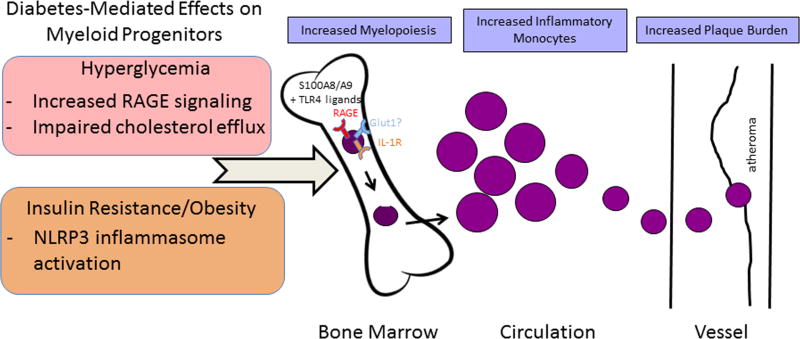
Figure 2.
Diabetes-mediated effects on myeloid progenitors and their consequences. In the setting of hyperglycemia, plasma levels of S100A8/A9 increase. In the bone marrow, this provides more S100A8/A9 to interact with RAGE on the surface of macrophages and common myeloid progenitors (CMPs), triggering the production of M-CSF and GM-CSF and increasing CMP and granulocyte–macrophage progenitors (GMPs). This subsequently accelerates the production of monocytes and neutrophils. In the setting of obesity and insulin resistance, S100A8/A9 interacts with TLR4 on adipose tissue macrophages and induces IL-1β production. Mature IL-1β then travels to the bone marrow and binds the IL-1 receptor on CMPs and GMPs, stimulating myelopoiesis. Both pathways result in the circulation of inflammation-prone monocytes (in mice, the Ly6-Chi subset), which enter the plaque in greater numbers and become macrophages. The glucose transporter GLUT1 may be a novel regulator of myelopoiesis in the diabetic state via reducing glucose utilization by hematopoietic stem and progenitor cells, thereby suppressing their proliferation and differentiation.