Abstract
Interpersonal and communication skills are 2 essential qualities of every physician. These are separate and distinct parts of the professional character of every physician. In pediatrics these abilities present even a higher impact.
We performed a survey-type prospective study based on questionnaires on 100 subjects, equally divided into 4 groups: 25 children, 25 pediatricians, 25 care-givers (parents, tutors, and relatives), and 25 health care staff, in a Tertiary Pediatric Clinic from Romania, between January 2017 and April 2017.
We included 100 participants in our study, equally divided into 4 groups: pediatric patients, pediatricians, care-givers, and health care staff. The 1st group comprised 25 children diagnosed with different chronic conditions, presenting the age between 5 and 14 years. The male gender predominated among the children (57%). The lowest general average score for “Communication” section was encountered among pediatricians group, 3.8, while the other 3 groups presented the same average score for this section, that is, 4.6. The children and the health care staff offered the same average score for “Transparency,” that is, 4.6, while the pediatricians offered a score of 4.5, and the care-givers of 4.7. The lowest average score for the item “Hospital environment” was given by the doctors, that is, 3.3, followed by care-givers with a score of 3.6, health care staff 3.7, and children with an average score of 3.8. All the 4 groups included in the study offered a general average of 4.9 out of 5 for the “Intercultural issues” section. The lowest average score for “Time management” section was offered by both children and pediatricians, that is, 4.1, while care-givers and health care staff had a slightly better perception regarding this item, offering 4.2 and 4.3, respectively.
The opinion among the 4 groups included in the study was generally similar regarding the 5 items assessed by our questionnaires. Therefore, the main aspects that need to be improved in the health care system in downward order are the following: hospital environment, time management, communication, transparency, and intercultural issues.
Keywords: children, communication skills, pediatrician
1. Introduction
Interpersonal and communication skills are 2 essential qualities of every physician. These are separate and distinct parts of the professional character of every physician. In pediatrics, these abilities present even a higher impact because the manner in which the physician informs the family about their child's disease has a decisive impact on the further doctor–patient and doctor–care-givers relationships.[1] If the physician owns both, communication and interpersonal skills, the child's parents or care-givers will become his partners in the following treatment of the child's illness leading therefore to a great clinical outcome.[2,3] It is very important to communicate effectively with the family, the care-givers, and the patient despite the pediatric age, in order to obtain a full compliance regarding the treatment, and therefore the patient's outcome. In Romania, the low socioeconomic and educational level of the population is an important issue when it comes to health problems. Unfortunately, these cases are not rare in our country, where still many people live in poor conditions, and many of them do not go to school. Every physician must learn to overpass this socioeconomic border and to make sure that he explains the diagnosis and all its implications in such manner that every patient and family member understands its appropriately the diagnosis, the treatment, the complications that can appear in the lack of treatment, and the burden of the disease itself for the patient independently by their educational level in order to obtain the expected clinical outcome. If the communication of the diagnosis is adequate and the physician emphasizes with the patients and his family, this will be the first major step toward the medical success. By gaining the parent's confidence and by building a doctor–patient–care-givers relationship based on trust, the physician will be able to gather important information regarding the anamnesis, the medical history, the onset of the disease, the symptoms of the patient, even those things that with a superior attitude he would have missed. Therefore, in Romania it is very important for a physician to develop the ability to “talk the patient's language” and to tailor communication to each individual in order obtain the needed trust.[1]
One of the greatest challenges for every physician regarding communication skills is represented by communicating the diagnosis of a severe condition with a poor prognosis. Therefore, it is crucial for the patient's managements that the care-givers understand properly all its implications. The physician must emphasize with the care-givers, must show compassion and understanding, but he must control his emotions in order to maintain the trust he earned.[1] The nonverbal communication represents probably the milestone in these situations because under these circumstances the care-givers’ pain and sufferance are so expressed that their understanding perception is impaired and it may seem that they do not hear anything. The diagnosis must be fully understood in order to assess it properly. Under these circumstances the physician must preserve his medical thinking. On one hand, he must never give false hopes, but on the other hand, he should not destroy all the care-givers’ hopes because in order to help the child, the care-givers must keep their calm and think as positively as possible. Therefore, the alliance between the physician and the child's care-givers is very important in every step of the clinical management. The child must also understand as much as possible the diagnosis and the therapeutic regimen that he is about to follow. Despite the small age, the physician must find a proper way to explain the condition to the child.
Based on all the facts mentioned above, it is very clear that the pediatrician must not only fulfill the needs of his patient, namely the child, but he also needs to satisfy the entire family's needs in order to build a relationship based on trust and respect that will eventually lead to the best outcome for the pediatric patient. Therefore, the aim of our study was to assess the relationship between pediatrician and patient based on the opinions of all those involved in the patient's care: pediatrician, patient, care-givers, and health care staff, and to identify the main concerns that need to be improved.
2. Material and method
We performed a survey-type prospective study based on questionnaires on 100 subjects, randomly included, equally divided into 4 groups: 25 children, 25 pediatricians, 25 care-givers (parents, tutors, and relatives), and 25 health care staff, in a Tertiary Pediatric Clinic from Romania, between January 2017 and April 2017. The questionnaires comprised 24 questions divided into 5 main sections, as it follows: communication (7 questions), transparency in communication (8 questions), hospital environment (2 questions), intercultural issues (2 questions), and time management (5 questions). The Communication section included questions regarding the support that is given to the patients, the respect received from the patients, the kind of support received from the medical team, the quality of patients’ life, the ease of doctor–patient conversation, of making appointment for checkups and in obtaining follow-up information and care. In the transparency section, the respondents were asked to rate the physician's ability to involve other doctors in patient's care, the grade of listening to patient's complaints and the way in which the explanations are given to a patient, the manner in which the patients are treated, the way providers keep patient informed about care, the level of privacy that the providers offer to the patients, and the manner in which the patients receive written information about symptoms or problems to look for after leaving the hospital. The 4th section of the questionnaire, Hospital Environment comprised questions regarding hospital's appearance and convenience (location, parking, hours, and office layout). In the intercultural issues section were evaluated the manner in which the pediatrician acted around patients and how the patients were treated. The last section of the questionnaire, time management, assessed the level of the ease in making appointments, in contacting the doctor when his/her office is closed and in speaking directly with the doctor by telephone during office hours, but also the delay in response time when an urgent problem occurs and the amount of waiting time in pediatrician's office. Every questionnaire also comprised a section with personal data, regarding gender, age, place of birth, city of residence, years of experience in case of paediatricians and health care staff, and role of the paediatriciens in the hospital. Each question had 5 answers and was quantified through a score between 1 (minimum) and 5 (maximum). The inclusion criteria for each group were the following: patients group – children with the age between 5 and 14 years, diagnosed with different chronic conditions for more than 6 months; pediatricians group – pediatricians or specialists from other domains that interacted with children (ie, intensive care, psychiatry, neurology, etc); care-givers group – parents, tutors, relatives of the pediatric patients included in the study; and health care staff – nurses that work in pediatric units. The exclusion criteria were: children under the age of 5 years or above the age of 14 years, length of the disease under 6 month, children whose care-givers refused to sign the informed consent, and participants who refused to signs the informed consent. The informed consent was obtained from every participant prior to inclusion in the study, except for pediatric patient, for whom the informed consent was signed by their care-givers. The study was performed in compliance with the principles of the Helsinki Declaration and was approved by the Ethics Committee of the University of Medicine and Pharmacy of Tîrgu Mureş (No 25/7 April 2017).
1.1. Statistical analysis
For data analysis, descriptive and inferential statistics elements were used. For the comparison of the central trend Mann–Whitney test was applied. For the value P the significance level was 0.05. Statistical analysis was performed using the program GraphPad Prism version 5.
3. Results
We included 100 participants in our study, equally divided into 4 groups: pediatric patients, pediatricians, care-givers, and health care staff. The 1st group comprised 25 children diagnosed with different chronic conditions, presenting the age between 5 and 14 years. The male gender predominated among the children (57%). According to the age, we subdivided this group into 3 subgroups: 5 to 7 years (33%), 8 to 11 years (20%), and 12 to 14 years (47%). Depending on the illness length, 47% of the cases presented a length between 1 and 3 years, 33% of the cases between 4 and 8 years, and only 7% of the children were diagnosed for more than 8 years. The 2nd group comprised 25 female pediatrician. Among them, 63% were over 45 years old, and 37% had the age between 36 and 45 years. Regarding the experience in the field of pediatrics, 63% of the pediatricians were working for more than 15 years, and 37% had a work experience between 5 and 10 years. The care-givers group comprised mostly women (81%), among which 34% had the age under 35 years, 53% were between 36 and 45 years old, and 13% above the age of 45 years. The health care staff group included only female nurses, among who 67% had the age above 45 years, 20% were between 36 and 45 years old, and 13% had an age ranging between 26 and 35 years. Their working experience in the field of pediatrics was as follows: 67% over 15 years of experience, 7% between 10 and 15 years, 13% between 5 and 10 years, and also 13% between 0 and 5 years of experience. In Fig. 1, we described the average scores for the 4th groups included in the study.
Figure 1.
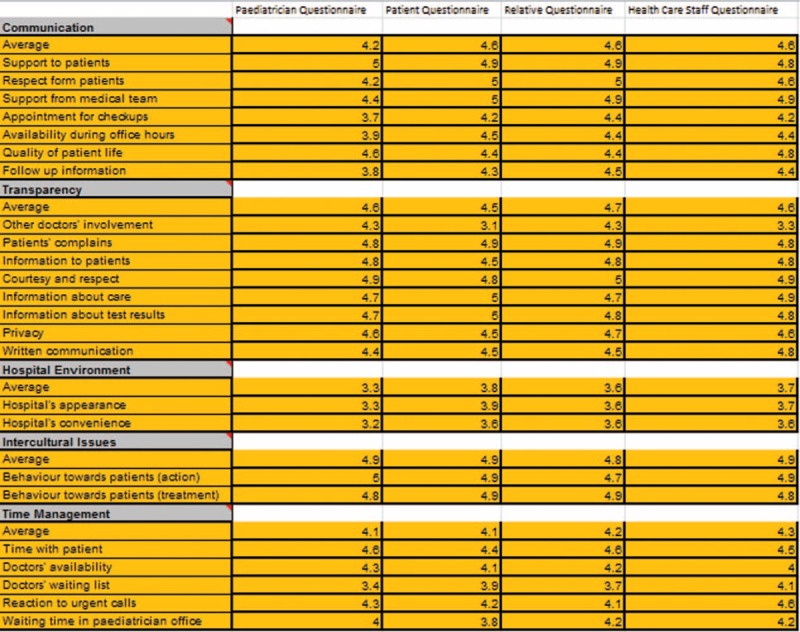
The average scores for the 4th groups.
The communication section assessed every participant's opinion regarding the support offered to the patient, respect in hospital, support offered by the medical team, quality of patient's life, doctor's availability, the ease in making appointments for checkups, and follow-up information. The lowest general average score for communication was encountered among pediatricians group, 3.8, while the other 3 groups presented the same average score for this section, that is, 4.6. The lowest average score was offered for the variable “ease in making appointments for checkups” by all the 4 groups, while the variable “support offered to patients” received the highest average score. We did not found any significant statistical difference between the 4 groups regarding the communication section (P = .11) (Fig. 2).
Figure 2.
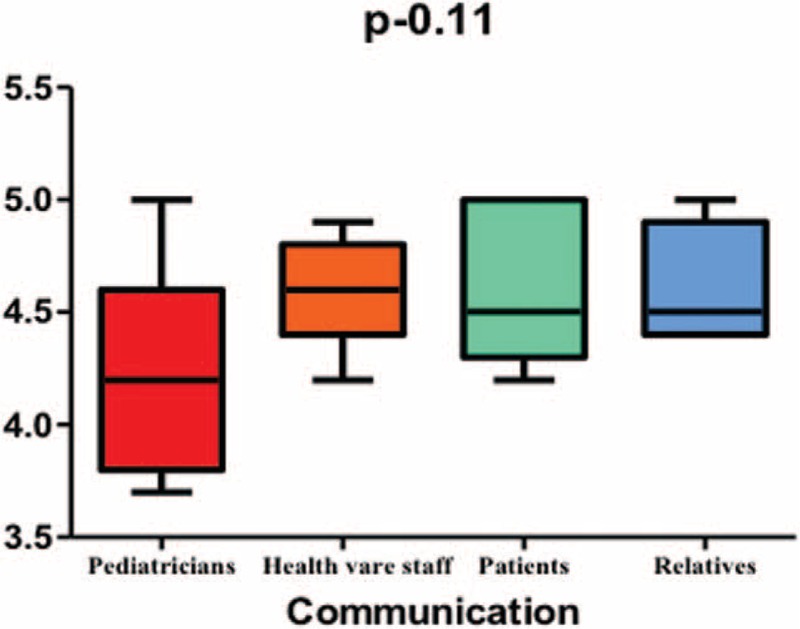
Communication skills in pediatrics.
The 2nd section of our questionnaires assessed transparency in communication regarding other doctor's involvement in care, efficiency and rapidity in solving patients’ complaints, information delivery to patient, courtesy and respect in the care process, privacy issues, and written information. The children and the health care staff offered the same average score for transparency, that is, 4.6, while the pediatricians offered a score of 4.5, and the care-givers of 4.7. The item “courtesy and respect” received the highest score among all 4 groups, while the item “involvement of other doctors in care” was offered the lowest score. We did not encounter any statistical difference between the 4 groups regarding the transparency section (P = .86) (Fig. 3).
Figure 3.
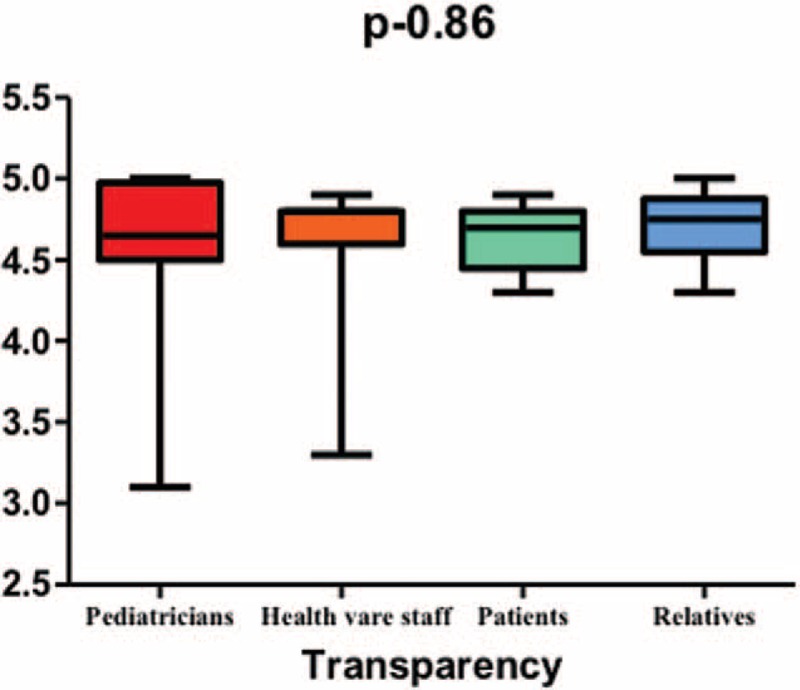
Transparency in pediatrics.
In the 3rd section, we assessed hospital environment regarding the appearance and the convenience of the hospital. The lowest average score for this item was given by the doctors, that is, 3.3, followed by care-givers with a score of 3.6, health care staff 3.7, and children with an average score of 3.8. We encountered a tendency toward statistical significance between the 4 groups (P = .05) (Fig. 4).
Figure 4.
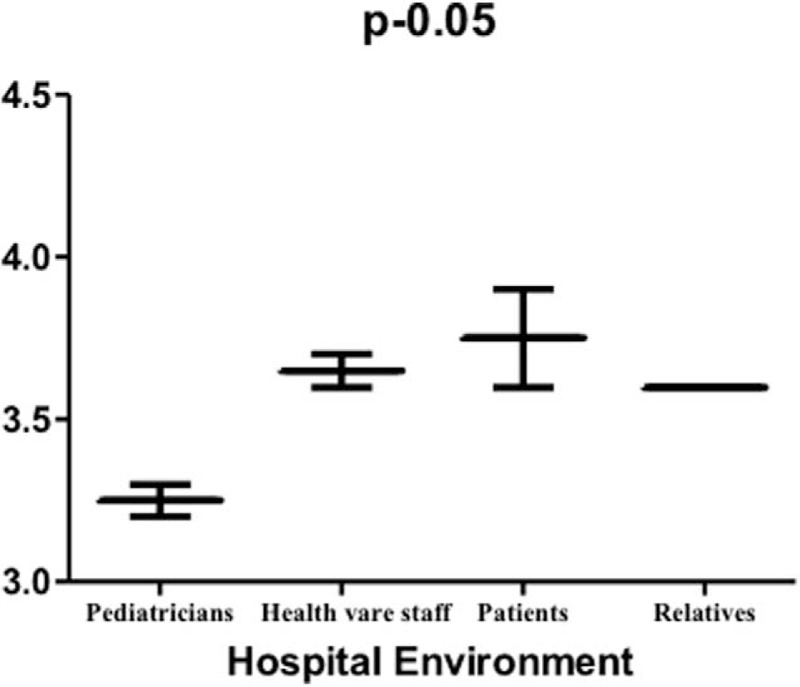
Hospital environment in pediatrics.
The 4th item of our questionnaire evaluated the intercultural issues regarding behavior toward patient in terms of action/attitude. All the 4 groups included in the study offered a general average of 4.9 out of 5, and therefore we did not identify any statistical difference between the 4 groups (P = .75) (Fig. 5).
Figure 5.
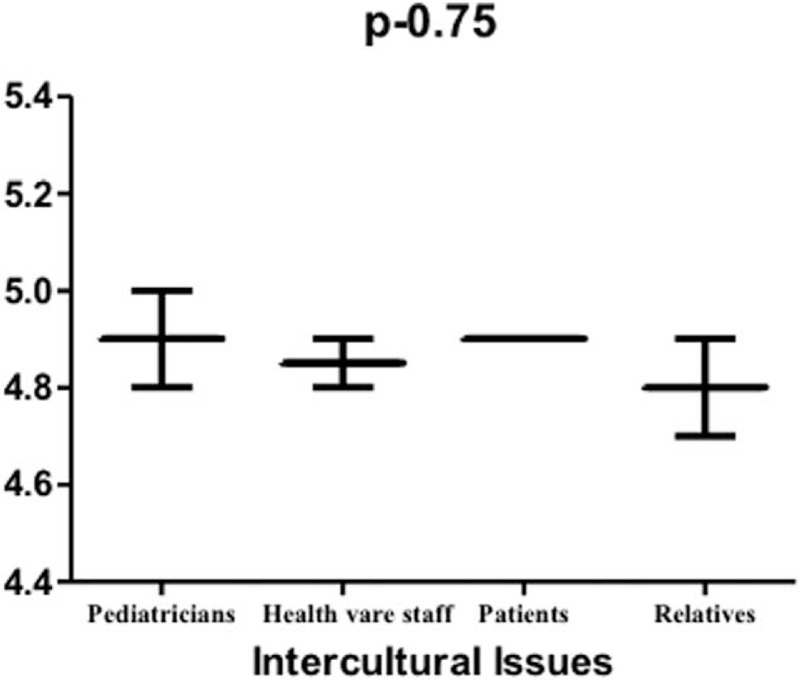
Intercultural issues in pediatrics.
The last section, called “time management,” assessed the pediatrician's skills in adequately managing his time. The lowest average score for this item was offered by both children and pediatricians, that is, 4.1, while care-givers and health care staff had a slightly better perception regarding this item, offering 4.2 and 4.3, respectively. We did not find any statistical difference regarding this item between the 4 groups included in our study (P = .079) (Fig. 6).
Figure 6.
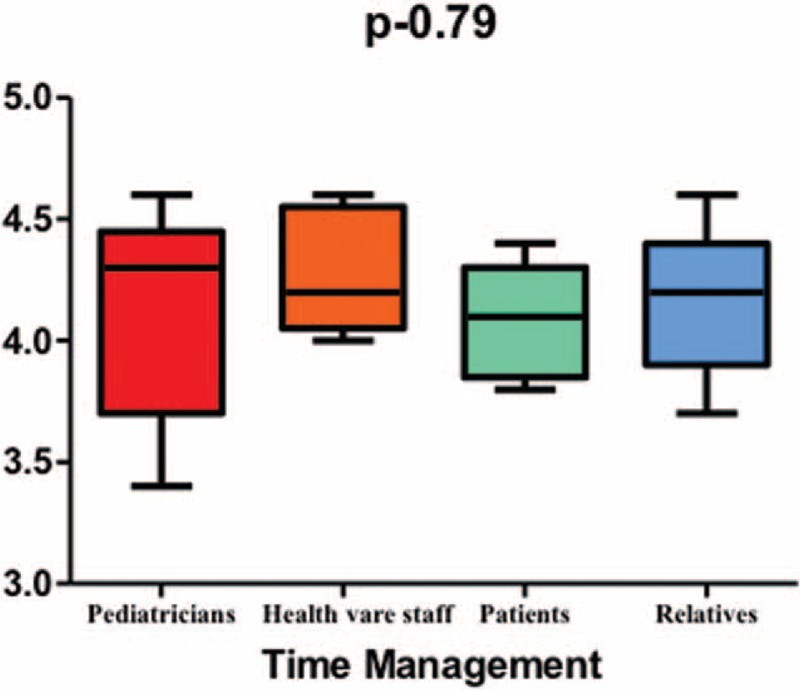
Time management in pediatrics.
4. Discussions
Effective communication between heath care providers and children or/and their care-givers represents a milestone in the management of every pediatric pathology, and it can be much more challenging than in case of adult patients. According to the American Academy of Pediatrics, effective communication is the cornerstone of care, the response to the needs of the patient and family dynamic, being centered on the patient's and family's care.[4] Generally, a medical relationship comprises 2 subject, but in case of pediatrics, this relationship is particular due to the fact that it involves 3 members: physician, parent, and child leading to an increased degree of communication difficulty. The physician–parent–child communication comprises 3 elements: informativeness referring to the quantity and quality of health information provided by the pediatrician; interpersonal sensitivity that concerns affective behaviors regarding the physician's attention to, and interest in the care-givers’ and pediatric patient's feelings and concerns; and partnership building explained by the manner in which the doctor invites the parent/care-givers and child to express their concerns, perspectives, and suggestions during the consultation.[5] In our study, informativeness was assessed within the transparency section being rated with the lowest score by the pediatricians,[4,5] and with the highest by the care-givers (4.7), who seemed more satisfied with the provided medical information than their children who offered only 4.6 for this item, likewise the health care staff. Also, interpersonal sensitivity was assessed by the intercultural issues section included in our questionnaire, and all the 4 groups offered the same score for this item, almost the maximum score (4.9) reflecting their satisfaction regarding the physician's attitude toward the patient's and family's needs. Nevertheless, every physician must be aware that he must improve continuously his affective behaviors. Also, the physicians must provide accessible information to their patients in order to avoid medicolegal actions. It was proven that between 35% and 70% of medicolegal actions are a result of one or multiple of the following factors: poor delivery of information, failure to understand the patient's and family's conceptions and opinions, failure to request and include patient's values into the medical strategy, and perceptions of desertion.[3,6–11]
Time management is not only a useful skill for the physician himself, but it is also a key strategy in order to gain patient's and family's respect leading eventually to better outcomes. Clinicians tend usually to use closed interviewing techniques in order to diminish the duration of the consult, by asking yes or no questions and hinder their patients’ needs to express their feelings, believes, opinions, and under some conditions, even to reveal the real reason for seeking consultation. All these facts will result in a wrong diagnosis, failure to cure the patient and poor health outcomes.[12–15] Therefore, the medical provider must be aware of the need to solicit child and family to express their concerns in order to gain their trust without the fear of losing his valuable time being proven that this fact does not increase the duration of the consultation, contrariwise it increases its utility.[6,16] We also assessed in our study the pediatricians’ skill in adequately managing his time in the last section of our questionnaire, named exactly “time management.” The lowest score for this item was offered by the children (4.1) proving that they are not satisfied with the amount of time their doctor allocates to their needs. It is also very important to underline that the same low score was also provided by the pediatricians themselves proving that they are aware of the fact that they are not able to manage properly their time leading to their patient's dissatisfaction. The acknowledgement of the fact that due to a variety of reasons they are not capable to manage their time is a real proof that they are willing to learn how to correct this issue and to gain their patient's satisfaction. Care-givers and health care staff expressed a slightly better perception regarding this item, offering scores of 4.2 and 4.3, respectively. Nevertheless, these are not satisfying opinions and they clearly claim for major improvement concerning the pediatricians’ time managements skills.
It is well known that working with children could be perhaps the most challenging among all the medical specialties. Similar surveys also reported that many children are dissatisfied with the manner their health care providers treat them while they are admitted.[17] Therefore, the current acute need for improvement regarding medical communication should be recognized among all universities, and undergraduate students should be provided with adequate tools for effective communication toward specific teaching techniques during their clinical internships.[18] Nevertheless there were reported several studies focused on students’ communication skills,[19,20] the information regarding the distinct complexities and the challenges of a 3-way interview between a child, their parent/care-giver and the physician, is still limited.[21–25] Nowadays health care communication is usually learned through trial and error technique[26] mostly due to the fact that medical school faculty members need themselves mentors to teach them communication skills.[27] Therefore, practicing physicians and undergraduate medical students need to learn these communication skills from mentors who are trained communicators, such as child life therapists,[28] child psychologists, or other nonphysician mentors like members of different academies specialized in health care communication.[29,30] It was proven by several studies that the most important predictive factors for an effective communication between physicians and patients/parents are: interest, caring, warmth, and responsiveness.[31–33]
The medical profession is probably one of the most challenging and rewarding of all, and in order to communicate effectively with patients/parents, across a broad range of socioeconomic and cultural backgrounds the physician must develop every day his communication and interpersonal skills. One of the most effective models of doctor–patient communication was defined in the Kalamazoo Consensus Statement and it comprises the following steps: build doctor–patient relationship, open the discussion, gather information, understand patient's perspective, share information, reach agreement on problems and plans, and provide closure.[34] Communication is probably the most common “procedure” in medicine, but it is unfortunately frequently neglected in the medical universities.[35] Nevertheless, most medical schools focus mostly on teaching medical procedures and techniques, health care communication skills should be provided to all medical students in every medical university even from the beginning in order to increase their practical abilities and to develop a proper doctor–patient relationship.
Nevertheless, we also must underline several limitations of our study, such as the fact that the subjects included in our study came from a single geographic area of the country and from a single area of South-Eastern Europe, as well as the relatively small number of subjects included in each of the 4 groups which could have potentially decreased the statistical power of our study. In addition, we also must improve our communication skills continuously. Likewise, this research needs to be extended to other geographic areas from our country, from Europe and even the world. Among the strengths of this study, we mention the accuracy in collecting the data from the subjects included in the study being performed by an experienced team.
To the best of our knowledge this is the first study in Romania performed on children and their parents/care-givers according to pediatric soft skills in communication which assessed multiple concerns regarding the health care system, such as pediatrician's communication skills, pediatrician's skills in managing his time, hospital environment, including 4 groups involved in health care: pediatric patients, parents/care-givers, pediatricians, and health care staff.
5. Conclusions
The opinion among the 4 groups included in the study was generally similar regarding the 5 items assessed by our questionnaires. Therefore, the main aspects that need to be improved in the health care system in downward order are the following: hospital environment, time management, communication, transparency, and intercultural issues. Even though the scores were relatively similar among the 4 groups included in the study, the minor differences encountered in each group express the individual needs for change and improvement, but also their dissatisfactions.
Acknowledgments
The authors thank Erasmus+ Programme of the European Union, “Softis-Ped-Softskills for Children's Health”, project number: 2016-1-RO01-KA203-024630 for the support.
Footnotes
Funding/support: This research was partially supported by Erasmus+ Programme of the European Union, “Softis-Ped-Softskills for Children's Health”, project number: 2016-1-RO01-KA203-024630.
The authors have no conflicts of interest to disclose.
References
- [1].Benson BJ. Domain of competence: interpersonal and communication skills. Acad Pediatr 2014;14(2 Suppl):S55–65. [DOI] [PubMed] [Google Scholar]
- [2].Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- [3].Levinson W, Roter DL, Mullooly JP, et al. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA 1997;277:553–9. [DOI] [PubMed] [Google Scholar]
- [4].Medical Home Initiatives for Children With Special Needs Project Advisory Committee. American Academy of Pediatrics. The medical home. Pediatrics 2002;110(1 Pt 1):184–6. [PubMed] [Google Scholar]
- [5].Street RL. Physicians’ communication and parents’ evaluations of pediatric consultations. Med Care 1991;29:1146–52. [DOI] [PubMed] [Google Scholar]
- [6].Levinson W. Doctor-patient communication and medical malpractice: implications for pediatricians. Pediatr Ann 1997;26:186–93. [DOI] [PubMed] [Google Scholar]
- [7].Hickson GB, Clayton EW, Githens PB, et al. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 1992;267:1359–63. [PubMed] [Google Scholar]
- [8].Beckman HB, Markakis KM, Suchman AL, et al. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med 1994;154:1365–70. [PubMed] [Google Scholar]
- [9].Hickson GB, Clayton EW, Entman SS, et al. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA 1994;272:1583–7. [PubMed] [Google Scholar]
- [10].Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care. JAMA 1994;272:1588–91. [PubMed] [Google Scholar]
- [11].Hobgood C, Tamayo-Sarver JH, Elms A, et al. Parental preferences for error disclosure, reporting, and legal action after medical error in the care of their children. Pediatrics 2005;116:1276–86. [DOI] [PubMed] [Google Scholar]
- [12].Young KT, Davis K, Schoen C, et al. Listening to parents. A national survey of parents with young children. Arch Pediatr Adolesc Med 1998;152:255–62. [PubMed] [Google Scholar]
- [13].Horwitz SM, Leaf PJ, Leventhal JM. Identification of psychosocial problems in pediatric primary care: do family attitudes make a difference? Arch Pediatr Adolesc Med 1998;152:367–71. [DOI] [PubMed] [Google Scholar]
- [14].Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. 1. Doctor-patient interaction and patient satisfaction. Pediatrics 1968;42:855–71. [PubMed] [Google Scholar]
- [15].Maguire P, Pitceathly C. Key communication skills and how to acquire them. BMJ 2002;325:697–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Street RL. Communicative styles and adaptations in physician-parent consultations. Soc Sci Med 1992;34:1155–63. [DOI] [PubMed] [Google Scholar]
- [17].Healthcare Commission. Healthcare Commission Patient Survey Report 2004 – young patients. http://www.nhssurveys.org/Filestore/CQC/YP_KF_2004.pdf [Accessed Jun 27, 2017. [Google Scholar]
- [18].Frost KA, Metcalf EP, Brooks R, et al. Teaching pediatric communication skills to medical students. Adv Med Educ Pract 2015;6:35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Keir A, Wilkinson D. Communication skills training in paediatrics. J Paediatr Child Health 2013;49:624–8. [DOI] [PubMed] [Google Scholar]
- [20].Gough JK, Frydenberg AR, Donath SK, et al. Simulated parents: developing paediatric trainees’ skills in giving bad news. J Paediatr Child Health 2009;45:133–8. [DOI] [PubMed] [Google Scholar]
- [21].Paul S, Dawson KP, Lanphear JH, et al. Video recording feedback: a feasible and effective approach to teaching history-taking and physical examination skills in undergraduate paediatric medicine. Med Educ 1998;32:332–6. [DOI] [PubMed] [Google Scholar]
- [22].Crossley J, Eiser C, Davies HA. Children and their parents assessing the doctor-patient interaction: a rating system for doctors’ communication skills. Med Educ 2005;39:820–8. [DOI] [PubMed] [Google Scholar]
- [23].Crossley J, Davies H. Doctors’ consultations with children and their parents: a model of competencies, outcomes and confounding influences. Med Educ 2005;39:807–19. [DOI] [PubMed] [Google Scholar]
- [24].Bosse HM, Schultz J-H, Nickel M, et al. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: a randomized controlled trial. Patient Educ Couns 2012;87:300–6. [DOI] [PubMed] [Google Scholar]
- [25].Bosse HM, Nickel M, Huwendiek S, et al. Peer role-play and standardised patients in communication training: a comparative study on the student perspective on acceptability, realism, and perceived effect. BMC Med Educ 2010;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hilden JM, Emanuel EJ, Fairclough DL, et al. Attitudes and practices among pediatric oncologists regarding end-of-life care: results of the 1998 American Society of Clinical Oncology survey. J Clin Oncol 2001;19:205–12. [DOI] [PubMed] [Google Scholar]
- [27].Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med 2003;18:685–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].American Academy of Pediatrics. Committee on Hospital Care. Child life services. Pediatrics 2000;106:1156–9. [PubMed] [Google Scholar]
- [29].Sourkes BM. Shaw RJ, DeMaso DR. Armfuls of time: the psychological experience of a child with a life-threatening illness. American Psychiatric Pub, Textbook of Pediatric Psychosomatic Medicine. Arlington: 2010. [Google Scholar]
- [30].Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ 1991;303:1385–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Simonian SJ, Tarnowski KJ, Park A, et al. Child, parent, and physician perceived satisfaction with pediatric outpatient visits. J Dev Behav Pediatr 1993;14:8–12. [PubMed] [Google Scholar]
- [32].Wofford MM, Wofford JL, Bothra J, et al. Patient complaints about physician behaviors: a qualitative study. Acad Med 2004;79:134–8. [DOI] [PubMed] [Google Scholar]
- [33].Heller KS, Solomon MZ. Initiative for Pediatric Palliative Care (IPPC) Investigator Team. Continuity of care and caring: what matters to parents of children with life-threatening conditions. J Pediatr Nurs 2005;20:335–46. [DOI] [PubMed] [Google Scholar]
- [34].Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med 2001;76:390–3. [DOI] [PubMed] [Google Scholar]
- [35].Levetown M. American Academy of Pediatrics Committee on Bioethics. Communicating with children and families: from everyday interactions to skill in conveying distressing information. Pediatrics 2008;121:e1441–60. [DOI] [PubMed] [Google Scholar]


