Abstract
BACKGROUND
Older adults that transfer from skilled nursing facilities (SNF) to home have significant risk for poor outcomes. Transitional care of SNF patients (i.e., time-limited services to ensure coordination and continuity of care) is poorly understood.
OBJECTIVE
To determine the feasibility and relevance of the Connect-Home transitional care intervention, and to compare preparedness for discharge between comparison and intervention dyads.
DESIGN
A non-randomized, historically controlled design enrolling dyads of SNF patients and their family caregivers.
SETTING
Three SNFs in the Southeastern United States.
PARTICIPANTS
Intervention dyads received Connect-Home; comparison dyads received usual discharge planning. Of 173 recruited dyads, 145 transferred to home, and 133 completed surveys within 3 days of discharge.
INTERVENTION
The Connect-Home intervention consisted of tools and training for existing SNF staff to deliver transitional care of patient and caregiver dyads.
MEASUREMENT
Feasibility was assessed with a chart review. Relevance was assessed with a survey of staff experiences using the intervention. Preparedness for discharge, the primary outcome, was assessed with Care Transitions Measure-15 (CTM-15).
RESULTS
The intervention was feasible and relevant to SNF staff (i.e., 96.9% of staff recommended intervention use in the future). Intervention dyads, compared to comparison dyads, were more prepared for discharge (CTM-15 score 74.7 vs. 65.3, Mean Ratio 1.16, 95% CI: 1.08, 1.24).
CONCLUSION
Connect-Home is a promising transitional care intervention for older patients discharged from SNF care. The next step will be to test the intervention using a cluster randomized trial, with patient outcomes including rehospitalization.
Keywords: Transitional care, skilled nursing facilities, quasi-experimental clinical trial
Introduction
Older Americans who complete care in hospitals, use Medicare benefits for rehabilitation in skilled nursing facilities (SNF), and subsequently transfer home are an especially vulnerable group. More than 70% of these patients are aged 75 years or older, 49% are dependent on others for at least three activities of daily living, and 37% are eligible for Medicare and Medicaid.1 Moreover, this patient group frequently relies on spouses and children for intensive caregiving following their transition from SNF to home.2,3 Within 30 days of discharge from SNFs, one in five of these patients use emergency services or are re-hospitalized.4,5
Current practice in SNFs is for existing professional staff to provide “discharge planning” services for patients transitioning to their homes. These services are highly variable in content and quality, often lack key staff or caregiver input, and frequently occur in only the last few days of the SNF stay.6,7 Payment models do not compensate SNFs for time spent on discharge planning and do not yet provide incentives to improve post-SNF outcomes. Consequently, patients and their family caregivers (defined as relatives, friends or neighbors and hereafter referred to as caregivers) are often unprepared to manage their health care after discharge.8–10
One way to improve outcomes may be to improve transitional care, defined as time-limited services designed to ensure health care continuity, avoid preventable poor outcomes, and promote the safe and timely transfer of patients.11,12 Evidence from trials of hospital-based interventions indicate that older adults who received transitional care, compared to usual care, were more prepared and less frequently re-hospitalized after returning home.13 We adapted successful elements of two evidence-based transitional care models (Project RED and the Transitional Care Model) and a model of organizational change in nursing homes (CONNECT for Preventing Falls) and developed “Connect-Home,” a team-based transitional care intervention for SNF patients and their caregivers using existing nursing home staff.15–17 This study was designed to determine the feasibility and relevance of Connect-Home (Aim 1) and to compare preparedness for discharge between controls and intervention dyads (Aim 2).
Methods
Design
This pilot study used a non-randomized, historically controlled design enrolling dyads of patients and their caregivers in 3 SNFs. First, the quality of transitional care was assessed for comparison dyads who received usual care. After a three to four week intervention period, the quality of transitional care was assessed for intervention dyads who received Connect-Home services. The intervention (described in detail below) consisted of support for existing SNF staff to provide transitional care of SNF patient and caregiver dyads. Feasibility and relevance were measured using data abstracted from medical records and data from surveys with SNF staff. Preparedness for discharge was measured using the Care Transitions Measure-15 (CTM-15).18 The Internal Review Board at the BLINDED approved all study procedures.
Setting, Subjects and Recruitment
Connect-Home was pilot tested in SNFs owned and operated by a not-for-profit nursing home chain in BLINDED. Each study site had occupancy of greater than 100 beds, an electronic medical records (EMR) system, and a SNF patient volume of at least 20 patients per month. In each SNF, we aimed to recruit 30 dyads in each of the comparison and intervention periods. To enroll dyads, a research assistant sequentially screened all newly admitted patients. Patients were eligible if they had the ability to speak English and discharged from the SNF to home (based on SNF staff assessment and hospital discharge materials). Although the goal of the sampling plan was to recruit patient and caregiver dyads, patients were included if they did not have a caregiver who could be recruited. The rationale for this decision was to mimic the situation of clinical care of patients in this population, in which a friend, family member or other responsible party is not always available or willing to participate in care. Patients were excluded if they had both more than mild cognitive impairment (based on physician documentation in hospital discharge records and/or Minimum Data Set nurse assessment of cognitive impairment) and no legally authorized representative who could be enrolled in the study. Caregivers were eligible if they assisted with the patient’s care at home and had the ability to speak English. Staff were eligible if they were involved in delivering elements of discharge planning or transitional care. Using IRB approved consenting procedures, study participants (patients, caregivers and staff) provided informed written consent to participate in all research activities; a legally authorized representative’s consent for study participation was obtained for all patients with cognitive impairment.
Usual Care
Patients and caregivers in the historical comparison phase of the study received usual discharge planning. The content of discharge planning differed across study sites and included services, such as care plan meetings, referrals to home care, instructions to schedule follow-up appointments, discharge medication lists, and written instructions about care at home.
Connect-Home Intervention
Patients and caregivers in the intervention phase of the study experienced Connect-Home (Table 1). The Connect-Home 4-step transitional care process included protocolized procedures for staff in SNFs to interact on patient care-teams to deliver transitional care. In step one, staff, patients and caregivers created a transition plan of care that was documented using a consistent template by day 15–17 of SNF stay. In step two, staff convened a care plan meeting on day 8–10 to set priorities, review plans, and educate the patient and caregiver. In step three, staff, patients and caregivers implemented the transition plan; for example, a registered nurse reconciled final medication orders and the patient’s discharge medication list, a social worker scheduled follow-up appointments and faxed medical records to community clinicians, and, on the day of discharge, a staff nurses used a written transition plan to review the complete transition plan with patients and caregivers. In step four, the social worker telephoned the patient or caregiver at home within 72 hours of discharge to review the transition plan of care and triage questions or problems. In step four, the social worker tried at least twice to reach the patient or caregiver by telephone. Staff documented Connect-Home activities related to each step in the EMR system.
Table 1.
Connect-Home: Transitional Care in Skilled Nursing Facilities
| Transitional Care in 4 Steps | |
|---|---|
| Step 1 | Complete a Transition Plan of Care (TPOC) by day 15–17 (of 20 day stay) Use the TPOC to organize rehabilitation, medical follow-up, caregiver supports, medication instructions, and other self-care activities at home. |
| Step 2 | Convene a care plan meeting by day 8–10 (of 20 day stay) Set priorities, review the TPOC, and educate the patient and primary caregiver. |
| Step 3 | Implement the transition plan by day 17 (of 20 day stay)
|
| Step 4 | Call the patient or caregiver at home within 72 hours of discharge Review the TPOC, triage medical questions, and confirm home and primary care activities. |
|
| |
| Tools, Training and Technical Assistance to Implement Connect-Home | |
|
| |
| Tools | Tools on paper and in the electronic medical record to create a TPOC and home medication list |
| Training | 4 hours of face to face training with nurses, rehabilitation therapists, social workers, and others; training includes transitional care roles and responsibilities and details the 4-step process |
| Audit | Interviews with SNF staff and patient chart audits to assess adherence to study procedures. |
| Feedback | In person dialogue with individual staff to discuss performance and identify strategies for refining implementation. |
Connect-Home was implemented using tools, training, and technical assistance for site-based SNF staff. Tools included (a) a schedule to coordinate staff delivery of the 4 steps of transitional care; (b) a template for the transition plan in the electronic medical record (EMR); and (d) the Connect-Home implementation toolkit with procedures to support staff in the SNFs. Before data collection was started in the study SNFs, a study investigator (MT) worked with an information technology specialist in the nursing home chain to install the transition plan of care template in the EMR system. Staff training was provided in each SNF separately; training consisted of four hours of face to face training, including three hours with the full team of nurses, social workers and rehabilitation therapists, and one hour with groups of staff in the same discipline. Technical assistance was provided by a study investigator (MT) during the intervention phase in each SNF; the investigator audited medical records (to assess staff adherence to study procedures) and gave verbal and structured written feedback to staff in groups and in one-to-one meetings about performance. Additional detail about Connect-Home is described in Supplementary Material S1.
Data Collection
Data collection consisted of (a) face-to-face interviews with patients in the SNF and telephone interviews with caregivers at baseline; (b) telephone interviews with patient and caregiver dyads one to three days after discharge and 30 days after discharge; (c) chart reviews of medical records after SNF discharge; and (d) in-person interviews with SNF staff during the intervention phase. Baseline interviews with patients and caregivers lasted approximately 20 minutes; follow up telephone interviews 15–20 minutes, and staff interviews 10 minutes.
To assess the feasibility of Connect-Home, an investigator reviewed patient medical records and collected data on staff adherence to study procedures. Measures of feasibility included (a) completing transition plans of care, (b) convening care plan meetings before the tenth day of the SNF admission, (c) participation of patients’ caregivers in care plan meetings, (d) scheduling follow-up medical appointments, (e) transmitting of medical records to follow-up, (f) making follow-up calls at home within 72 hours of discharge, and (g) reaching the patient or caregiver by telephone after discharge.
To assess the relevance of the intervention to SNF staff, investigators collected written responses to surveys provided anonymously by staff. Using a survey designed by the research team, relevance was measured with three 4-point Likert scaled items. Acceptability was defined as greater than 80% of SNF staff reporting the intervention was useful, not difficult to use, and should be used in the future.
Primary Outcome Measure
The primary outcome was patient and caregiver preparedness for discharge, which was assessed using the (CTM-15).18 The CTM-15 was validated in studies of hospital patients that transferred to home, but not with hospital patients that transfer to a SNF before subsequent transfers to home; it shows high reliability and is the most widely used self-report measure of preparedness for discharge.19 The CTM-15 is a survey with 15 4-point Likert scaled items; it is scored on a scale ranging from 0–100, with a higher score indicating greater preparation for discharge.19 The CTM-15 was administered by telephone one to three days after SNF discharge. Research staff attempted to contact the SNF patient first; if the patient was not reachable or requested that their caregiver respond, the researcher surveyed the caregiver.
Measures of Co-variates
Data were collected to describe baseline characteristics that potentially co-vary with preparedness for discharge, including health literacy21 and social support.22 Baseline characteristics of primary caregivers were collected, including caregiver burden23 and age, gender, relationship to patient, and days per week required to support the patient. Additional data were abstracted from the medical record, including the medical history in the index hospitalization and the SNF stay, and referral of home care after SNF stay. Paired chart abstraction was used until agreement of 85% or greater was achieved on all items, which required eight abstractions; then, a single investigator completed the chart abstraction. To explore preliminary data on more distal outcomes, we also surveyed patients and/or caregivers by telephone 30 days after transition home on hospitalization, emergency department use, overall health,24 activities of daily living disability,25 falls, and unmet needs.
Statistical Analysis
We described all dyad characteristics, as well as measures relating to feasibility, staff perceptions of the intervention, primary outcome and co-variates using means and standard deviations for continuous variables and counts and percentages for categorical variables. We tested for group differences using Wilcoxon rank-sum tests for continuous variables and chi-square tests for categorical variables. To assess the impact of the intervention on our primary outcome of CTM-15 score, we fit a linear model. To ensure that CTM-15 score satisfied the assumption of normality integral to linear models, we analyzed the log-transformed values for this score. In this model, an indicator variable for group membership (historical comparison versus intervention) was included as a predictor, while facility and an indicator variable for whether each score came from the patient or caregiver were included as covariates. In preliminary analyses, facility was first included as a random effect to account for correlation within each facility. However, since the variance of this random facility effect did not significantly differ from zero, facility was included as a covariate with a fixed effect in our final model. None of the patient or caregiver characteristics (including cognitive status and caregiver burden) were independently associated with CTM-15 score and thus were not included in the final models. Due to our log-transformation of this score, the mean ratio with respect to group membership was estimated, along with its 95% confidence interval (CI). All statistical analyses were run using SAS software version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Study Subjects
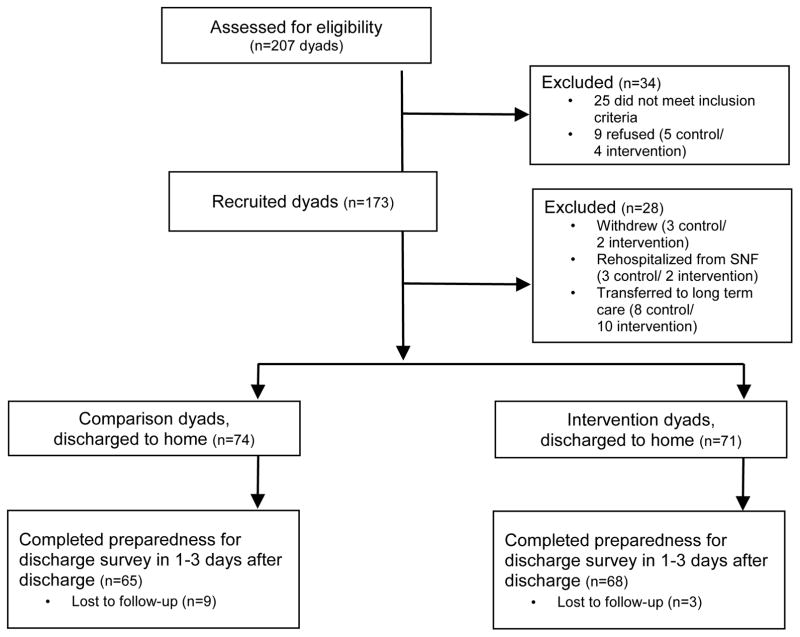
Of 207 dyads that were assessed for eligibility, 34 dyads were ineligible or refused to participate, and 173 dyads (84%) consented to participate (Figure 1), including 58 dyads in SNF 1, 58 dyads in SNF 2, and 57 dyads in SNF 3. The primary reasons dyads chose not participate were concerns about respondent burden and privacy. Of 173 recruited dyads, 28 patients withdrew before SNF discharge due to (a) patient or caregiver perceptions that participation was burdensome or (b) patient re-rehospitalization from the SNF, transfer to long term care, or death. Of 173 recruited dyads, a total of145 patients transferred to home and thus met all eligibility criteria; of these, 133 completed surveys [65 comparison (87.8%) and 68 intervention (95.8%)] in 1–3 days after SNF discharge to provide data on the primary outcome.
Figure 1.
CONSORT Diagram
On average, patients were aged 80 years and caregivers were aged 64 years; other characteristics of patients and caregivers are described in Table 2. Comparison and intervention patients shared similar demographic, psychosocial and clinical characteristics, except cognitive impairment (defined as a physician diagnosis of cognitive impairment), which was more frequently observed in the intervention group (14.9% vs. 26.8%).
Table 2.
Characteristics of patients (and caregivers) who transferred home (N = 145)1
| Variable | Scale range | Comparison (N=74) | Intervention (N=71) | p2 |
|---|---|---|---|---|
| Patient | ||||
| Mean Age (SD) | - | 79.78 (8.4) | 80.24 (8.7) | 0.52 |
| Female gender, n (%) | - | 53.00 (71.6) | 50.00 (70.4) | 0.87 |
| White race, n (%) | - | 66.00 (89.2) | 66.00 (92.9) | 0.43 |
| Primary Diagnosis | ||||
| Major joint replacement, n (%) | - | 18.00 (24.3) | 21.00 (29.6) | 0.48 |
| Hip/pelvis fracture, n (%) | - | 5.00 (6.8) | 9.00 (12.7) | 0.23 |
| Other fractures, n (%) | - | 4.00 (5.41) | 7.00 (9.9) | 0.31 |
| Back surgery, n (%) | - | 2.00 (2.70) | 6.00 (8.4) | 0.13 |
| Other diagnosis, n (%) | - | 44.00 (59.5) | 28.00 (39.4) | 0.02 |
| Mean Charlson Score (SD) | 0–36 | 6.08 (2.3) | 6.20 (2.2) | 0.50 |
| Cognitive Impairment, n (%) | - | 11.00 (14.9) | 19.00 (26.8) | 0.08 |
| Mean Hospital length of stay (days) (SD) | - | 6.93 (5.5) | 5.18 (2.8) | 0.10 |
| Mean skilled nursing facility length of stay (days) (SD) | - | 31.42 (27.8) | 25.93 (17.6) | 0.34 |
| Discharge to home, n (%) | - | 65.00 (87.8) | 62.00 (87.3) | 0.93 |
| Mean Rapid Estimate of Adult Literacy in Medicine score (SD) | 1–8 | 7.68 (0.9) | 7.18 (1.8) | 0.12 |
| Mean Social Support (SD) | 8–40 | 35.19 (6.3) | 33.72 (7.4) | 0.33 |
| Mean Activities of Daily Living Disability (SD) | 1–4 | 1.46 (1.4) | 1.90 (1.5) | 0.08 |
| Caregiver | ||||
| Mean Age (SD) | - | 63.71 (13.7) | 63.57 (13.4) | 0.80 |
| Female gender, n (%) | - | 37.00 (80.4) | 38.00 (84.4) | 0.62 |
| Relation to patient | ||||
| Spouse, n (%) | - | 19.00 (41.3) | 14.00 (31.1) | 0.79 |
| Child, n (%) | - | 18.00 (39.1) | 21.00 (46.7) | - |
| Friend or other, n (%) | - | 9.00 (19.6) | 10.00 (22.2) | - |
| Mean care days / week (SD) | - | 4.91 (2.6) | 5.09 (2.5) | 0.82 |
| Lives with patient, n (%) | - | 22.00 (47.8) | 22.00 (48.9) | 0.92 |
| Mean Zarit burden score (SD) | 1–5 | 3.07 (2.7) | 4.40 (2.8) | 0.01 |
Data are reported for patients (and their caregivers) who transferred to home
p value based on chi square tests for categorical variables and Wilcoxon rank-sum tests for continuous variables
Higher scores indicate greater comorbidity
Cognitive status was determined using physician notes in hospital and skilled nursing charts
Higher scores indicate greater health literacy
Higher scores indicated greater social support
Higher scores indicate greater disability
Higher scores indicate greater caregiver burden
Feasibility of the Intervention
Feasibility was assessed for intervention patients that transferred from SNFs to home (N=71 dyads). Across the SNFs, it was consistently feasible for staff to: complete transition plans of care (90.1%), convene care plan meetings (85.9%), schedule follow-up medical appointments (90.1%), transmit medical records to follow-up clinicians (81.7%), and make follow-up calls within 72 hours of patient discharge (75%). Making at least two attempts to call after discharge, SNF staff reached 56% of patient or caregiver dyads at home.
Relevance of the Intervention
Thirty-two SNF staff members were surveyed to assess relevance of the intervention: 27 (84.4%) reported it was “not difficult at all to use,” 26 (81.3%) reported it was “useful for preparing patients and family caregivers for transitions in care from the SNF to home,” and 31 staff (96.9%) reported that it is a “good idea to continue using Connect-Home in the future.”
Primary Outcome: The Impact of Connect-Home on Preparedness for Discharge
Preparedness for discharge was assessed for 133 of the enrolled dyads that completed CTM-15 surveys in one to three days after discharge; in 88 dyads (66%), the patient provided CTM-15 data; in the remainder, a patient’s caregiver provided data. Intervention dyads, versus comparison dyads, had significantly higher scores on the Care Transition Measure-15 (74.7 vs. 65.3, Mean Ratio 1.16, 95% CI: 1.08, 1.24). Comparison and intervention dyads reported similar outcomes at 30 days: (a) on a five-point scale, mean self-rated health was 2.69 vs. 2.94; (b) on a four-point scale, the mean change in ADL disability from baseline to 30 days was 0.89 vs. 1.16; (c) the number of self-reported falls was 8 (13.1%) vs. 11 (17.7%); (d) the number of patient hospitalizations was 3 (4.9%) vs. 4 (6.4 %); (e) the number of self-reported ED visits 3 (4.9%) vs. 5 (8.0%); and (f) the number of unmet needs was 14 (22.9%) vs. 12 (19.3%).
Discussion
Annually in the U.S., 1.8 million older adults transfer from hospitals to approximately 15,000 nursing homes providing Medicare post-acute care services.26 This study tested an intervention to improve SNF staff’s capacity to prepare older adults and their caregivers for transitions from SNFs to home. The findings suggest that Connect-Home was feasible, relevant to staff, and associated with improved patient and caregiver dyads’ preparedness for post-SNF care. Prior studies indicate that older adults and their caregivers who are prepared for transitions in care experience fewer medical complications and avoid hospital readmissions.13,27 Informed by organizational theory,28,29 the intervention was designed to optimize the way professional staff, caregivers and individual patients worked in teams to develop transition plans and ensure continuity of care during patient transitions.
Few studies have tested transitional care of SNF patients and caregivers. Among these, interventions delivered in a SNF,30 patient visits to a specialized clinic,31 and pharmacist home visits32 were associated with reduced rates of hospital readmissions or emergency department visits. These studies either used added staff or resources to provide transitional care or were tested in a single SNF, which may limit their use in the current post-acute care environment. Our preliminary findings indicate that Connect-Home improves preparedness for discharge without need for additional staff, suggesting that it has the potential to be generalizable and cost-effective. Further research will be needed to determine its impact on re-admissions and other outcomes.19
With increasing SNF accountability for patient outcomes after discharge, nursing home leaders will need to develop new services.27 In this study, we did not measure the relevance of the intervention to nursing home administrators; however, when the study was complete, administrators in the study sites urged the research team to sustain the intervention, and expand it to additional SNFs. These projects are ongoing, and suggested the relevance of Connect-Home to administrators.
Findings suggest implications for future research. First, in the telephone follow-up call, we reached only 56% of patients or caregivers; additional strategies will be needed to increase patient and caregiver participation. Second, studies indicate that post-discharge outcomes can be improved with medication reconciliation; future studies should include this element of care and measure adverse drug events. Third, future studies should measure the cost of training and time to deliver intervention components. Fourth, future transitional care interventions in SNFs may require additional post-discharge services for dyads with the greatest risk for poor outcomes. Studies are needed to sustain transitional care services in SNFs, such as staff training and procedures to monitor program fidelity.
The findings in this pilot study are limited by use of a quasi-experimental design without randomization or concurrent controls; use of only three SNFs in one nursing home chain; and testing with a small sample of dyads that was primarily white, female, and ineligible for Medicaid. Future controlled, randomized studies of transitional care in SNFs are needed with more representative populations and sufficient sample sizes to analyze outcomes at 30 days after SNF discharge.28
Conclusions
The transitional care services in the Connect-Home study were feasible, valued by staff, and improved preparedness for discharge. The next step will be to test Connect-Home using a cluster randomized trial using patient-oriented outcomes including fall rates, hospital use after discharge, and the cost of care.
Supplementary Material
Supplementary Material S1. Resources and Guidance to Implement Connect-Home
Acknowledgments
Funding
Supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Grant Number 1KL2TR001109.
The authors acknowledge the contributions of Lydia Foy, Deborah Tillman, and other valued staff in BLINDED for their contributions to the research in the study SNFs.
The authors have not conflicts of interest to disclose.
Footnotes
An abstract of this study was submitted to and selected for podium presentation at the 2017 Annual Scientific Meeting of the American Geriatrics Society.
Authors’ Contributions
Mark Toles drafted the manuscript. All authors contributed to the conception, analysis, interpretation and revision of the manuscript. All authors agree about the final version of the manuscript.
References
- 1.Medicare Payment Advisory Commission. Report to Congress. [Accessed April 7, 2015];Medicare Payment Policy. 2013 http://www.medpac.gov/-documents-/reports.
- 2.Byrne K, Orange JB, Ward-Griffin C. Care transition experiences of spousal caregivers: from a geriatric rehabilitation unit to home. Qual Health Res. 2011 Oct;21(10):1371–1387. doi: 10.1177/1049732311407078. [DOI] [PubMed] [Google Scholar]
- 3.Levine C, Halper D, Peist A, et al. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood) 2010 Jan-Feb;29(1):116–124. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 4.Coleman EA, Min SJ, Chomiak A, et al. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004 Oct;39(5):1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toles M, Anderson RA, Massing M, et al. Restarting the cycle: incidence and predictors of first acute care use after nursing home discharge. J Am Geriatr Soc. 2014 Jan;62(1):79–85. doi: 10.1111/jgs.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health and Human Services. [Accessed September 28, 2016];Skilled nursing facilities often fail to meet care planning and discharge planning requirements. 2013 https://oig.hhs.gov/oei/reports/oei-02-09-00201.pdf.
- 7.Toles M, Colon-Emeric C, Naylor MD, et al. Transitional care in skilled nursing facilities: a multiple case study. BMC health services research. 2016;16:186. doi: 10.1186/s12913-016-1427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee J. An imperative to improve discharge planning: Predictors of physical function among residents of a Medicare skilled nursing facility. Nurs Adm Q. 2006 Jan-Mar;30(1):38–47. doi: 10.1097/00006216-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Popejoy LL, Dorman Marek K, et al. Patterns and problems associated with transitions after hip fracture in older adults. J Gerontol Nurs. 2013 Sep;39(9):43–52. doi: 10.3928/00989134-20130620-01. [DOI] [PubMed] [Google Scholar]
- 10.Toles M, Abbott KM, Hirschman KB, et al. Transitions in care among older adults receiving long-term services and supports. J Gerontol Nurs. 2012 Nov;38(11):40–47. doi: 10.3928/00989134-20121003-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003 Apr;51(4):556–557. doi: 10.1046/j.1532-5415.2003.51186.x. [DOI] [PubMed] [Google Scholar]
- 12.Naylor MD. Transitional care of older adults. Annu Rev Nurs Res. 2002;20:127–147. [PubMed] [Google Scholar]
- 13.Verhaegh KJ, MacNeil-Vroomen JL, Eslami S, et al. Transitional care interventions prevent hospital readmissions for adults with chronic illnesses. Health Aff (Millwood) 2014 Sep 1;33(9):1531–1539. doi: 10.1377/hlthaff.2014.0160. [DOI] [PubMed] [Google Scholar]
- 14.Naylor MD, Aiken LH, Kurtzman ET, et al. The care span: The importance of transitional care in achieving health reform. Health Aff (Millwood) 2011 Apr;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 15.Anderson RA, Colon-Emeric C. Outcomes of Nursing Management Practices in Nursing Homes. National Institute of Nursing Research, National Institutes of Health; 2012. [Google Scholar]
- 16.Jack BW. [Accessed November 1, 2013];Project RED (Re-Engineered Discharge) 2013 http://www.bu.edu/fammed/projectred/
- 17.Naylor [Accessed November 1, 2013];Transitional Care Model. 2013 http://www.transitionalcare.info/
- 18.Coleman EA, Smith JD, Frank JC. Development and testing of a measure designed to assess the quality of care transitions. International Journal of Integrative Care. 2009 Aug 8; doi: 10.5334/ijic.60. 2002. www.ijic.org. [DOI] [PMC free article] [PubMed]
- 19.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: The care transitions measure. Med Care. 2005 Mar;43(3):246–255. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Parry C, Mahoney E, Chalmers SA, et al. Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008 Mar;46(3):317–322. doi: 10.1097/MLR.0b013e3181589bdc. [DOI] [PubMed] [Google Scholar]
- 21.Bass PF, 3rd, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003 Dec;18(12):1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute of Health. [Accessed February 20, 2014];NIH Instrumental Support SF 18+ 2012 http://www.nihtoolbox.org/WhatAndWhy/Emotion/SocialRelationships/Social%20Relationships/NIH%20TB%20SR%20Instrumental%20Support%20SF%2018+.pdf.
- 23.Bedard M, Molloy DW, Squire L, et al. The Zarit Burden Interview: a new short version and screening version. Gerontologist. 2001 Oct;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. [Accessed November 25, 2014];CDC Health Related Quality of Life –14 “Healthy Days Measure”. http://www.cdc.gov/hrqol/hrqol14_measure.htm.
- 25.Gill TM, Gahbauer EA, Han L, et al. Functional trajectories in older persons admitted to a nursing home with disability after an acute hospitalization. J Am Geriatr Soc. 2009 Feb;57(2):195–201. doi: 10.1111/j.1532-5415.2008.02107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Medicare Payment Advisory Commission. Report to Congress. [Accessed September 26, 2016];Medicare payment policy. 2016 http://www.medpac.gov/docs/default-source/reports/june-2016-report-to-the-congress-medicare-and-the-health-care-delivery-system.pdf?sfvrsn=0.
- 27.Toles M, Colon-Emeric C, Asafu-Adjei J, et al. Transitional care of older adults in skilled nursing facilities: A systematic review. Geriatric nursing (New York, NY ) 2016 Jul-Aug;37(4):296–301. doi: 10.1016/j.gerinurse.2016.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carnahan JL, Unroe KT, Torke AM. Hospital Readmission Penalties: Coming Soon to a Nursing Home Near You! J Am Geriatr Soc. 2016;64(3):614–618. doi: 10.1111/jgs.14021. [DOI] [PubMed] [Google Scholar]
- 28.Anderson RA, Toles MP, Corazzini K, et al. Local interaction strategies and capacity for better care in nursing homes: a multiple case study. BMC health services research. 2014;14:244. doi: 10.1186/1472-6963-14-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colon-Emeric C, Pinheiro SO, Anderson RA, et al. Connecting the learners: improving uptake of a nursing home educational program by focusing on staff interactions. Gerontologist. 2013 May 23; doi: 10.1093/geront/gnt043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berkowitz RE, Fang Z, Helfand BK, et al. Project Reengineered Discharge (RED) Lowers Hospital Readmissions of Patients Discharged From a Skilled Nursing Facility. J Am Med Dir Assoc. 2013 Oct;14(10):736–740. doi: 10.1016/j.jamda.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Park HK, Branch LG, Bulat T, et al. Influence of a transitional care clinic on subsequent 30-day hospitalizations and emergency department visits in individuals discharged from a skilled nursing facility. J Am Geriatr Soc. 2013 Jan;61(1):137–142. doi: 10.1111/jgs.12051. [DOI] [PubMed] [Google Scholar]
- 32.Reidt SL, Holtan HS, Larson TA, et al. Interprofessional Collaboration to Improve Discharge from Skilled Nursing Facility to Home: Preliminary Data on Postdischarge Hospitalizations and Emergency Department Visits. J Am Geriatr Soc. 2016 Sep;64(9):1895–1899. doi: 10.1111/jgs.14258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kind AJ, Brenny-Fitzpatrick M, Leahy-Gross K, et al. Harnessing Protocolized Adaptation in Dissemination: Successful Implementation and Sustainment of the Veterans Affairs Coordinated-Transitional Care Program in a Non-Veterans Affairs Hospital. J Am Geriatr Soc. 2016 Feb;64(2):409–416. doi: 10.1111/jgs.13935. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material S1. Resources and Guidance to Implement Connect-Home