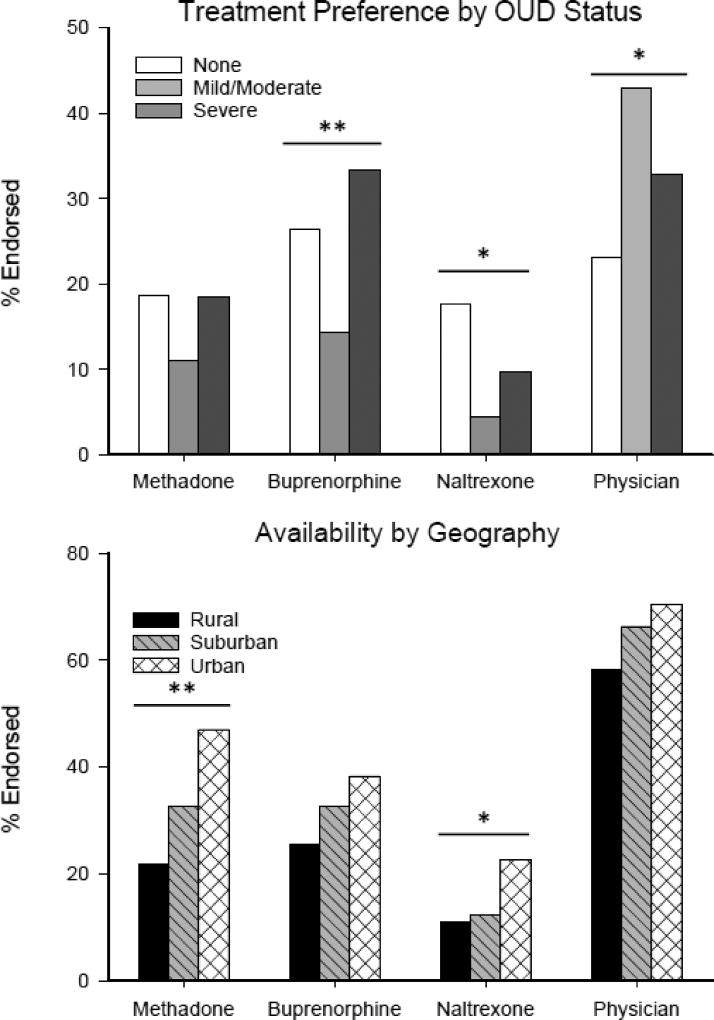
Figure 1.
(Top) The preference for MATs and physician visits (without expressed purpose of MAT) was examined based on self-reported opioid use severity. Mild and moderate OUD was combined to balance group size. This led to three groups including no OUD (0–1 symptoms; n=91), mild/moderate OUD (2–5 symptoms, n=91), and severe OUD (6+ symptoms; n=174). Participants with severe OUD were more likely to endorse buprenorphine as a preferred treatment option when compared to participants with no-OUD or mild/moderate OUD (χ2(2)=11.09, p=.004). In addition, participants with no-OUD and severe OUD were more likely to endorse oral/XR naltrexone as a preferred treatment option relative to participants with mild/moderate OUD (χ2(2)=8.64, p=.013). There were no group differences in preference for methadone. Participants with mild/moderate and severe OUD were more likely to endorse preference for a physician visit as a treatment option compared to participants with no-OUD (χ2(2)=8.07, p=.018). (Bottom) Participants rated the perceived availability of methadone (χ2(2)=11.75, p=.003) and naltrexone (χ2(2) =6.82, p=.033) as less available in rural and suburban areas compared to urban areas; buprenorphine did not display a significant difference in perceived availability. *=p<.05; **=p<.01.