Abstract
Objectives:
The operating room is a place of surgical intervention with its accompanying bodily and cognitive strain on the performers. Stress in the operating room may lead to the onset of central serous chorioretinopathy as reported hereby in a retina surgeon and is labeled as operating room central serous chorioretinopathy.
Methods:
The same operator performed the optical coherence tomography scans on one retina surgeon. A masked observer estimated the maximal height of the subretinal fluid.
Results:
Central serous chorioretinopathy recurred four times over a 1-year period 1 -2 days after a stressful day in the operating room, especially when cases were done under topical or subtenon anesthesia for cataract surgery, vitreous surgery or combined surgeries with complex ocular and medical problems and inability for anesthesia team to intervene. Stress management allowed resolution of subretinal fluid between 3 and 4 weeks. Adopting this strategy, no further attacks were documented by optical coherence tomography for 5 years.
Conclusions:
(1) This is one of a few optical coherence tomography documentation of resolution of central serous chorioretinopathy within 3-4 weeks of its occurrence and its recurrence induced by stress in the operating room; (2) Unassisted topical anesthesia required in patients with complex medical and ocular problems causes more cognitive stress than when surgery is carried under assisted local or general anesthesia (partly due to unexpected ocular or bodily movements); and (3) the available evidence suggests that those overcommitted surgeons (type A personality) may very well be most susceptible to burnout and central serous chorioretinopathy.
Keywords: Ophthalmology, surgery
Introduction
Current life is full of target dates, dissatisfaction and increasing demands with strain becoming a way of life. Persistent anxiety is linked with several disorders such as systemic hypertension, coronary artery disease, accelerated atherosclerosis and central serous chorioretinopathy (CSCR).1,2 Operating rooms are one source of stress with up to 40% of responding surgeons reporting burnout and emotional exhaustion in one study.3 In general, many surgeons choose this challenging medical specialty to witness the enjoyment of promoting healing, yet with remarkable challenges often accompanied with distress. Intraoperative stress may lead to the onset of CSCR in surgeons.2,3 We report the case of CSCR dominated by the stress of the operating room.
Case report
A 56-year-old US-trained retinal specialist noted a dark central scotoma spot with micropsia on 6 September 2010. Visual acuity was 6/6 bilaterally. Funduscopy and spectral-domain optical coherence tomography (OCT) revealed left foveal detachment (Figure 1). Medical history included irritable bowel syndrome, migraine, labile minimal systemic hypertension and type A personality with neither sleep apnea nor corticosteroid intake in any form. Serial OCT revealed resolution of subretinal fluid after a period of relaxed work and recurrence at the time of surgery. The source of stress was primarily from the operating room. CSCR occurred 1–2 days after the surgeon expressed high degrees of stress in the operating room. The majority of surgeries were carried under topical or subtenon anesthesia with little anesthesia assistance due to lack of experienced anesthesia personnel (junior anesthesia resident or anesthesia assistant), especially in satellite surgical centers; being a referral tertiary center, patients were very sick on several anticoagulants with repeated cough, miotic pupils (diabetic, pseudoexfoliation, intake of alpha blocker), Alzheimer disease, congestive heart failure, orthopnea or morbid obesity. Surgeries carried under general anesthesia were not accompanied by much perceived stress or recurrence of subretinal fluid. Complete resolution of subretinal fluid by OCT occurred as soon as 3–4 weeks after stress management. The same operator performed the OCT scans. A masked observer determined maximal height of the subretinal fluid.
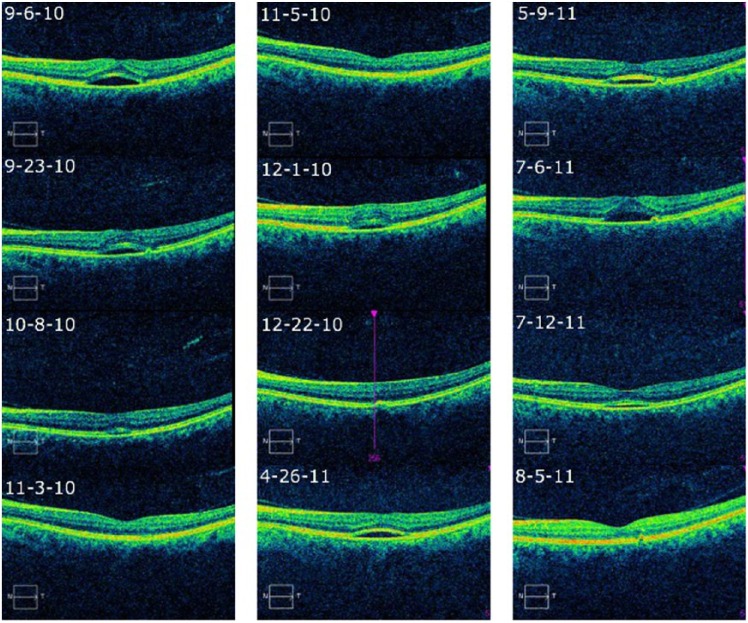
Figure 1.
CSCR of the left eye at initial visit and 6-year follow-up OCT scans. Resolution of subretinal fluid 4 weeks later. Four recurrences within 1 year. Resolution of central serous fluid 4 weeks after each attack. No recurrences noted 5 years after the last recurrence.
Subretinal fluid occurred within 24–48 h of the perceived stress and took 3–4 weeks for resolution. Each recurrence was preceded by a stressful day in the operating room. After four recurrences over a 1-year period (Figure 1), there were no further recurrences for the next 5 years of follow-up by serial biweekly OCT (total 6-year follow-up) (Table 1). This could be achieved by stress management strategy (decrease workload, avoid operating on very complex cases under topical anesthesia, avoid emergency cases or operating on weekends or afterhours when the retina nursing staff is not around, complete adherence to zero caffeine intake, good sleep before the day of surgery, walk half an hour daily). Since the initiation of the stress management plan 1 year after the initial episode of CSCR, the surgeon did not experience any stressful episodes. Enhanced depth OCT revealed thickened choroid and angio OCT failed to reveal choroidal new vessel under the detachment of the retinal pigment epithelium.
Table 1.
OCT data over 6-year follow-up.
| Month/day/year | Time | Maximum height of subretinal fluid (µm) | Onset of CSCR | Source of stress |
|---|---|---|---|---|
| 9/5/2010 | 11:46 am | 126 | First episode | OR stress preceded by clinic overload |
| 9/6/2010 | 2:50 pm | 134 | ||
| 9/15/2010 | 7:07 am | 141 | ||
| 9/22/2010 | 6:05 pm | 67 | ||
| 9/23/2010 | 7:25 am | 81 | ||
| 5:46 pm | 112 | |||
| 9/26/2010 | 7:58 am | 83 | Recurrence #1 | OR stress |
| 4:43 pm | 67 | |||
| 10/4/2010 | 7:42 am | 30 | ||
| 5:50 pm | 44 | |||
| 10/7/2010 | 11:39 am | 44 | ||
| 10/12/2010 | 6:02 pm | 22 | ||
| 11/2/2010 | 7:34 pm | 7 | ||
| 11/4/2010 | 2:50 pm | 119 | Recurrence #2 | OR stress |
| 11/7/2010 | 5:32 pm | 67 | ||
| 11/30/2010 | 7:18 pm | 59 | ||
| 12/21/2010 | 7:29 pm | 0 | ||
| 2/10/2011 | 2:05 pm | 0 | ||
| 3/2/2011 | 5:55 pm | 0 | ||
| 4/26/2011 | 7:15 pm | 72 | Recurrence #3 | OR stress + prepare for lectures abroad |
| 5/9/2011 | 5:07 pm | 52 | ||
| 7/6/2011 | 5:59 pm | 76 | Recurrence #4 | OR stress |
| 7/12/2011 | 6:20 pm | 8 | ||
| 8/5/2011 | 4:49 pm | 0 | ||
| 10/28/2011 | 2:52 pm | 0 | ||
| 6/6/2015 | 5:38 am | 0 | ||
| 4/10/2016 | 5:26 am | 0 | 6-year follow-up |
OR: operating room; OCT: optical coherence tomography; CSCR: central serous chorioretinopathy.
Bold values represent the time of recurrence to emphasize what happened when the attack occurred.
Discussion
The hypothalamic–pituitary–adrenocortical axis and the sympatho-adrenal system represent the principal mediators for stress stimuli. When the system is persistently over-burdened, a variety of illnesses appear to arise such as systemic hypertension or atherosclerosis. Chronic stress is accompanied by elevated corticosteroid serum levels that can affect the hippocampus resulting in decreased cognitive abilities. The best example of how stress can result in a well-perceived disease is the post-traumatic stress disorder.
Type A personality and obstructive sleep apnea have been involved in the pathogenesis of CSCR, possibly from elevated serum epinephrine and cortisol, both secondarily altering the autoregulation of the choroidal circulation.4 Both acute and chronic stress are present in all facets of surgery from organizational matters, changing technologies, or interactions with coworkers. Surgery is a challenging profession from the burden of both physical and cognitive efforts.5,6 Therefore, some authors tried to investigate the cognitive efforts of surgeons during surgery that potentially result in cardiovascular changes. The methodology adopted included monitoring of pulse as well as variability of heart rate,7 together with simultaneous documentation of the level of perceived stress. Prolonged sympathetic hyperactivity could anticipate CSCR occurrence and recurrence. Surgeons most dedicated to their patient appear most prone to burnout.6,7
Surgical specialty is rapidly evolving with the adoption of technologies like laparoscopic and robotic surgery. Minimally invasive surgery is known to require higher mental concentration for surgeons than conventional surgery.5 Stress appears related to years of experience and complexity of surgery (tertiary centers get complex difficult cases).7 In Ophthalmology, topical anesthesia and small-incision phacoemulsification8 or vitrectomy9 has allowed successful surgery in very severely ill subjects (morbid obesity,8,9 kyphosis, Parkinson, congestive heart failure, recent myocardial infarction or cerebrovascular accident). Moreover, many such patients cannot tolerate any sedative and hence there is more reliance on surgical skills to do intricate precise surgery in somewhat uncooperative patient further raising the degree of surgical stress. Expeditious and yet precise technique is essential to do phacoemulsification or vitreous surgery in restless patients under topical anesthesia with no sedation. Any delay in surgery (from machine failure, program shutdown, missing or damaged instruments or disposable like endolaser or vitrector), circulating nurse not available all the time, nurses not familiar with ophthalmology procedures and incompetent anesthesia staff (rotating junior resident with little experience or anesthesia technician not allowed to give sedation) can irritate the patient and surgeon resulting in heightened prolonged stress.
Neurosensory detachment in CSCR resolves spontaneously in a majority of patients with 40%–50% having recurrences in the same eye.10–12 The current case is the first documentation of diurnal variation of subretinal fluid (Table 1) in CSCR.10 Also this is the third OCT documentation of resolution of CSCR within 3–4 weeks11,12 of its occurrence. The time of resolution of CSCR was mentioned in the literature10–12 as 2–3 months, before the advent of OCT. Gruszka11 reported resolution of subretinal fluid after 1 month of eplerenone therapy, while Ng et al.10 detected resorption of subretinal fluid 3 weeks following rapid tapering of systemic corticosteroids and restoration of emotional well-being in a patient with graft versus host disease and steroid-induced CSCR.
In conclusion, we present a unique case of an ophthalmologist surgeon who recorded meticulously the recurrence of CSCR shortly after severe stress during surgery over 1 year, resolution of subretinal fluid from 3 to 4 weeks after each attack and cessation of the attacks following adoption of stress management strategy.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article.
References
- 1. Bazzazi N, Ahmadpanah M, Akbarzadeh S, et al. In patients suffering from idiopathic central serous chorioretinopathy, anxiety scores are higher than in healthy controls, but do not vary according to sex or repeated central serous chorioretinopathy. Neuropsychiatr Dis Treat 2015; 11: 1131–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Demirtas Y, Tulmac M, Yavuzer R, et al. Plastic surgeon’s life: marvelous for mind, exhausting for body. Plast Reconstr Surg 2004; 114: 923–931. [DOI] [PubMed] [Google Scholar]
- 3. Businger A, Stefenelli U, Guller U. Prevalence of burnout among surgical residents and surgeons in Switzerland. Arch Surg 2010; 145: 1013–1016. [DOI] [PubMed] [Google Scholar]
- 4. Tewari HK, Gadia R, Kumar D, et al. Sympathetic-parasympathetic activity and reactivity in central serous chorioretinopathy: a case-control study. Invest Ophthalmol Vis Sci 2006; 47: 3474–3478. [DOI] [PubMed] [Google Scholar]
- 5. Schuetz M, Gockel I, Beardi J, et al. Three different types of surgeon-specific stress reactions identified by laparoscopic simulation in a virtual scenario. Surg Endosc 2008; 22: 1263–1267. [DOI] [PubMed] [Google Scholar]
- 6. Balch CM, Shanafelt T. Combating stress and burnout in surgical practice: a review. Adv Surg 2010; 44: 29–47. [DOI] [PubMed] [Google Scholar]
- 7. Jones KI, Amawi F, Bhalla A, et al. Assessing surgeon stress when operating using heart rate variability and the state trait anxiety inventory: will surgery be the death of us? Colorectal Dis 2015; 17: 335–341. [DOI] [PubMed] [Google Scholar]
- 8. Mansour AM, Dairy M. Surgical modifications in cataract for morbid obesity. J Cat Refract Surg 2004; 30: 2265–2268. [DOI] [PubMed] [Google Scholar]
- 9. Mansour AM. Standing vitrectomy in morbid obesity. Retina 2006; 26: 963–964. [DOI] [PubMed] [Google Scholar]
- 10. Ng SK, Durkin S, Gilhotra JS. Rapid resolution of graft-versus-host-disease-related central serous chorioretinopathy. Semin Ophthalmol 2015; 30: 432–434. [DOI] [PubMed] [Google Scholar]
- 11. Gruszka A. Potential involvement of mineralocorticoid receptor activation in the pathogenesis of central serous chorioretinopathy: case report. Eur Rev Med Pharmacol Sci 2013; 17: 1369–1373. [PubMed] [Google Scholar]
- 12. Castro-Correia J, Countinho MF, Rosas V, et al. Long-term follow-up of central serous retinopathy in 150 patients. Doc Ophthalmol 1992; 1: 379–386. [DOI] [PubMed] [Google Scholar]