Abstract
The burden of substance use and especially the unmatched rates of overdoses in rural Central Appalachia highlight the need for innovative approaches to curb the initiation to drug misuse and to address current substance use disorders. Effective substance use interventions involve a thorough understanding of the region. In Central Appalachia, many of the barriers to treatment are shared with other rural and impoverished areas, including a lack of access to health care and lack of health care providers with specialized training. Parts of Appalachia also present their own considerations, including the challenges of fostering trust and encouraging treatment-seeking in communities with dense, long-term, place-based social and family networks. Current policies and interventions for substance use have been largely inadequate in the region, as evidenced by continued increases in substance use and substance-related deaths, especially related to nonmedical prescription drug use and increasing heroin use. The authors discuss ways in which rural life, poverty, identity, and values in Appalachia have influenced substance use and treatment and propose strategies and interventions to improve outcomes.
Keywords: Addiction, opioid use, Appalachia, treatment, injection drug use, rural
Substance Use in Rural Appalachia
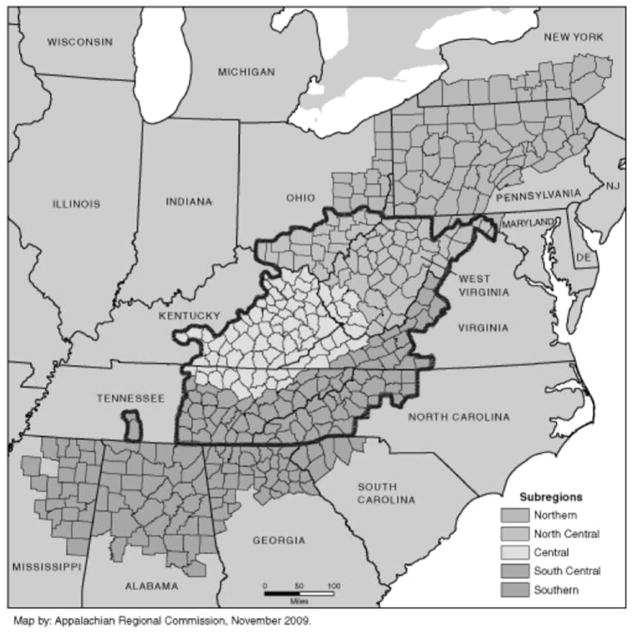
Substance use has increased steadily in rural Appalachia over the past two decades (Centers for Disease Control and Prevention [CDC], 2011; Havens, Walker, & Leukefeld, 2007). Prescription medications, specifically opioids, are abused at rates exceeding national averages in rural Appalachia, resulting in a negative impact on the health of the overall population (CDC, 2011; Zhang et al., 2008). Nonmedical prescription drug use is of particular concern in rural Central Appalachia (see counties in West Virginia, Southwest Virginia, Eastern Kentucky, Southeast Ohio, East Tennessee, and Western North Carolina outlined in Figure 1), with among the highest rates of use and overdoses across the US (CDC, 2011; Havens et al., 2013; Havens et al., 2007; Jonas, Young, Oser, Leukefeld, & Havens, 2012; Young & Havens, 2012). Currently, West Virginia has the highest rate of drug overdoses in the country, with an age adjusted rate of 35.5 overdoses per 100,000 inhabitants compared to a national average of 14.7 per 100,000 persons (CDC, 2015; Rudd, Aleshire, Zibbell, & Gladden, 2016). Despite high rates of opioid misuse throughout West Virginia and surrounding areas, drug use in coalmining regions of rural Central Appalachia (“the coalfields,” concentrated especially in Eastern Kentucky and Southern West Virginia, plus counties in Virginia, Tennessee, and Ohio) are over and above even those of rural non-coalmining Appalachia, indicating that people living in coalmining regions, specifically those with mountaintop coal removal, are at increased risk of developing substance use disorders (Steele, 2015; Zhang et al., 2008).
Figure 1.
The outlined regions depicts counties in Central Appalachia.
Patterns of drug use in Central Appalachia are distinctive to the region in that low education levels, high rates of unemployment, and high rates of job related injuries perpetuate risks for substance use (Coalition on Appalachian Substance Abuse Prevention [CASAP], 2016). In addition, a long history of anti-regulatory sentiments in the region may create resistance to legal efforts to curb substance sales and use (CASAP, 2016) and a paucity of training in substance use treatment for medical providers leaves many minimally equipped to address substance use disorders (CASAP, 2016). Importantly, Hansen and Resick (1990) described rural Appalachians as often living in a largely “self-contained culture” similar to other minority groups such as Native American and Amish communities. Such groups may resist Western medicine approaches. However, unlike the subcultures of Native American and Amish people, the distinct ways of life and belief systems of Appalachians are less readily acknowledged. Specifically, Appalachians appear consistent with normative middle class Americans in race, religion, ancestry, and language. Similarities between normative Americans and rural Appalachians may work against Appalachians in that less emphasis is placed on awareness and specialized training to facilitate understanding of local beliefs that could lead to better patient experiences and improved treatment outcomes (Hansen & Resick, 1990).
Many factors have contributed to the rise in nonmedical prescription drug use. For example, historically, Central Appalachia has had a large number of physical laborers (e.g., coal miners and loggers), making the population prone to workplace injury and chronic pain. In the late twentieth century, new synthetic painkillers (the FDA approved prescription opiates Vicodin in 1984, OxyContin in 1995, and Percocet in 1999) provided such workers with relief (Kobak, 2012; Van Zee & Kobak, 2015). This concentration of need, in combination with inadequate federal and state regulation and pharmaceutical companies’ marketing of prescription pain medications to physicians in regions with high demand for pain treatment (“Drug firms,” 2016; Kobak, 2012), resulted in increased prescription drug availability (Bates, 2008; Kobak, 2014), with prescription rates of OxyContin five to six times higher than national averages in some counties (“Drug Firms,” 2016). In Central Appalachia, high rates of chronic pain, inadequate regulatory oversight, and targeted marketing by pharmaceutical companies led to prescription pain medications that were readily available (Zhang et al., 2008). In conjunction, too little public health education about the risks and abuse liability tied to prescription pain drugs resulted in individuals who were unaware of the consequences of initiating use (Zhang et al., 2008).
Throughout Central Appalachia, opioid and polysubstance misuse often translate into injection drug use and, in turn, high rates of blood-borne diseases such as Hepatitis C and HIV, which have increased the region’s social and economic burdens. Until the 2010 release of a reformulated, controlled-release version, OxyContin was the primary pathway to injection drug use in Central Appalachia (Young & Havens, 2012). From 2006 to 2012, rates of Hepatitis C infection, the most common blood-borne infection in the United States, skyrocketed in Central Appalachia; most conspicuously, rates of Hepatitis C in people under 30 in Central Appalachian states increased 364% (Zibbell et al., 2015). The notable rise in Hepatitis C across the Central Appalachian region coincided with a 21.1% increase in treatment admissions for opioid dependence and a 12.6% increase in patients’ reporting that injection was their primary route of drug administration (Zibbell et al., 2015). In other rural parts of the country, increases in Hepatitis C have preceded HIV outbreaks, raising concern over the potential for elevated rates of HIV in rural Appalachia (Havens et al., 2013; Indiana State Department of Health, 2015; Van Handel et al., 2016; Zibbell et al., 2015). In order to curb further spread of blood-borne viruses via injection drug use, a concerted focus in the region to educate, treat, and offer safer alternatives to residents is necessary.
Considerations for Substance Use Treatment
Many characteristics of Appalachia make substance use treatment difficult and distinctive when compared to other impoverished areas (CASAP, 2016). Shortcomings in effective treatment of substance use problems in rural Appalachia include: (1) lack of access to health professionals because of cost and insufficient health insurance coverage; (2) lack of access to qualified health care providers as a result of travel distance, lack of training in evidence-based and evidence-supported treatments, and/or lack of trust in health professionals to provide effective treatment; and (3) lack of educational and economic opportunity contributing to systemic poverty, a key determinant of higher rates of substance abuse (CASAP, 2016). Each of these points is discussed in turn.
Health Insurance Coverage
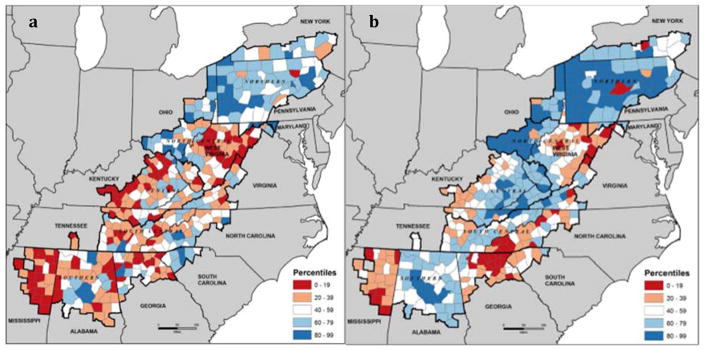
Rural residents have less access to health care broadly (Caldwell, Ford, Wallace, Wang, & Takahashi, 2016), and mental health care specifically (Reschovsky & Staiti, 2005), compared to urban residents; moreover, individuals suffering from substance use problems are less likely to be insured compared to their non-addicted counterparts (Hendryx, 2008). The Healthcare Costs, Coverage, and Access (HCCA) index, a composite score that weighs county-by-county access to health care, insurance coverage, and costs, reported that Central Appalachian counties that are not contiguous to metropolitan areas have disproportionately lower index scores (Lane et al., 2012). The low HCCA index scores in non-adjacent counties are, in part, driven by high rates of uninsured individuals, as shown in Figure 2. Although this report was conducted specifically on behalf of the Appalachian Regional Commission, it suggests that the other areas of the country with extremely low HCCA scores comparable to those in very rural Appalachia are broad areas of Texas, Louisiana, and Florida with high percentages of Latino immigration (Lane et al., 2012). The extent to which these health care access disparities will persist or be reduced in rural Appalachia may be contingent on the future of the Patient Protection and Affordable Care Act.
Figure 2.
County healthcare cost, coverage, and access index scores across Appalachia (from Lane et al., 2012, Health Care Costs and Access Disparities in Apppalachia, Appalachian Regional Commission). Blue represents good access, coverage, and payment compared to the national average. White indicates the County’s index score is close to the national average. Red indicates the index score is well below the national average. Panel a shows the combined index scores for cost, coverage, and access. Panel b shows the percentiles for healthcare insurance coverage only.
Between its passage in 2010 and 2016, the Affordable Care Act has increased coverage rates for people across America, and the subsequent expansion of the Medicaid program increased coverage for people in participating states (Courtemanche, Martin, Ukert, Yelowitz & Zapata, 2016). In 2015, the decrease in uninsured individuals in Central Appalachia was among the greatest in the nation (Witters, 2016), in part because Kentucky and West Virginia adopted both the Medicaid expansion and health care insurance exchange programs. In Kentucky, the rate of uninsured individuals went from 20.4% in 2013 to 7.5% in 2015 (Witters, 2016). Similarly, uninsured rates in West Virginia went from 17.6% in 2013 to 7.7% in 2015 (Witters, 2016). Other Central Appalachian states, including Tennessee and Virginia, have not adopted the Medicaid Expansion and as such have not seen these marked increases in health insurance coverage Kaiser Family Foundation, 2016). Medicaid expansion, and specifically the coverage of otherwise uncompensated care costs, not only provides more access for individuals, but also disproportionately benefits rural health care providers by stabilizing funding sources (State Health Reform Assistance Network, 2016).
Improvements in rates of health insurance coverage and in services covered by health insurance have offered some relief in Central Appalachia and rural areas in general, but the current political environment threatens recent gains. Additionally, greater and relatively easy access to substance use services are still needed (Watson, 2011) especially given that rural areas, as compared to urban centers, have fewer mental health providers per capita and lower availability of specialized providers such as addiction psychologists and psychiatrists (Hendryx, 2008).
Providers
In Central Appalachia, as in other rural areas, health professionals qualified to provide efficacious treatment may be prohibitively far away. According to the Appalachian Regional Commission, approximately 55% of people living in Central Appalachia are in rural areas compared to 20% of the national population (Housing Assistance Council, 2010). The rurality of much of Central Appalachian may make access to health professionals disproportionately costly, especially for those who are uninsured. Moreover, rural health care providers nationally, including those tasked with treating substance use disorders, may not receive sufficient training in evidence-based treatments. Indeed, rural providers are less likely to use empirically-based interventions than those in urban areas (Dotson et al., 2014), further increasing barriers to treatment access. A lack of training availability can result in outdated treatment modalities that are minimally effective or even detrimental to recovery. Furthermore, training and implementation of evidence-based treatments (discussed in a section to follow) may better leverage strengths of Central Appalachian and other rural communities.
In addition to insufficient training of rural health care providers, Appalachian stereotypes such as fundamentalism, primitivism, isolationism, backwardness, and homogeneity (Billings, 2000; Scott, 2010) stand in the way of some health care providers’ accurately understanding people living in this region (Coyne, Demian-Popescu, & Friend, 2006). Focus groups to identify beliefs of those living in Appalachia show promise as a way to unearth—rather than presume—pertinent values. In Central Appalachia, focus groups have identified economic disparity, unemployment, and under-education as characteristics that may increase both substance use and treatment failure (Coyne et al., 2006). Characteristics such as strong faith in God, strong family ties, strong sense of pride, and valuing self-sufficiency, on the other hand, may act as preventative factors and help to bolster treatment effectiveness in the region (Coyne et al., 2006; Zhang et al., 2008).
Distrust or fear of stigma on the part of some Appalachian residents toward mental health professionals may present a challenge for substance use treatment in Central Appalachia (Zhang et al., 2008). Focus groups revealed a distrust of medical professionals for fear that they might prescribe drugs that will lead to addiction and concern that private family problems will become public (Coyne et al., 2006). Moreover, Appalachians in Southern West Virginia noted discomfort with medical professionals born outside the United States because of presumed cultural differences that resulted in poor relationships between the provider and patient (Coyne et al., 2006). The lack of trust in health care professionals hinders treatment seeking and treatment compliance in the region, underscoring the need for community-based initiatives to repair trust.
Social Determinants of Health
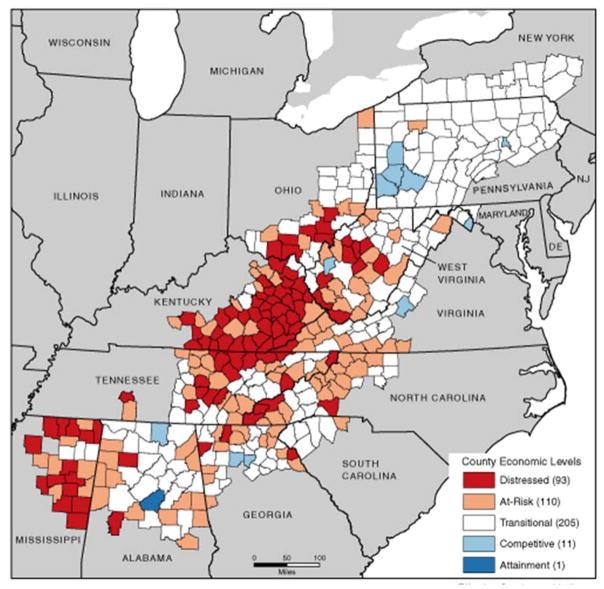
Several social determinants of health, such as poverty and economic distress, are closely tied to other contributing factors for substance use, including lack of health care coverage and a lack of sufficiently trained and accessible health care providers. Nonetheless, these factors perpetuate the risk for substance use problems (Appalachian Regional Commission, 2013; CASAP, 2016; Leukefeld, Walker, Havens, Leedham, & Tolbert, 2007; Schoeneberger, Leukefeld, Hiller, & Godlaski, 2006). Central Appalachian counties are disproportionately impoverished even when compared to other areas in Appalachia (see Figure 3). In addition, Central Appalachian counties are occupationally distressed and these counties largely cluster around coalmining areas already at greater risk of prescription drug abuse (as discussed above). The combination of poverty, occupational distress, lack of health care coverage, and the shortage of qualified providers of substance use treatments underscore the growing need for multifaceted policies interventions in the region.
Figure 3.
Appalachian Regional Commission county-by-county map of economic disparity.
Strategies for Substance Abuse Programs and Treatments
Central Appalachia needs improved substance use interventions because of the high rates of use and to the unparalleled economic and social burden that substance use causes for the people living in this area (Leukefeld et al., 2007; Schoeneberger et al., 2006). Successful interventions in rural Central Appalachia will require (1) public health dissemination strategies adapted to the region, (2) greater reliance on evidenced-based treatment strategies, and (3) the expansion of telehealth in the absence of a more equitable distribution of health providers.
Public Health Initiatives
Well-crafted public health interventions can facilitate better dissemination and acceptability of substance use treatment. Effective outreach followed by treatment implementation strategies sensitive to regional characteristics, such as skepticism of influence from unfamiliar sources and strength of familial and social networks, may increase treatment acceptability and outcomes. Additionally, culturally appropriate public health strategies that foster trust and community involvement may lower the threshold for treatment seeking and provide a reduction in public health burden for those not yet ready to stop substance use.
Lay health providers, or local residents who receive frontline training and offer initial treatment, may serve as a bridge between community members and specialized health care providers by offering referrals from a trusted source to more specialized providers (Eng & Young, 1992; Wewers et al., 2016; Zuvekas, Nolan, Tumaylle, & Griffin, 1999). Given that some individuals in Appalachia report a distrust of health care professionals (Coyne et al., 2006), the use of long-time community members to provide the first line of care may be especially important for this region. Moreover, the training provided to lay health providers may help to raise awareness of relatively high levels of disparity and unmet need compared to national health standards (Halverson, Friedell, Cantrell, & Behringer, 2012).
Another public health strategy, participatory development, includes community members in planning and decision-making to build ties and trust between outside agencies and locals (Keefe, 2009). Participatory development values local cultures, community organizations, collaboration between mental health professionals and community members, and empowerment of local individuals (Prokopy & Castelloe, 1999). These models facilitate people-focused plans that foster local leadership, such as that provided by lay health advisors, and increase participation by at-risk members of the population. The success of a participatory development program is measured by its sustainability without, or with minimal, outside help. Given the reports from focus groups in the region (Coyne et al., 2006), inclusion of local religious leaders in program development and triage care may aid in acceptability of implementation and dissemination strategies.
In addition to public health models that increase community involvement and acceptability, integrated health care models facilitate the housing of medical and mental health facilities together. By providing joint accommodations for both services, patients receive multiple benefits, including increased convenience and decreased stigma related to mental health treatment (Franko, 2014). Moreover, for individuals suffering from multiple health problems or chronic diseases, integrated care models have a positive economic impact for the patient (Desmedt et al., 2016). Continued movement toward these models may provide increased access, reduced stigma, and reduced economic burden for individuals living the rural Central Appalachia.
Finally, syringe exchange programs, or the provision of free access to clean syringes and disposal of used syringes, are needed in Central Appalachia. Given that use of nonprescription opioids is a major risk factor for progressing into injection drug use (Havens et al., 2007; Leukefeld et al., 2005; Young & Havens, 2012), and that injection drug use is associated with increased risk for infectious diseases such as Hepatitis C and HIV (Havens et al., 2013), syringe exchange programs provide a harm reduction technique to reduce the spread of infectious disease. Syringe exchange programs prevent the spread of infectious disease by providing a front-line alternative for injection drug users (Hyshka, Strathdee, Wood, & Kerr, 2012). Importantly, these programs have been successful in other rural areas (Strathdee & Beyrer, 2015). In one study of Appalachian Kentucky injection drug users, fewer than 4% reported regularly purchasing clean syringes from pharmacies (Havens et al., 2013), highlighting the low rates of access or use of clean needles. An ongoing challenge for syringe exchange programs is the discrepancy between empirical evidence showing that increased access to clean needles decreases spread of disease (Gibson, Flynn, & Perales, 2001; Lurie et al., 1993; Watters, Estilo, Clark, & Lorvick, 1994), and decisions by sociopolitical policy makers, who make claims about community detriment without research-backing (Allen, Ruiz, & O’Rourke, 2015). Perhaps the buy-in of local opinion leaders may increase the likelihood of success for syringe exchange programs and aid in their implementation in rural Appalachia (Vestal, 2016).
The opportunities for meaningful public health initiatives in Central Appalachia are vast. Areas for public health interventions include the adoption of public health models, such as lay health providers and participatory development, to promote community engagement and sustainability for substance use treatment. Continued movement toward integrated health care models that reduce stigma, cost, and barriers to access will reduce the burden for patients to receive specialized substance use treatment. Finally, implementation of syringe exchange programs throughout the region will help to reduce the spread of infectious diseases.
Evidence Based Treatments
In addition to public health initiatives in rural Central Appalachia, training and adoption of evidence-based treatments may provide the tools necessary to successfully treat individuals with substance use disorders. These treatments broadly fit into two, often overlapping, domains: medical and psychological. Opioid substitution therapies (OSTs) provide medicinal alternatives to opioid misuse. Methadone and buprenorphine (including Suboxone and Subutex) maintenance treatments provide safer alternatives than illicit opioids because of the much lower abuse potential (Ball & Ross, 2012; Marsch, 1998; West, O’Neal, & Graham, 2001). OSTs, sometimes in conjunction with psychological treatment, support reduced opioid use and help individuals remain abstinent from, and in treatment for, illicit opioid use (Mattick, Breen, Kimber, & Davoli, 2014). Providing access to OSTs, especially through integrated health care offices, may provide cost-effective options for more widespread treatment, especially if increased coverage through the Affordable Care Act and the Mental Health Parity and Addiction Equity Act persist (Volkow, Frieden, Hyde, & Cha, 2014).
Psychological interventions, either on their own or in combination with medicinal treatments, provide skills to promote and maintain abstinence. Innovative treatments that are appropriate for rural Central Appalachia include system-based interventions such as the Community Reinforcement Approach (CRA), a psychotherapeutic intervention that uses social, recreational, familial, and vocational reinforcers to assist clients toward recovery. CRA includes motivational enhancement, monitoring of pharmacotherapy such as OSTs, functional analysis of substance use patterns, skills training (including drug refusal, communication skills, problem solving skills, and relapse prevention), help with employment, relationship counseling, and social recreational counseling (Smith & Meyers, 1995). CRA has been used successfully to treat cocaine, opioid, and cannabis dependence (Abbott, 2009; Abbott, Moore, Weller, & Delaney, 1998; Bickel, Amass, Higgins, Badger, & Esch, 1997; Budney & Higgins, 1994; McGarvey et al., 2014; Roozen, Kerkhof, & Van den Brink, 2003; Schottenfeld, Pantalon, Chawarski, & Pakes, 2000; Smith, Meyers, & Miller, 2001) and, in combination with OSTs, it is associated with a reduction in opioid use, reduction in other drug use, improvements in legal status, improvement in employment status, and improvement in social functioning (Abbott, 2009; Abbott et al., 1998; Roozen et al., 2003).
Importantly, CRA leverages strengths of the rural Appalachian identity, such as a deep-seated connection to extended family, by including family members in the treatment process to help facilitate exposure to prosocial reinforcers. It is especially well-suited for the rural Appalachian environment, as many components of the treatment are adaptable to be administered through telehealth technologies and by lay health providers, increasing treatment feasibility in the region and reducing costs over time. An important note is that implementation of psychological treatments is often expensive, even with expanding health care coverage, and may require substantial initial investment from government agencies, such as through dissemination and implementation initiatives through National Institutes for Health, grant funding mechanisms through the Substance Abuse and Mental Health Services Administration (SAMHSA), as well as other grant funding mechanisms.
Telehealth Interventions
In combination with the implementation of medical (e.g., OSTs) and psychological (e.g., CRA) services, telehealth interventions provide the opportunity to reduce cost while still expanding the provision of evidence-based medical and psychological treatments (Backhaus et al., 2012; Graham, 1996; Perle & Nierenberg, 2013). In randomized clinical trials, telehealth interventions are as effective as face-to-face interventions and can be combined with empirically supported substance use treatments (Gros et al., 2013; King, Brooner, Peirce, Kolodner, & Kidorf, 2014; Richardson, Frueh, Grubaugh, Egede, & Elhai, 2009). Importantly, telehealth strategies are increasingly feasible where legislation for equitable reimbursement of telehealth services is available, such as in Virginia and Kentucky (West Virginia Center on Budget & Policy, 2013). Additionally, the reach of technology has grown and the spread of computer and cellular access makes the use of telehealth interventions increasingly feasible, though portions of Central Appalachia have disparate access compared to national averages and compared to other regions of Appalachia (Lawrence, Oliver, Hogan, & VanLear, 2015). Despite access challenges, a local leader in telehealth services in Appalachia, Cherokee Health Services, has successfully implemented telehealth systems in collaboration with school systems to reach rural adolescents in need of physical and mental health screening (Franko, 2014).
In addition to established evidence-based treatments and telehealth strategies, promising interventions are being developed to increase treatment availability in rural areas. One example is computerized treatments for opioid dependence, such as the Therapeutic Education System, which provide module- and skills-based cognitive-behavioral treatment anywhere with computer access (Bickel, Marsch, Buchhalter, & Badger, 2008). In combination with OSTs, the Therapeutic Education System is an empirically-supported treatment for opioid use disorder (Campbell et al., 2014) that can provide services to areas where a specialized treatment provider may be unavailable. Similarly, remotely delivered contingency management, or incentive-based treatment to promote abstinence, is currently an area of development with potential to provide efficacious and cost effective treatment regardless of proximity to a health care provider. Contingency management, when delivered remotely, allows individuals to submit biological samples, such as breath alcohol levels, from home. Although not yet studied in opioid using populations, remote contingency management treatment is effective for smoking cessation (Dallery & Raiff, 2011) and is currently under evaluation for alcohol use disorder (Koffarnus, Kablinger, Swallow, & Bickel, 2015).
Conclusions
Nonmedical prescription drug use has increased over the past two decades in Central Appalachia (CDC, 2011; Havens et al., 2007) and prescription opioid abuse has come to the forefront as a public health concern. The burden of nonmedical opioid abuse in rural Appalachia extends beyond the individual drug users as it tears away at traditionally close-knit families, reduces the viable workforce, increases crime, overloads the justice system, and spreads disease through the region (CDC, 2011; Leukefeld et al., 2005). A call to action by state and federal leaders in Central Appalachia, taking the form of political endorsements of taxes on opioids (Merica, 2016) and local leaders stating the need for more funding and resources (Vilsack & McAuliffe, 2016) has brought the opioid problem to the public’s attention.
Successful large-scale interventions in Central Appalachia, like those in other rural areas, require capitalizing on local values to increase treatment seeking, acceptability, and fidelity. Participatory development models to implement lay health providers as a first line of care coupled with widespread use of telehealth to provide access to rural regions and to increase availability of highly trained professionals will improve substance use treatment. Empirically-based medical and psychological interventions such as OSTs, the Community Reinforcement Approach, the Therapeutic Education System, and remote contingency management offer candidate treatments that are well suited for the region. Furthermore, harm reduction techniques such as syringe exchange programs are necessary to curb pending epidemics of blood-borne diseases. Together, treatment efforts, with the support of funding initiatives in Central Appalachia, may pave the way for similar models in other rural areas struggling with comparable mental health and substance use problems.
References
- Abbott PJ. A review of the community reinforcement approach in the treatment of opioid dependence. Journal of Psychoactive Drugs. 2009;41(4):379–385. doi: 10.1080/02791072.2009.10399776. [DOI] [PubMed] [Google Scholar]
- Abbott PJ, Moore BA, Weller SB, Delaney HD. AIDS risk behavior in opioid dependent patients treated with community reinforcement approach and relationships with psychiatric disorders. Journal of Addictive Diseases. 1998;17(4):33–48. doi: 10.1300/J069v17n04_04. [DOI] [PubMed] [Google Scholar]
- Algeo K. Locals on local color: Imagining identity in Appalachia. Southern Cultures. 2003;4(4):27–54. [Google Scholar]
- Allen ST, Ruiz MS, O’Rourke A. The evidence does not speak for itself: The role of research evidence in shaping policy change for the implementation of publicly funded syringe exchange programs in three US cities. International Journal of Drug Policy. 2015;26(7):688–695. doi: 10.1016/j.drugpo.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appalachian Regional Commission. Graph illustration of the Appalachian region. 2013 Retrieved August 8, 2016, from https://www.arc.gov/appalachian_region/TheAppalachianRegion.asp.
- Backhaus A, Agha Z, Maglione ML, Repp A, Ross B, Zuest D, … Thorp SR. Videoconferencing psychotherapy: A systematic review. Psychological Services. 2012;9(2):111–131. doi: 10.1037/a0027924. [DOI] [PubMed] [Google Scholar]
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment: Patients, programs, services, and outcome. New York: Springer-Verlag; 2012. [Google Scholar]
- Bates AA. White opium, black coal, and the Appalachian revolution. Appalachian Heritage. 2008;36(2):56–59. [Google Scholar]
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding behavioral treatment to opioid detoxification with buprenorphine. Journal of Consulting and Clinical Psychology. 1997;65(5):803–810. doi: 10.1037//0022-006x.65.5.803. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: A randomized controlled trial. Experimental and Clinical Psychopharmacology. 2008;16(2):132–143. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings DB, Norman G, Ledford K, editors. Back talk from Appalachia: Confronting stereotypes. Lexinton, KY: University Press of Kentucky; 2000. [Google Scholar]
- Budney A, Higgins ST. A community reinforcement plus vouchers approach: Treating cocaine addiction. Rockville, Maryland: National Institute on Drug Abuse; 1994. [Google Scholar]
- Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. American Journal of Public Health. 2016;106(8):1463–1469. doi: 10.2105/AJPH.2016.303212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell AN, Nunes EV, Matthews AG, Stitzer M, Miele GM, Polsky D, … Ghitza UE. Internet-delivered treatment for substance abuse: A multisite randomized controlled trial. American Journal of Psychiatry. 2014;171(6):683–690. doi: 10.1176/appi.ajp.2014.13081055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Overdoses of prescription opioid pain relievers--United States, 1999–2008. Morbidity and Mortality Weekly Report. 2011;60(43):1487–1492. Retrieved from www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Drug Overdose Data. 2015 Retrived October 8, 2016, from www.cdc.gov/drugoverdose/data/statedeaths.html.
- Coalition on Appalachian Substance Abuse Policy. 2016 Dec 1; Retrieved from cdar.uky.edu/casap/overview.html.
- Courtemanche C, Martin J, Ukert B, Yelowitz A, Zapata D. National Bureau of Economic Research. 2016. Impacts of the Affordable Care Act on health insurance coverage in Medicaid expansion and non-expansion states (No. w22182) [DOI] [PubMed] [Google Scholar]
- Coyne CA, Demian-Popescu C, Friend D. Social and cultural factors influencing health in southern West Virginia: A qualitative study. Preventing Chronic Disease. 2006;3(4):1–8. [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Raiff BR. Contingency management in the 21st century: Technological innovations to promote smoking cessation. Substance Use and Misuse. 2011;46(1):10–22. doi: 10.3109/10826084.2011.521067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmedt M, Vertriest S, Hellings J, Bergs J, Dessers E, Vankrunkelsven P, … Vandijck D. Economic impact of integrated care models for patients with chronic diseases: A systematic review. Value in Health. 2016;19(6):892–902. doi: 10.1016/j.jval.2016.05.001. [DOI] [PubMed] [Google Scholar]
- Dotson JW, Roll JM, Packer RR, Lewis JM, McPherson S, Howell D. Urban and rural utilization of evidence-based practices for substance use and mental health disorders. Journal of Rural Health. 2014;30(3):292–299. doi: 10.1111/jrh.12068. [DOI] [PubMed] [Google Scholar]
- Drug firms shipping painkillers into Appalachia, closing pill mills not helping. 2016 Dec 1; Retrieved from http://www.kyforward.com/rural-blog-drug-firms-shipping-painkillers-into-appalachia-closing-pill-mills-not-helping/
- Eng E, Young R. Lay health advisors as community change agents. Family and Community Health. 1992;15(1):24–40. [Google Scholar]
- Franko B. Blending primary care and behavioral health: An ideal model for the diverse cultures of Appalachia. In: Welch W, editor. Public health in Appalachia: Essays from the clinic and the field. Jefferson, NC: McFarland and Company; 2014. pp. 81–104. [Google Scholar]
- Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15(11):1329–1341. doi: 10.1097/00002030-200107270-00002. [DOI] [PubMed] [Google Scholar]
- Graham MA. Telepsychiatry in Appalachia. American Behavioral Scientist. 1996;39(5):602–615. [Google Scholar]
- Gros DF, Morland LA, Greene CJ, Acierno R, Strachan M, Egede LE, … Frueh BC. Delivery of evidence-based psychotherapy via video telehealth. Journal of Psychopathology and Behavioral Assessment. 2013;35(4):506–521. [Google Scholar]
- Halverson JA, Friedell GH, Cantrell ES, Behringer BA. Health care systems. In: Ludke RL, Obermiller PJ, editors. Appalachian health and well-being. Lexington, KY: University Press of Kentucky; 2012. pp. 89–110. [Google Scholar]
- Hansen MM, Resick LK. Health beliefs, health care, and rural Appalachian subcultures from an ethnographic perspective. Family and Community Health. 1990;13(1):1–10. [Google Scholar]
- Havens JR, Lofwall MR, Frost SDW, Oser CB, Leukefeld CG, Crosby RA. Individual and network factors associated with prevalent Hepatitis C infection among rural Appalachian injection drug users. American Journal of Public Health. 2013;103(1):e44–e52. doi: 10.2105/AJPH.2012.300874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens JR, Walker R, Leukefeld CG. Prevalence of opioid analgesic injection among rural nonmedical opioid analgesic users. Drug and Alcohol Dependence. 2007;87(1):98–102. doi: 10.1016/j.drugalcdep.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Hendryx M. Mental health professional shortage areas in rural Appalachia. Journal of Rural Health. 2008;24(2):179–182. doi: 10.1111/j.1748-0361.2008.00155.x. [DOI] [PubMed] [Google Scholar]
- Housing Assistance Council. Taking stock: Rural people, poverty, and housing in the 21st century. 2010 Retrieved from http://www.ruraldataportal.org/docs/hac_taking-stock-regions.pdf.
- Hsiung DC. Two worlds in the Tennessee mountains: Exploring the origins of Appalachian stereotypes. Lexington, KY: University Press of Kentucky; 2015. [Google Scholar]
- Hyshka E, Strathdee S, Wood E, Kerr T. Needle exchange and the HIV epidemic in Vancouver: Lessons learned from 15 years of research. International Journal of Drug Policy. 2012;23(4):261–270. doi: 10.1016/j.drugpo.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indiana State Department of Health. Indiana State Department of Health investigates additional HIV cases tied to southeastern Indiana outbreak. 2015 [news release]. Retrieved from http://www.in.gov/isdh/files/August_28_ISDH__Investigates_Additional_HIV_Cases_Tied_To_Southeastern_Indiana_Outbreak.pdf.
- Jonas AB, Young AM, Oser CB, Leukefeld CG, Havens JR. OxyContin® as currency: OxyContin® use and increased social capital among rural Appalachian drug users. Social Science and Medicine. 2012;74(10):1602–1609. doi: 10.1016/j.socscimed.2011.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Status of state action on the Medicaid explansion decision. 2016 Dec 1; Retrived from kff.org/helth-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0.
- Keefe S. Participatory development in Appalachia: Cultural identity, community, and sustainability. Knoxville, TN: University of Tennessee Press; 2009. [Google Scholar]
- King VL, Brooner RK, Pierce JM, Kolodner K, Kidorf MS. A randomized trial of web-based videoconferencing for substance abuse counseling. Journal of Substance Abuse Treatment. 2014;46(1):36–42. doi: 10.1016/j.jsat.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak SE. OxyContin flood in the coalfields: Searching for higher ground. In: Fisher SL, Smith BE, editors. Transforming places: Lessons from Appalachia. Chicago, IL: University of Illinois Press; 2012. pp. 198–209. [Google Scholar]
- Kobak SE. When OxyContin struck, and how the community struck back: One woman remembers. In: Welch W, editor. Public health in Appalachia: Essays from the clinic and the field. Jefferson, NC: McFarland & Company; 2014. pp. 65–80. [Google Scholar]
- Koffarnus MN, Kablinger AS, Swallow AE, Bickel WK. Remote alcohol monitoring to facilitate abstinence reinforcement: Preliminary data. Alcoholism-Clinical and Experimental Research. 2015;39:204A–204A. doi: 10.1111/acer.13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane N, Konrad R, Ricketts T. Health care costs and access disparities in Apppalachia. Washington, DC: Appalachian Regional Commission; 2012. [Google Scholar]
- Lawrence S, Oliver Z, Hogan M, VanLear S, Baller J, Horrigan J, … Watts D. Program evaluation of the Appalachian Regional Commision’s telecommunications and technology projects: FY2004-FY2010. 2015 Nov; Retrived from https://www.arc.gov/research/researchreportdetails.asp?REPORT_ID=120.
- Leukefeld C, McDonald HS, Mateyoke-Scrivner A, Roberto H, Walker R, Webster M, Garrity T. Prescription drug use, health services utilization, and health problems in rural Appalachian Kentucky. Journal of Drug Issues. 2005;35(3):631–643. [Google Scholar]
- Leukefeld C, Walker R, Havens J, Leedham CA, Tolbert V. What does the community say: Key informant perceptions of rural prescription drug use. Journal of Drug Issues. 2007;37(3):503–524. [Google Scholar]
- Lurie P, Reingold AL, Bowser B, Chen D, Foley J, Guydish J, … Sorensen J. The public health impact of needle exchange programs in the United States and abroad: Summary, conclusions and recommendations. Atlanta: Centers for Disease Control and Prevention; 1993. [Google Scholar]
- Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: A meta-analysis. Addiction. 1998;93(4):515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Systematic Reviews. 2014;2(2):1–84. [Google Scholar]
- McGarvey EL, Leon-Verdin M, Bloomfield K, Wood S, Winters E, Smith J. Effectiveness of A-CRA/ACC in treating adolescents with cannabis use disorders. Community Mental Health Journal. 2014;50(2):150–157. doi: 10.1007/s10597-012-9566-2. [DOI] [PubMed] [Google Scholar]
- Merica D. Clinton backs Manchin plan to tax opioids. CNN. 2016 Jul 7; Retrieved from http://www.cnn.com/2016/05/03/politics/hillary-clinton-west-virginia-opioids/
- Perle JG, Nierenberg B. How psychological telehealth can alleviate society’s mental health burden: A literature review. Journal of Technology in Human Services. 2013;31(1):22–41. [Google Scholar]
- Prokopy J, Castelloe P. Participatory development: Approaches from the global south and the United States. Community Development. 1999;30(2):213–231. [Google Scholar]
- Reschovsky JD, Staiti AB. Access and quality: Does rural America lag behind? Health Affairs. 2005;24(4):1128–1139. doi: 10.1377/hlthaff.24.4.1128. [DOI] [PubMed] [Google Scholar]
- Richardson LK, Frueh C, Grubaugh B, Anouk L, Egede L, Elhai JD. Current directions in videoconferencing tele-mental health research. Clinical Psychology: Science and Practice. 2009;16(3):323–338. doi: 10.1111/j.1468-2850.2009.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozen HG, Kerkhof AJ, Van den Brink W. Experiences with an outpatient relapse program (community reinforcement approach) combined with naltrexone in the treatment of opioid-dependence: Effect on addictive behaviors and the predictive value of psychiatric comorbidity. European Addiction Research. 2003;9(2):53–58. doi: 10.1159/000068808. [DOI] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths-United States, 2000–2014. Morbidity and Mortality Weekly Report. 2016;64(50–51):1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Schoeneberger ML, Leukefeld CG, Hiller ML, Godlaski T. Substance abuse among rural and very rural drug users at treatment entry. American Journal of Drug and Alcohol Abuse. 2006;32(1):87–110. doi: 10.1080/00952990500328687. [DOI] [PubMed] [Google Scholar]
- Schottenfeld RS, Pantalon MV, Chawarski MC, Pakes J. Community reinforcement approach for combined opioid and cocaine dependence: Patterns of engagement in alternate activities. Journal of Substance Abuse Treatment. 2000;18(3):255–261. doi: 10.1016/s0740-5472(99)00062-8. [DOI] [PubMed] [Google Scholar]
- Scott R. Removing mountain: Extracting nature and identity in the Appalachian coalfields. Minneapolis, MN: University of Minnesota Press; 2010. Hillbillies and coal miners: Representations of a national sacrifice zone; pp. 31–64. [Google Scholar]
- Smith JE, Meyers RJ. The community reinforcement approach. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches: Effective alternatives. 2. Needham Heights, MA: Allyn & Bacon; 1995. pp. 251–266. [Google Scholar]
- Smith JE, Meyers RJ, Miller WR. The community reinforcement approach to the treatment of substance use disorders. American Journal on Addictions. 2001;10:s51–s59. doi: 10.1080/10550490150504137. [DOI] [PubMed] [Google Scholar]
- State Health Reform Assistance Network. Medicaid expansion: Just the facts. 2016 Retrieved from http://statenetwork.org/resource/medicaid-expansion-just-the-facts/
- Steele E. The impact of mountaintop coal removal on adolescent and young adult risk behaviors in rural, urban, and Appalachian areas of Kentucky. Doctoral Dissertation. 2015 Retrieved from http://libres.uncg.edu/ir/asu/f/Steele%20Thesis.docx.pdf.
- Strathdee SA, Beyrer C. Threading the needle—How to stop the HIV outbreak in rural Indiana. New England Journal of Medicine. 2015;373:397–399. doi: 10.1056/NEJMp1507252. [DOI] [PubMed] [Google Scholar]
- Van Handel MM, Rose CE, Hallisey EJ, Kolling JL, Zibbell JE, Lewis B, … Brooks JT. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. Journal of Acquired Immune Deficiency Syndromes. 2016;73(3):323–331. doi: 10.1097/QAI.0000000000001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Zee A, Kobak SE. OxyContin in the coal fields---Still searching for “higher ground” fifteen years later. Workshop presentation at the Appalachian Studies Association annual conference; Johnson City, TN. 2015. Mar, [Google Scholar]
- Vestal C. Early results in W.V. town’s needle exchange program show progress. 2016 Retrieved 07/07/2016, 2016, from http://www.pbs.org/newshour/rundown/early-results-of-w-va-towns-needle-exchange-program-shows-progress/
- Vilsack T, McAuliffe T. More resources needed to battle the opioid epidemic in Appalachia. Roanoke Times. 2016 Retrieved from http://www.roanoke.com/opinion/commentary/vilsack-and-mcauliffe-more-resources-needed-to-battle-the-opioid/article_a17bac24-ee8c-5390-82a0-1190cba70690.html.
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—Tackling the opioid-overdose epidemic. New England Journal of Medicine. 2014;370(22):2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Watson J. Free clinics and the uninsured: The need for remote area medical in Central Appalachia after health reform. Doctoral Dissertation. 2011 Retrieved from http://dc.etsu.edu/cgi/viewcontent.cgi?article=2549&context=etd.
- Watters JK, Estilo MJ, Clark GL, Lorvick J. Syringe and needle exchange as HIV/AIDS prevention for injection drug users. Journal of the American Medical Association. 1994;271(2):115–120. [PubMed] [Google Scholar]
- West SL, O’Neal KK, Graham CW. A meta-analysis comparing the effectiveness of buprenorphine and methadone. Journal of Substance Abuse. 2001;12(4):405–414. doi: 10.1016/s0899-3289(01)00054-2. [DOI] [PubMed] [Google Scholar]
- West Virginia Center on Budget & Policy. Ensuring broadband access in Appalachia. 2013 Retrieved from http://www.wvpolicy.org/wp-content/uploads/2013/04/CARN-broadband-report.pdf.
- Wewers ME, Shoben A, Contry S, Curry E, Ferketich AK, Murray DM, … Wermert A. Effectiveness of two community health worker models of tobacco dependence treatment among community residents of Ohio Appalachia. Nicotine & Tobacco Research. 2016 doi: 10.1093/ntr/ntw265. https://doi.org/10.1093/ntr/ntw265. [DOI] [PMC free article] [PubMed]
- Witters D. Arkansas, Kentucky Set Pace in Reducing Uninsured Rate. 2016 Retrieved 07/07/2016, 2016, from http://www.gallup.com/poll/189023/arkansas-kentucky-set-pace-reducing-uninsured-rate.aspx.
- Young AM, Havens JR. Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: A cross-sectional comparison and retrospective survival analysis. Addiction. 2012;107(3):587–596. doi: 10.1111/j.1360-0443.2011.03635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Infante A, Meit M, English N, Dunn M, Bowers K. An analysis of mental health and substance abuse disparities and access to treatment services in the Appalachian region. 2008 Aug; Retrieved from https://www.arc.gov/research/researchreportdetails.asp?REPORT_ID=71.
- Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, … Holtzman D. Increases in Hepatitis C virus infection related to injection drug use among persons aged≤ 30 years-Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. Morbidity and Mortality Weekly Report. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- Zuvekas A, Nolan L, Tumaylle C, Griffin L. Impact of community health workers on access, use of services, and patient knowledge and behavior. Journal of Ambulatory Care Management. 1999;22(4):33–44. doi: 10.1097/00004479-199910000-00007. [DOI] [PubMed] [Google Scholar]