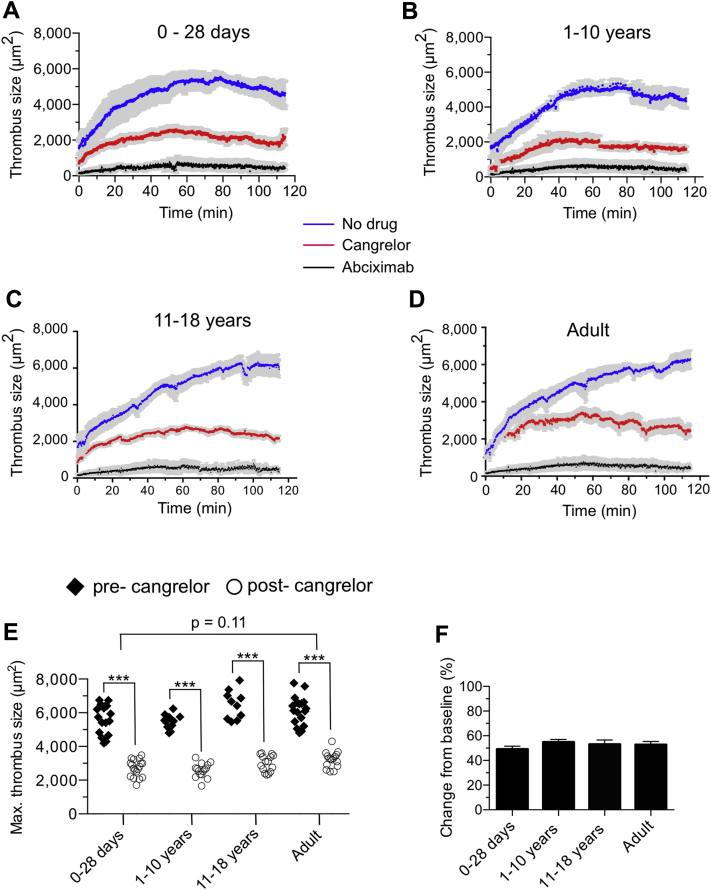
Figure 3.
Cangrelor Reduces Human Platelet Thrombus Formation in Avatar Mice
(A to D) Time course of fluorescent platelets accumulating on laser-injured arterioles contained with the cremaster muscle of von Willebrand factorHA1 mice. Cangrelor (30-μg/kg bolus; 4-μg/kg/min infusion) or abciximab (0.25-μg/kg bolus; 0.125-μg/kg/min infusion) were administered intravenously after establishing baseline thrombus formation in the absence of drug. n = 15 (age 0 to 28 days); n = 10 (age 1 to 10 years); n = 8 (age 11 to 18 years); n = 15 for adults. (E) Maximal thrombus size pre- and post-administration of cangrelor in the same animal. Each symbol represents the area of a thrombus in 1 arteriole of an avatar mouse. (F) Percent change in thrombus size in response to cangrelor treatment based on data shown in E. See Supplemental Video 2. Data represent mean ± SEM. ***p < 0.001 for drug versus no treatment according to the Mann-Whitney U test.
Cangrelor Reduces Human Platelet Thrombus Formation in Laser-Injured Arterioles of VWFHA1 Mutant Mice
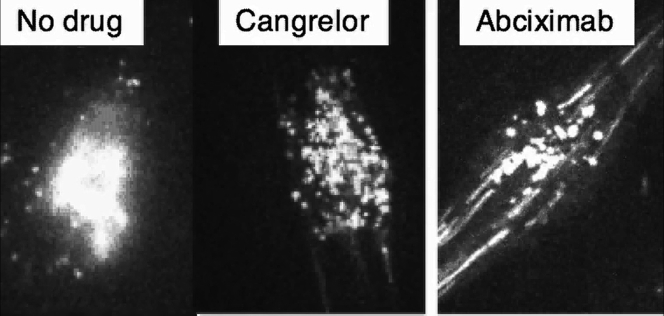
Video demonstrates the ability of the P2Y12 antagonist cangrelor (30-μg/kg bolus; 4-μg/kg/h infusion) to significantly reduce the ability of platelets from a neonatal cardiac patient from supporting thrombus growth without preventing core formation. In contrast, administration of the integrin αIIbβ3 blocker abciximab (0.25-μg/kg bolus; 0.125-μg/kg/min infusion) nearly abrogates platelet–vessel wall interactions, thereby preventing all aspects of thrombus formation (see Figure 6). Thrombus formation before administration of cangrelor is shown for comparison in the same animal. A new von Willebrand factor (VWF)HA1 mouse was used to assess the effects of abciximab.