Abstract
Aim
To determine the formula that predicts the injury severity score from parameters that are obtained in the emergency department at arrival.
Methods
We reviewed the medical records of trauma patients who were transferred to the emergency department of Gunma University Hospital between January 2010 and December 2010. The injury severity score, age, mean blood pressure, heart rate, Glasgow coma scale, hemoglobin, hematocrit, red blood cell count, platelet count, fibrinogen, international normalized ratio of prothrombin time, activated partial thromboplastin time, and fibrin degradation products, were examined in those patients on arrival. To determine the formula that predicts the injury severity score, multiple linear regression analysis was carried out. The injury severity score was set as the dependent variable, and the other parameters were set as candidate objective variables. IBM spss Statistics 20 was used for the statistical analysis. Statistical significance was set at P < 0.05. To select objective variables, the stepwise method was used.
Results
A total of 122 patients were included in this study. The formula for predicting the injury severity score (ISS) was as follows: ISS = 13.252–0.078(mean blood pressure) + 0.12(fibrin degradation products). The P‐value of this formula from analysis of variance was <0.001, and the multiple correlation coefficient (R) was 0.739 (R2 = 0.546). The multiple correlation coefficient adjusted for the degrees of freedom was 0.538. The Durbin–Watson ratio was 2.200.
Conclusions
A formula for predicting the injury severity score in trauma patients was developed with ordinary parameters such as fibrin degradation products and mean blood pressure. This formula is useful because we can predict the injury severity score easily in the emergency department.
Keywords: Biomarker, fibrin degradation products (FDP), injury severity score (ISS), multiple linear regression analysis, trauma
Introduction
Trauma is the main cause of death in young people in Japan, that carries the country's social future. In particular, mortality rises in patients with multiple traumas. Emergency physicians and trauma surgeons devote themselves to eradicate preventable trauma death. Grasping the severity of trauma patients precisely and quickly after arrival at the hospital is important in the management of trauma patients.
The injury severity score (ISS) developed by Baker et al.1 is a score that reflects the severity of multiple traumas, and is one of the most widely used scoring tools for trauma. The ISS is calculated as the sum of the square of the highest abbreviated injury score of each part of the body. However, the ISS cannot be obtained immediately after arrival at the hospital because detailed evaluation with image examinations such as roentgenogram, ultrasound, and/or computed tomography is required for calculation of the ISS. Emergency physicians and trauma surgeons have to carry out the initial evaluation with the suspected ISS of the patients. In our previous study, we reported that the blood levels of fibrin degradation products (FDP) and D‐dimer upon arrival at the hospital reflected the severity of trauma and those parameters were directly related with the ISS.2 However, the precise ISS could not be predicted with only those two parameters.
The purpose of this study was to develop a model that predicts the ISS precisely and simply based on the parameters obtained in the emergency department at arrival.
Patients and Methods
The protocol of this study was approved without the need for informed consent by the research ethics board of The Gunma University Hospital (Maebashi, Japan).
We reviewed the medical records of trauma patients who were transferred to the emergency department of Gunma University Hospital between January 2010 and December 2010. The exclusion criteria were set as follows: patients who received blood transfusion and/or other procedures at another hospital before being transferred to our hospital, and patients with conditions and/or diseases that resulted in coagulation abnormality such as blood disease, advanced malignant tumor, pregnancy, severe hepatic dysfunction, and taking anticoagulant agents.
We reviewed the heart rate, mean blood pressure (mBP), Glasgow coma scale, hematocrit, hemoglobin, red blood cell count, platelet count, international normalized ratio of prothrombin time, activated partial thromboplastin time, fibrinogen, and FDP levels in those patients upon arrival at our hospital. The hematocrit, hemoglobin, and platelet count were measured with the fluoro‐flow cytometry method using an XE‐5000 (Sysmex, Kobe, Japan), and international normalized ratio of prothrombin time, activated partial thromboplastin time, FDP, and fibrinogen were measured using the CS‐2000i (Sysmex); FDP was measured by the immunoturbidimetric method.
In addition, the patients' ISS was calculated using the method of Baker et al.1 We evaluated the relationships between the ISS and other factors to find useful parameters reflecting the severity of trauma immediately after transportation to the hospital.
Statistical analysis
The relationships between the ISS and other parameters were analyzed by linear regression analysis.
To determine the formula that predicts the ISS, multiple linear regression analysis was carried out. The ISS was set as the dependent variable, and the other parameters were set as candidate objective variables. To select objective variables, the stepwise method was used. Multicollinearity was evaluated by the variance inflation factor, and autocorrelation was evaluated by the Durbin–Watson ratio. IBM (Tokyo, Japan) spss Statistics 20 was used for the statistical analysis. Statistical significance was assumed to be present at P < 0.05.
Results
A total of 738 patients with trauma were transferred to our emergency department between January 2010 and December 2010. This study included 122 patients with trauma. The other 616 patients were excluded based on the criteria described above. They were all civilian. The causes of trauma were as follows: traffic accident, 59 patients; fall, 37; sports, 6; assault, 4; self‐injury, 4; and other, 12. The male/female ratio was 74/48, and the mean age of the patients was 51.4 ± 21.9 (range, 7–89) years old. Four patients (3.3%) died in our hospital and 118 patients (96.7%) were discharged alive from our hospital.
Table 1 shows the median and interquartile range of each parameter, and Pearson's correlation coefficient between the ISS and each parameter.
Table 1.
Characteristics of trauma patients who came to the emergency department of Gunma University Hospital, January–December 2010 (n = 122)
| Median | Interquartile range | R for ISS | |
|---|---|---|---|
| ISS | 4.00 | 9.00 | 1.000 |
| Age, years | 51.00 | 38.80 | 0.175 |
| HR, b.p.m. | 81.50 | 23.30 | −0.181* |
| mBP, mmHg | 104.50 | 28.20 | −0.406** |
| GCS | 15.00 | 1.00 | −0.446** |
| Ht, % | 40.90 | 6.30 | −0.293** |
| Hb, g/dL | 14.10 | 2.60 | −0.040 |
| RBC, ×106/μL | 4.50 | 0.80 | −0.053 |
| Plt, ×104/μL | 21.10 | 6.00 | 0.083 |
| Fib, mg/dL | 243.00 | 88.00 | −0.284** |
| PT‐INR | 1.01 | 0.01 | 0.497** |
| APTT, s | 30.40 | 5.35 | 0.485** |
| FDP, μg/mL | 4.95 | 13.10 | 0.710** |
*P < 0.05, **P < 0.01. APTT, activated partial thromboplastin time; FDP, fibrin degradation products; Fib, fibrinogen; GCS, Glasgow coma scale; Hb, hemoglobin; HR, heart rate; Ht, hematocrit; ISS, injury severity score; mBP, mean blood pressure; Plt, platelet count; PT‐INR, international normalized ratio of prothrombin time; RBC, red blood cell count.
The results of multiple linear regression analysis are shown in Table 2. The ISS prediction model is as follows;
Table 2.
Multiple linear regression analysis for predicting the injury severity score in trauma patients
| PRC | Standardized PRC | P‐value | 95% CI | VIF | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Invariable | 13.252 | <0.01 | 8.178 | 18.325 | ||
| mBP | −0.078 | −0.216 | 0.01 | −0.124 | −0.032 | 1.095 |
| FDP | 0.120 | 0.646 | <0.01 | 0.096 | 0.144 | 1.095 |
CI, confidence interval; FDP, fibrin degradation products; mBP, mean blood pressure; PRC, partial regression coefficient; VIF, variance inflation factor.
The P‐value of this model based on anova <0.001, and the multiple correlation coefficient (R) was 0.739; therefore, R2 was 0.546. The multiple correlation coefficient adjusted for the degrees of freedom was 0.538. The Durbin–Watson ratio was 2.200. There was one outlier over 3SD (Standard Deviation). Figure 1 shows the scatter plot of residual error between the ISS and the predicted ISS calculated by this predictive model. A scatter plot of both the actual and predicted ISS values is shown in Figure 2.
Figure 1.
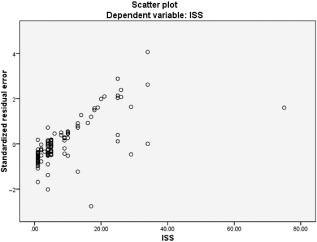
Scatter plot of residual error between the injury severity score (ISS) and predicted ISS in trauma patients on arrival at the emergency department (n = 122), calculated by the predictive formula: ISS = 13.252 − 0.078 × mean blood pressure + 0.12 × fibrin degradation products.
Figure 2.
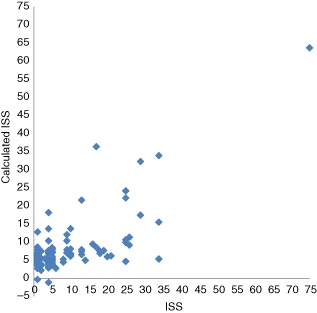
Scatter plot of both the actual and predicted injury severity scores (ISS) in trauma patients on arrival at the emergency department (n = 122), calculated by the predictive formula: ISS = 13.252 − 0.078 × mean blood pressure + 0.12 × fibrin degradation products.
Discussion
The physiological evaluation of patients is one of the most important tasks carried out in the emergency room. The clinical guidelines for trauma, such as the Advanced Trauma Life Support and Japan Advanced Trauma Evaluation and Care recommend that physicians evaluate physiological findings first and resuscitate if necessary, and assess anatomical findings second. These useful guidelines make great contributions to reducing preventable trauma death. However, it is difficult to find all traumas in the initial evaluation, even if the clinical examinations are carried out according to the diagnostic guidelines. Additionally, there are patients who have no complaints and are asymptomatic at arrival even though they are injured. To reduce the overlooking of trauma, we paid attention to blood coagulation upon arrival at the emergency department. We previously reported that FDP and D‐dimer levels of the patients who died and/or required massive transfusion were higher than those of other patients in that study. We also reported that the serum levels of FDP and D‐dimer were correlated with the ISS and these levels at arrival could be used to detect concealed trauma.2
The ISS is one of the most common and famous scoring systems to evaluate the severity of multiple injuries and has been used widely throughout the world.1 The ISS was a breakthrough because ISS made it possible to stratify patients who had a variety of organ trauma attributable to a number of causes. The trauma and injury severity score (TRISS) is a mathematical regression model that predicts the probability of survival in injured patients, and can be calculated based on the type of injury, the revised trauma score, the patient's age, and the ISS. Based on this calculated probability of survival, the patient's actual outcome (alive or dead) can be compared with the predicted outcome, and this ratio in a group of injured patients can be used as a measure of quality of care.3, 4, 5, 6 Thus, both the ISS and TRISS have made great contributions to the development of traumatology. However, the ISS has some problems. The ISS cannot be used for the evaluation of trauma severity in the pre‐hospital situation and/or immediately after arrival to the hospital because it shows only the results of anatomical evaluation and does not include the results of physiological evaluation, and cannot distinguish patients who are already in the shock state on arrival at the hospital from those with normal vital signs.
Some useful scoring systems of trauma such as the International Classification of Diseases code‐based Injury Severity Score7 and the New Injury Severity Score8 were developed to improve the precision or to make calculation easy. Recently, studies that compared the relative merits of these scoring systems have been published,9, 10 and these new scoring tools might be a little better than the ISS. However, the ISS has been used more widely than the other scoring systems up to the present because the difference between ISS and the others is quite small. Aydin et al.11 mentioned in their report that there was no significant difference when using the New Injury Severity Score instead of the ISS to calculate the TRISS, despite the fact that the ISS had been reported approximately 40 years ago.
Although the ISS is a good scoring system for trauma patients, the procedure for calculating the ISS is complicated12 and it is not possible for physicians in the emergency room to obtain the ISS of patients with trauma on arrival.
The ISS (and TRISS) reflect patients' prognosis. We do not decide to proceed to surgery or blood transfusion based on the ISS or TRISS, however, to know the provability of dying of trauma patients at arrival easily is useful for decision of treatment (for example, preparation of blood transfusion and/or operation). If we could establish the ISS of a trauma patient in the emergency department, it would be useful because we are able to predict their prognosis more easily. Therefore, we thought that it would be useful if there was a method of predicting the level of ISS based on ordinary clinical data. To our knowledge, there is no report regarding such an idea. We used multiple linear regression analysis to develop a predictive model as simple as possible. For usefulness in clinical situations, the candidate objective variables should be able to be obtained easily and quickly in the emergency department. This model is remarkably simple and needs only two objective variables, FDP and mBP, both of which can be easily and quickly obtained in the emergency department. The blood level of FDP has an equilateral correlation with ISS and mBP has a negative correlation with ISS; therefore, the partial regression coefficient of FDP is positive and that of mBP is negative. The standardized partial regression coefficient of FDP was 0.646, and that of mBP was −0.216. The multiple correlation coefficient (R) was 0.739 and it was thought that R is sufficiently high. The Durbin–Watson ratio was 2.200 and this is close to 2.0. Therefore, it is thought that this formula has predictive value.
Limitations
This was a retrospective study, and the number of patients was not large. Trauma patients in whom only the FDP level in blood was examined were included in this study. Blood examination was carried out in all patients at arrival, however, the duration from injury to FDP measurement was not considered. A large number of the cases analyzed in this study were not severe and the patients did not require transfusion and/or emergent surgical interventions. This study might be useful only to comprehend the pathophysiology of trauma patients, not to help clinical decision‐making. Further studies should be carried out in a multicenter setting.
Conclusion
We have developed a model to predict the ISS of trauma patients easily and quickly in an emergency situation. The model for predicting the ISS is as follows; ISS = 13.252 − 0.078 × mBP + 0.12 × FDP. This model is useful because the ISS can be predicted using only the FDP level and mBP, which are ordinary parameters in clinical situations.
Conflict of Interest
None.
References
- 1. Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 1974; 14: 187–196. [PubMed] [Google Scholar]
- 2. Hagiwara S, Oshima K, Aoki M et al Usefulness of fibrin degradation products and D‐dimer levels as biomarkers that reflect the severity of trauma. J. Trauma Acute Care Surg. 2013; 74: 1275–1278. [DOI] [PubMed] [Google Scholar]
- 3. Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: The TRISS method trauma score and the injury severity score. J. Trauma 1987; 27: 370–378. [PubMed] [Google Scholar]
- 4. Champion H, Sacco WJ, Lepper RL. An anatomic index of injury severity. J. Trauma 1980; 20: 197–202. [DOI] [PubMed] [Google Scholar]
- 5. Copes WS, Champion HR, Sacco WJ. The Injury Severity Score revisited. J. Trauma 1988; 28: 69–77. [DOI] [PubMed] [Google Scholar]
- 6. Rutledge R, Osler T, Emery S, Kromhout‐Schiro S. The end of the injury severity score (ISS) and the trauma injury severity score (TRISS): ICISS, an International Classification of Diseases, ninth revision‐based prediction tool, outperforms both ISS and TRISS as predictors of trauma patient survival, hospital charges, and hospital length of stay. J. Trauma 1998; 44: 41–49. [DOI] [PubMed] [Google Scholar]
- 7. Osler T, Rutledge R, Deis J, Bedrick E. ICISS: An international classification of disease‐9 based injury severity score. J. Trauma 1996; 41: 380–386. [DOI] [PubMed] [Google Scholar]
- 8. Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J. Trauma 1997; 43: 922–925. [DOI] [PubMed] [Google Scholar]
- 9. Tohira H, Jacobs I, Mountain D, Gibson N, Yeo A. Systematic review of predictive performance of injury severity scoring tools. Scand. J. Trauma Resusc. Emerg. Med. 2012; 20: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Frankema SP, Steyerberg EW, Edwards MJ, van Vugt AB. Comparison of current injury scales for survival chance estimation: An evaluation comparing the predictive performance of the ISS, NISS, and AP scores in a Dutch local trauma registration. J. Trauma 2005; 58: 596–604. [DOI] [PubMed] [Google Scholar]
- 11. Aydin SA, Bulut M, Ozgüç H et al Should the New Injury Severity Score replace the Injury Severity Score in Trauma and Injury Severity Score? Ulus. Travma Acil Cerrahi Derg. 2008; 14: 308–312. [PubMed] [Google Scholar]
- 12. Wong SS, Leung GK. Injury severity score (ISS) vs. ICD‐derived injury severity score (ICISS) in a patient population treated in a designated Hong Kong trauma center. Mcgill J. Med. 2008; 11: 9–13. [PMC free article] [PubMed] [Google Scholar]


