Figure 5. Mechanisms Through Which Cardiovascular Risk Factors Mediate Atherogenesis and Available Pharmacological Tools for Targeting Crucial Pathogenic Factors.
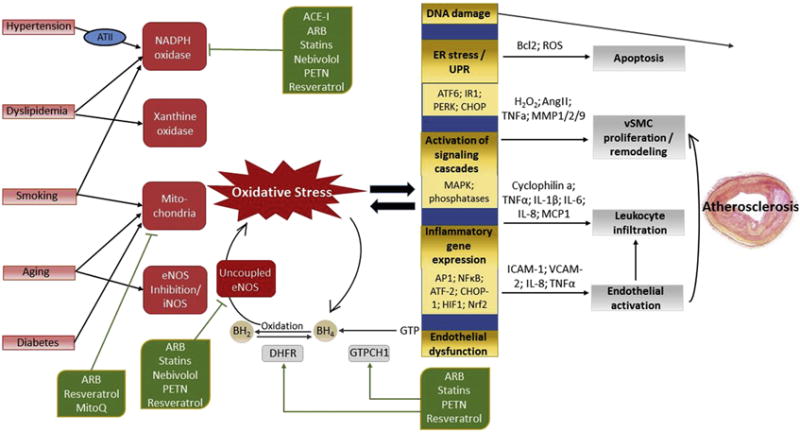
Cardiovascular risk factors promote oxidative stress by stimulation of various pro-oxidant enzyme systems, tipping the redox balance in favor of oxidation, with O2− as the key mediator. Hypertension activates NADPH oxidase via angiotensin II (ATII) and angiotensin 1 receptor (AT1R) signaling. The main ROS sources in states of hypercholesterolemia are NADPH oxidase and xanthine oxidase (activated by oxidized low-density lipoprotein), and the hypercholesterolemia-mediated up-regulation of AT1R. Hyperglycemia, as seen in diabetes, associates primarily with mitochondrial ROS production, which can secondarily activate NADPH oxidase. Compounds contained in cigarette smoke activate NADPH oxidase, which mediates mitochondrial dysfunction and thus ROS production. Aging is associated with increased mitochondrial dysfunction and reduced eNOS activity. Superoxide from all sources can inactivate vasoprotective NO by its reaction to ONOO−, which, in turn, mediates uncoupling of eNOS-mediated oxygen reduction and NO− production by oxidation of the essential cofactor tetrahydrobiopterin (BH4).
The enzymes dihydrofolate reductase (DHFR) and GTPCH1 counteract eNOS uncoupling by replenishing BH4 levels via regeneration and de novo synthesis, respectively. ATII decreases BH4 levels, not only by activating NADPH oxidase, but also by down-regulation of DHFR. NADPH oxidase has been seen to be inhibited by angiotensin-converting enzyme inhibitors (ACEIs), ATII receptor type 1 blockers (ARBs), 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins), the β-blocker nebivolol, the plant-derived polyphenol resveratrol, and the organic nitrate pentaerithrityl tetranitrate (PETN). The same compounds inhibit eNOS uncoupling by activating GTPCH1 and DHFR. Mitochondrial O2− generation is decreased by ARBs, MitoQ and resveratrol. Other abbreviations as in Figures 1 and 3.
