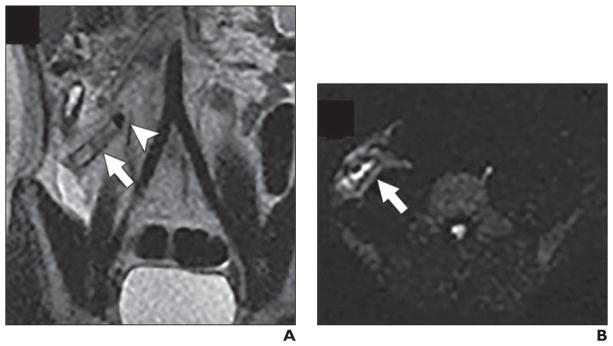
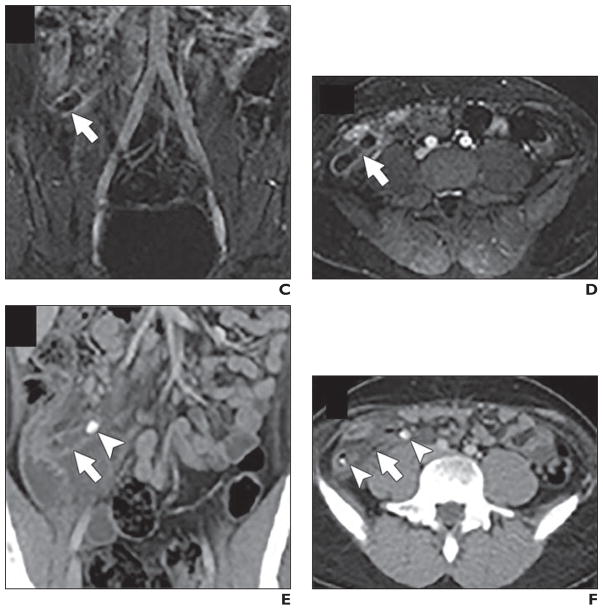
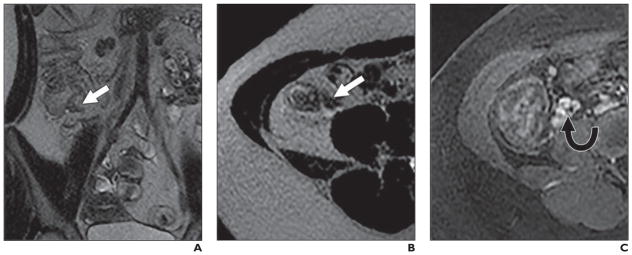
Figures 2–4 show examples of CT and MR images from patients included in this study, including two cases of appendicitis (Figs. 2 and 3) and a case of an acute exacerbation of Crohn disease (Fig. 4). Figure captions describe how the radiologists interpreted the cases.
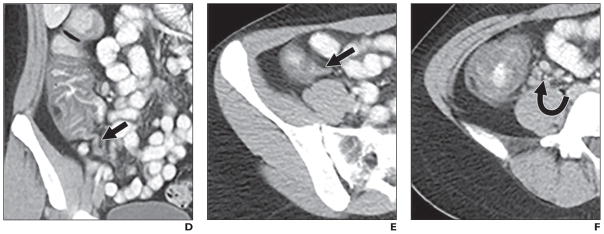
Fig. 2.
17-year-old girl with acute abdominal pain correctly diagnosed as acute appendicitis. All six radiologists rated this case as definitely appendicitis (score, 5) in all imaging modalities (appendix indicated by arrow).
A and B, Unenhanced coronal T2-weighted MRI sequence (A) and axial DWI sequence (B). Appendicolith is seen (arrowhead, A).
17-year-old girl with acute abdominal pain correctly diagnosed as acute appendicitis. All six radiologists rated this case as definitely appendicitis (score, 5) in all imaging modalities (appendix indicated by arrow).
C and D, Coronal contrast-enhanced MR image acquired after 90 s (C) and axial contrast-enhanced MR image acquired during arterial phase (D). E and F, Coronal (E) and axial (F) CT scans. Appendicoliths are seen (arrowheads).
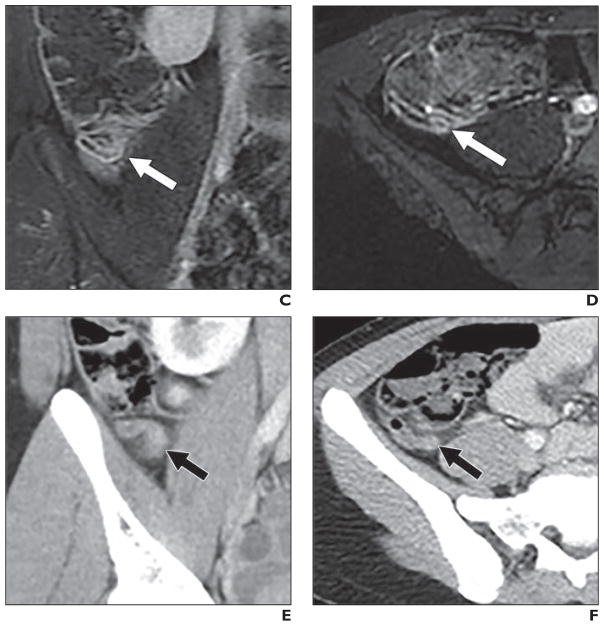
Fig. 4.
18-year-old woman with acute abdominal pain.
A and B, Axial (A) and coronal (B) T2-weighted unenhanced MR images shows appendix (arrow). All three pediatric radiologists rated appendicitis likelihood as 2 (probably no appendicitis), whereas one abdominal radiologist stated 4 (probably appendicitis); another, 3 (possible appendicitis or unsure); and another, 1 (definitely no appendicitis).
C, Contrast-enhanced MRI shows lymphadenopathy (arrow). With contrast-enhanced MRI, two abdominal radiologists rated it 1 (definitely no appendicitis) whereas one abdominal and two pediatric radiologists rated it 2 (probably no appendicitis).
18-year-old woman with acute abdominal pain.
D–F, Contrast-enhanced CT. All radiologists agreed on rating of 1 (definitely no appendicitis). Patient was found to have Crohn disease with involvement of cecum (D) and ascending colon (E), as well as lymphadenopathy (arrow, F), but no appendicitis. Arrows in D and E denote appendix.
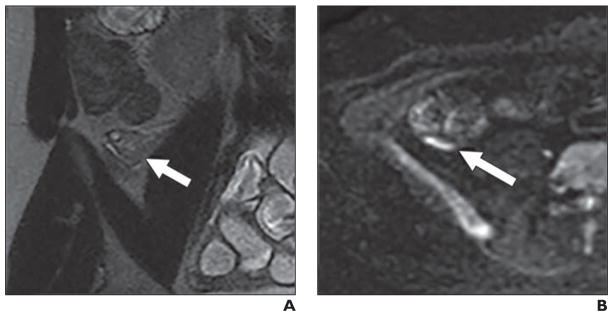
Fig. 3.
20-year-old woman with acute abdominal pain who underwent appendectomy, confirming diagnosis of appendicitis.
A and B, Unenhanced coronal T2-weighted MRI (A) and axial DWI (B) with high signal intensity on DWI. Two pediatric radiologists evaluated images as definitely no appendicitis (score, 1) and one as definitely appendicitis (score, 5), whereas two abdominal radiologists rated images as definitely appendicitis (score, 5) and one was unsure (score, 3). Arrows denote appendix.
20-year-old woman with acute abdominal pain who underwent appendectomy, confirming diagnosis of appendicitis.
C–F, Coronal (C) and axial (D) contrast-enhanced MR images show contrast uptake in appendix (arrow) as sign of inflammation. Axial (E) and coronal (F) contrast-enhanced CT scans show slightly thickened and enhancing appendix (arrow). For MR images as well as CT scans, one pediatric radiologist stated definitely no appendicitis (score, 1) and all others rated images as definitely appendicitis (score, 5).
Discussion
In this study, we found that the diagnostic accuracies of MRI and CT for the diagnosis of acute appendicitis in adolescents and young adults presenting with abdominal pain are very similar. Moreover, we did not find a statistically significant difference in the test characteristics of MRI for the diagnosis of appendicitis when interpreted by abdominal radiologists versus pediatric radiologists. Interpretation times for MRI were longer than CT, but there was no statistically significant difference in interpretation time when comparing abdominal radiologists to pediatric radiologists.
The highest sensitivity values for abdominal radiologists were observed when reading contrast-enhanced MRI, whereas pediatric radiologists demonstrated their highest sensitivity when interpreting CT. Specificity values were highest for abdominal radiologists when interpreting CT compared with unenhanced MRI for pediatric radiologists. Notably, unenhanced MRI was more accurately interpreted by pediatric radiologists when compared with abdominal radiologists. This result may be related to pediatric radiologists having more experience and comfort with the interpretation of unenhanced MRI in general compared with abdominal radiologists. Interrater reliability was slightly higher for CT compared with contrast-enhanced and unenhanced MRI, but we believe this difference is negligible and should not affect the test choice.
A study conducted by Rosines et al. [18] reported that contrast-enhanced images are helpful for the assessment of acute appendicitis in the pediatric population. However, those authors did not include DWI in their MRI protocol, which has proven valuable in other abdominal and bowel diseases [19]. Bayraktutan et al. [20] compared DWI with conventional unenhanced MRI and found that the combination of all sequences led to best sensitivity (92%) when evaluating for acute appendicitis. Our study is the first to compare unenhanced MRI versus contrast-enhanced MRI for the detection of appendicitis in pediatric patients, including the use of DWI. We did not detect a statistically significant difference between unenhanced MRI compared with contrast-enhanced MRI for either radiologist type, nor was there a difference when we combined the interpretations of all radiologists.
Each imaging modality has its own benefits and drawbacks apart from the diagnostic accuracy and interreader agreement: Contrast-enhanced CT and contrast-enhanced MRI require IV access, whereas an unenhanced MRI can be performed without this burden, which can be beneficial in an already anguished pediatric patient. MRI (unenhanced or contrast-enhanced) on the other hand, is often not as readily available as CT, but CT carries the burden of radiation exposure. Therefore, we believe that these advantages and disadvantages favor MRI, especially unenhanced MRI.
There are a number of limitations in our study. First, appendicitis most commonly afflicts patients aged 10–19 years, with a rate of 23.3 cases per 10,000 per year [21]. Therefore, only enrolling patients who were over 12 years old may have missed a small but relevant segment of patients. These patients are routinely evaluated by pediatric radiologists, which may have impacted our ability to detect a difference in interpretation accuracy between the two types of radiologists. Patients younger than 12 years may require sedation for MRI, which was the reason that younger patients were not included in this study. Furthermore, by expanding the upper age limit to 20 years, we included a cohort of patients with whom pediatric radiologists have less experience. Another limitation is the sample size for this study; we included 48 patients for this analysis, which may have limited the ability to observe a statistically significant difference between CT and MRI as well as between the diagnostic accuracy of abdominal versus pediatric radiologists. Although the study may be too small to detect a statistical difference, the degree of clinical difference between tests was minimal.
Finally, differential training between radiologist types may also have biased our results. All abdominal radiologists in our study interpreted over 200 cases for our parent study, whereas the pediatric radiologists only interpreted the 48 cases presented in this substudy. Results from Leeuwenburgh et al. [22] suggest that diagnostic accuracy may improve after interpreting approximately 100 examinations. Even so, all of the pediatric and abdominal radiologists involved in this study had significant experience in the interpretation of MRI of the bowel, including MR enterography, which may limit generalizability.
In conclusion, in this small prospective study, we did not detect a statistically or clinically significant difference in diagnostic performance of CT versus MRI for acute appendicitis in patients 12–20 years old. No significant difference in the diagnostic accuracy or interpretation times was observed between abdominal and pediatric radiologists. When using only unenhanced MRI, pediatric radiologists showed improved sensitivity and specificity compared with abdominal radiologists. Training radiologists to read MR images for possible appendicitis may further increase their diagnostic accuracy.
Acknowledgments
Supported by grants UL1TR00427, KL2TR000428, K24DK102595, and K08DK111234 from the National Institutes of Health.
References
- 1.Pickuth D, Heywang-Köbrunner SH, Spielmann RP. Suspected acute appendicitis: is ultrasonography or computed tomography the preferred imaging technique? Eur J Surg. 2000;166:315–319. doi: 10.1080/110241500750009177. [DOI] [PubMed] [Google Scholar]
- 2.Tseng YC, Lee MS, Chang YJ, Wu HP. Acute abdomen in pediatric patients admitted to the pediatric emergency department. Pediatr Neonatol. 2008;49:126–134. doi: 10.1016/S1875-9572(08)60027-3. [DOI] [PubMed] [Google Scholar]
- 3.Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789–796. doi: 10.7326/0003-4819-154-12-201106210-00006. [DOI] [PubMed] [Google Scholar]
- 4.Glass CC, Saito JM, Sidhwa F, et al. Diagnostic imaging practices for children with suspected appendicitis evaluated at definitive care hospitals and their associated referral centers. J Ped Surg. 2016;51:912–916. doi: 10.1016/j.jpedsurg.2016.02.055. [DOI] [PubMed] [Google Scholar]
- 5.Saito JM, Yan Y, Evashwick TW, Warner BW, Tarr PI. Use and accuracy of diagnostic imaging by hospital type in pediatric appendicitis. Pediatrics. 2013;131:e37–e44. doi: 10.1542/peds.2012-1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010;256:460–465. doi: 10.1148/radiol.10091570. [DOI] [PubMed] [Google Scholar]
- 7.Smith MP, Katz DS, Lalani T, et al. ACR appropriateness criteria: right lower quadrant pain—suspected appendicitis. Ultrasound Q. 2015;31:85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 8.Pershad J, Waters TM, Langham MR, Jr, Li T, Huang EY. Cost-effectiveness of diagnostic approaches to suspected appendicitis in children. J Am Coll Surg. 2015;220:738–746. doi: 10.1016/j.jamcollsurg.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 9.Binkovitz LA, Unsdorfer KL, Thapa P, et al. Pediatric appendiceal ultrasound: accuracy, determinacy and clinical outcomes. Pediatr Radiol. 2015;45:1934–1944. doi: 10.1007/s00247-015-3432-7. [DOI] [PubMed] [Google Scholar]
- 10.Burke LM, Bashir MR, Miller FH, et al. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol. 2015;213:693e1–6. doi: 10.1016/j.ajog.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 11.Orth RC, Guillerman RP, Zhang W, Masand P, Bisset GS., III Prospective comparison of MR imaging and US for the diagnosis of pediatric appendicitis. Radiology. 2014;272:233–240. doi: 10.1148/radiol.14132206. [DOI] [PubMed] [Google Scholar]
- 12.Repplinger MD, Levy JF, Peethumnongsin E, et al. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging. 2016;43:1346–1354. doi: 10.1002/jmri.25115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duke E, Kalb B, Arif-Tiwari H, et al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR. 2016;206:508–517. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 14.Soudack M, Raviv-Zilka L, Ben-Shlush A, Jacobson JM, Benacon M, Augarten A. Who should be reading chest radiographs in the pediatric emergency department? Pediatr Emerg Care. 2012;28:1052–1054. doi: 10.1097/PEC.0b013e31826caf3f. [DOI] [PubMed] [Google Scholar]
- 15.Ruma J, Klein KA, Chong S, et al. Cross-sectional examination interpretation discrepancies between on-call diagnostic radiology residents and subspecialty faculty radiologists: analysis by imaging modality and subspecialty. J Am Coll Radiol. 2011;8:409–414. doi: 10.1016/j.jacr.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 16.Onwubiko C, Mooney DP. The value of official reinterpretation of trauma computed tomography scans from referring hospitals. J Pediatr Surg. 2016;51:486–489. doi: 10.1016/j.jpedsurg.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Kinner S, Repplinger MD, Pickhardt PJ, Reeder SB. Contrast-enhanced abdominal MRI for suspected appendicitis: how we do it. AJR. 2016;207:49–57. doi: 10.2214/AJR.15.15948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosines LA, Chow DS, Lampl BS, et al. Value of gadolinium-enhanced MRI in detection of acute appendicitis in children and adolescents. AJR. 2014;203:W543–W548. doi: 10.2214/AJR.13.12093. [web] [DOI] [PubMed] [Google Scholar]
- 19.Chavhan GB, AlSabban Z, Babyn PS. Diffusion-weighted imaging in pediatric body MR imaging: principles, technique, and emerging applications. RadioGraphics. 2014;34:E73–E88. doi: 10.1148/rg.343135047. [DOI] [PubMed] [Google Scholar]
- 20.Bayraktutan Ü, Oral A, Kantarci M, et al. Diagnostic performance of diffusion-weighted MR imaging in detecting acute appendicitis in children: comparison with conventional MRI and surgical findings. J Magn Reson Imaging. 2014;39:1518–1524. doi: 10.1002/jmri.24316. [DOI] [PubMed] [Google Scholar]
- 21.Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res. 2012;175:185–190. doi: 10.1016/j.jss.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 22.Leeuwenburgh MM, Wiarda BM, Bipat S, et al. Acute appendicitis on abdominal MR images: training readers to improve diagnostic accuracy. Radiology. 2012;264:455–463. doi: 10.1148/radiol.12111896. [DOI] [PubMed] [Google Scholar]