Figure 1. Neurological consequences of obesity: an overview.
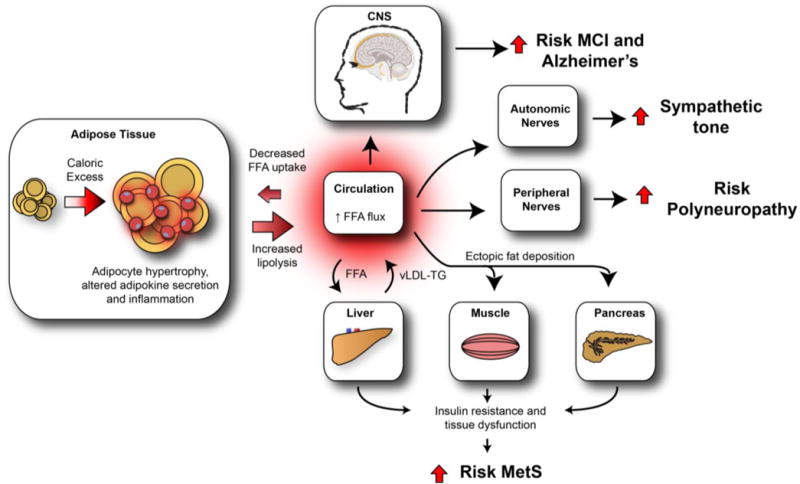
Increased caloric intake and decreased energy expenditure result in a net energy overload, leading to adipose tissue expansion (hyperplasia and hypertrophy). Sustained caloric excess in visceral adipose tissue activates resident adipose tissue macrophages, contributing to the development of adipose tissue dysfunction and metabolic inflammation. As a consequence, circulating FFAs rise, are lipotoxic to peripheral tissues, and contribute to the development of metabolic dyshomeostasis. High FFA flux into the liver increases vLDL-triglyceride production, further promoting dyslipidemia, while ectopic fat deposition in the muscle and pancreas promotes insulin resistance and pancreatic β-cell dysfunction, respectively. Collectively, these impairments lead to the MetS. Similarly, the CNS, ANS, and PNS are also detrimentally affected by obesity and obesity-induced metabolic dysfunction, which we hypothesize is driven by the lipotoxic effects of dyslipidemia and increased circulating FFA. In the CNS, dysfunction leads to MCI and Alzheimer’s disease while in the ANS and PNS, the end result is autonomic and peripheral neuropathy, respectively. FFA = free fatty acid. vLDL = very-low-density lipoprotein. TG = triglyceride. MCI = mild cognitive impairment. MetS = metabolic syndrome.
