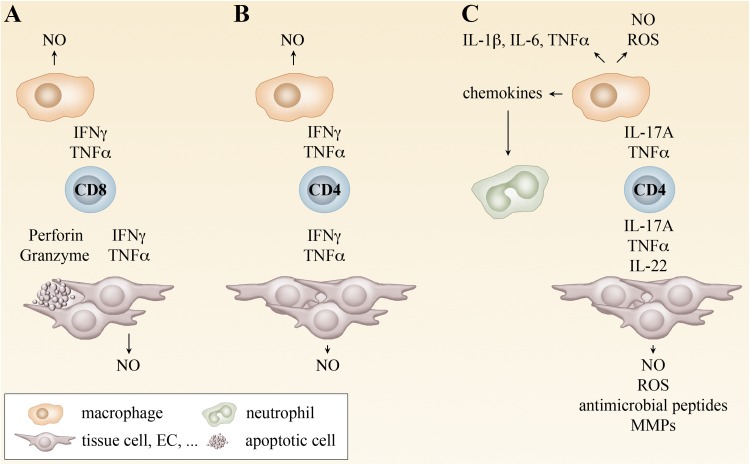
Fig. 2.
Mechanisms of T cell-mediated protection. CD8+ T cells differentiate in the infection with rickettsiae to cytotoxic T cells that induce apoptosis in infected cells via the release of perforin and granzymes. In addition, CD8+ T cells produce IFNγ and TNFα. These cytokines induce the production of NO by MΦ and other cells and, thus, enable bacterial killing. The release of cytokines by CD8+ T cells is sufficient for protection at least in the infection with some rickettsial species such as R. typhi where the cytotoxic activity is not essential for bacterial defense (a). CD4+ T cells usually differentiate into TH1 cells that produce IFNγ and TNFα in the infection with rickettsiae. TH1 cells are protective by the induction of NO and bacterial killing by MΦ and other cells (b). In the absence of IFNγ, CD4+ T cells develop into TH17 cells in the infection with rickettsiae. These cells release IL-17A, IL-22 and TNFα. IL-17A and TNFα synergistically induce the production of NO und ROS by MΦ and other cells. In addition, these cytokines induce the release of proinflammatory cytokines. IL-17A further induces the production of chemokines, leading to the recruitment of neutrophils that contribute to local inflammation. IL-22 does not act on immune cells but various tissue cells. IL-22 induces the release of antimicrobial peptides and other factors and can contribute in this way to bacterial elimination. At least in the infection with R. typhi TH17 cells can be protective. However, the combined release of TNFα and IL-17A is non-beneficial and exerts pathological effects. Inhibition of either TNFα or IL-17A in this situation renders TH17 cells as protective as TH1 cells (c)