Abstract
Background & objectives:
Persons with schizophrenia use various coping strategies to adapt to distressing symptoms as well as to deal with daily stressors. Efforts have been made to explore alternative frameworks of coping using Ways of Coping Checklist (WCC) in persons with schizophrenia. This study aimed to re-analyze (factor analysis) the revised-WCC in Indian patients with residual schizophrenia. The secondary aim of the study was to evaluate the relationship of new framework of coping with psychopathology, disability and quality of life (QOL).
Methods:
Using a cross-sectional design, 103 patients with residual schizophrenia were assessed on WCC. A principal component analysis with varimax rotation was carried out to determine the factor structure of WCC.
Results:
Factor analysis yielded six factors which explained 51.6 per cent of the total variance and had acceptable-to-good internal consistency. Based on the type of items loaded, the six factors were named as follows: active and growth-oriented coping, accepting and fantasizing, reflective and confrontative coping, detachment, seeking social support and negative emotional coping. Patients most often used coping strategy of seeking social support, followed by ‘accepting and fantasizing’ and ‘active and growth-oriented coping’. Correlation analysis showed that those who more often used ‘active and growth-oriented coping’ had less negative symptoms, lower level of disability and higher spiritual and overall QOL.
Interpretation & conclusions:
The factor structure of revised-WCC was different among patients with schizophrenia when compared with individuals without mental illness, living in the community. It was evident that use of certain adaptive coping strategies was associated with better QOL and lower level of psychopathology. Our findings provided a framework of coping in patients with residual schizophrenia and suggested that promotion of certain coping strategies might be useful in improving the QOL and reduction of psychopathology in patients with schizophrenia.
Keywords: Assessment, coping, India, psychotic symptoms, residual schizophrenia, stressors
Patients with schizophrenia use various coping strategies to adapt to distressing symptoms as well as to deal with daily stressors1,2,3,4,5,6,7. These individuals frequently use avoidance or distraction coping, alcohol or drug use and social isolation5 to cope with symptoms5,6 and to reduce distress5. Several studies have also found that patients often use ‘help seeking’ or ‘seeking social support’ to cope with psychotic6 and non-psychotic symptoms and daily stressors5,8. However, persons with schizophrenia more often use ‘emotion-focused’ and ‘passive coping’ strategies to deal with stressful situations. They may avoid facing stressors rather than considering possible courses of action or attempting to solve problem1,9. These coping strategies have been considered ‘ineffectual’ and maladaptive as these correlate with greater distress10, lesser hope, lower self-esteem and more depressive symptoms7, increased symptom severity11 or relapse12 and poorer quality of life (QOL)13. It has also been suggested that these individuals have a restricted repertoire of coping strategies that they employ when under stress7.
Coping strategies differ from stressor to stressor and patients of schizophrenia may face certain stressors that might be beyond their control. Some efforts have been made to explore alternative frameworks of coping in persons with schizophrenia. Lysaker et al14 attempted to rationally devise coping subscales from the items of the Ways of Coping Checklist (WCC) and showed internal consistency of the subscales, namely, acting, considering, ignoring, resigning, positive reappraising and self-soothing. They later established coping profiles and tested their correlation with hope, self-esteem, symptoms and functioning7. However, the framework proposed by another study conducted in a small sample of outpatients re-analyzed the original WCC scale and generated six subscales, with hope-related coping being associated with better QOL15. The existing factor analytic studies have been conducted in either heterogeneous samples or in persons with acute psychosis. No attempt has been made to study the factor structure in patients with residual symptoms who encounter difficulties that might be partly different from those with acute symptoms.
In addition to illness-related factors, cross-cultural differences have also been noted in coping in general16, and in coping with symptoms of schizophrenia17. Thus, cross-cultural differences might affect the choice of coping strategies, acceptability of certain ways of coping and individual means to employ those strategies. In India, despite the diversity in language, customs and rituals, collectivism is the common thread across sub-cultures that influences coping and decision-making of individuals. Seeking help and advice from other members in one's family or community group is commonly resorted to during difficult times18. Thus, it becomes imperative to study the framework of coping in schizophrenia in a cultural context. This study was aimed to carry out an exploratory factor analysis of WCC and devise a new and relevant framework of coping in patients with residual schizophrenia in the context of collectivistic Eastern culture. The secondary aim was to evaluate the relationship of new framework of coping with psychopathology, disability and QOL.
Material & Methods
This cross-sectional study was conducted in the outpatient clinic of department of Psychiatry, Postgraduate Institute of Medical Education and Research, a tertiary teaching hospital in Chandigarh, India, during January to December 2008. The study was approved by the Institute's Research and Ethics Committee, and all patients were recruited after obtaining written informed consent. Besides evaluation of coping, the study also involved assessment of psychopathology, various aspects of QOL and disability in patients with schizophrenia, data of which have already been published8,19,20. The detailed methodology is available elsewhere8,19,20.
For this study, the data of psychopathology as assessed on Positive and Negative Syndrome Scale (PANSS)21, data of disability as measured by the Indian Disability Evaluation Assessment Scale (IDEAS)22, QOL as assessed on the World Health Organization QOL's (WHOQOL) Spirituality, Religiousness and Personal Belief scale (SRPB)23 and coping as assessed by WCC (revised)24, were used.
Ways of Coping Checklist (WCC) (revised): The WCC (revised) developed by Folkman and Lazarus24,25,26 consists of a checklist of 66 items where each item has a brief description of a cognitive and behavioural strategy for coping with stressful events. The responder is asked to keep a specific stressful situation in mind that he/she may have experienced in the past week. Rating is done on a 4-point scale with higher scores indicating more frequent use of that particular strategy by the individual while dealing with the specific stressful situation. A factor analytic study of the WCC in a middle-aged community sample yielded eight coping subscales which included 50 items, namely, confrontive coping, distancing, self-controlling, seeking social support, accepting responsibility, escape-avoidance, planful problem-solving and positive reappraisal. The internal consistency of the coping subscales thus derived was good, with alpha value ranging from 0.61 to 0.7926.
Patients who had self-proclaimed proficiency in reading and understanding English were asked to use the WCC as a self-report measure. For the remaining patients, Hindi-translated version was used. Some of the patients, who were not proficient in Hindi, were provided assistance by giving substitute Punjabi words. Additionally, the investigators were flexible with the choice of words in using colloquial terms to convey the meaning, depending on their assessment of the patient's level of literacy and understanding so as to improve the comprehensibility of the items.
Method: Patients with residual schizophrenia as diagnosed by the Structured Clinical Interview for Axis-1 DSM-IV Disorders – Clinical Version27 of either gender, aged 20-60 yr, of any religion, without any other psychiatric comorbidity including substance dependence (except nicotine) were included in the study. Patients with any major or debilitating physical comorbidity were excluded. Patients were recruited using purposive sampling i.e., patients fulfilling the inclusion criteria were approached for consent and those who gave written informed consent were enrolled in the study. A total of 120 patients with residual schizophrenia were approached, of whom 103 were included in the study. Seventeen patients were excluded because they either did not meet the inclusion and/or fulfilled the exclusion criteria.
Statistical analysis: The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 14.0 (SPSS Inc., Chicago, Illinois, USA). Mean, standard deviation (SD) and frequencies were calculated for the socio-demographic and clinical data, and PANSS. Exploratory factor analysis was carried out by the method of principal component analysis so as to determine the minimum number of factors that would account for the maximum variance in the data. Orthogonal rotation was used so as to generate factors independent of one another. Sampling adequacy for the factor analysis was determined by the Kaiser–Meyer–Olkin measure28 of sampling adequacy and Bartlett's test of Sphericity was used to test the null hypothesis.
The optimum number of factors was determined using the Kaiser–Guttman rule29, and only factors with Eigenvalue of more than one were included initially. A scree plot was also generated simultaneously to determine the optimal number of factors. In addition, the existing literature was also considered before accepting the final factor solution. Only those factors with three or more items with a loading of ≥0.4 were considered. In case a variable loaded ≥0.4 on two or more factors, it was assigned to the factor where it had the highest loading. The internal consistency of the derived factors was evaluated using Cronbach's alpha. Weighted mean scores for each of the factor were calculated by descriptive analysis. Pearson's correlation analysis was conducted to determine associations between the new factor structure and PANSS, IDEAS and WHOQOL SRPB scores.
Results
The mean age of patients was 34.36±8.26 yr; 62.1 per cent patients (n=64) were male, slightly less than half were single (n=48, 46.6%), more than half of them had more than 10 yr of formal education (n=56, 54.3%) and were married and living with their spouses (n=46, 44.7%). Majority of the participants were Hindu by religion (n=73, 71%) and remaining were Sikhs (n=30; 29%). Forty five patients (43.7%) were employed while the remaining were unemployed, students or engaged in household work (including homemakers). About half of the patients belonged to a joint or extended family setup (51.5%).
The mean age at onset was 22.76±5.64 yr. The total duration of illness ranged from 36 to 396 months with a mean of 138.96±86.76 months. In terms of psychopathology, the mean positive subscale score on PANSS was 9.19±2.95, negative subscale score was 17.09±5.37, general psychopathology score was 23.16±5.76 and the total PANSS score was 49.45±11.31.
Factor analysis of WCC
Determining sampling adequacy: The Kaiser–Meyer–Olkin measure of sampling adequacy for the sample was 0.706. The Bartlett's test of Sphericity was used to test the null hypothesis that the correlation matrix was an identity matrix i.e., the variables were not correlated. The approximate Chi-square statistics for the current data was 4764 (df=2145; P<0.001), suggesting that factor analysis could be carried out with the data. These results indicated that factor analysis was appropriate for the data. Based on the Kaiser–Guttman rule, the initial factor analysis yielded 16 factors with Eigenvalue more than one, which explained 73.11 per cent of the total variance in the sample. The scree plot indicated tailing after seven factors.
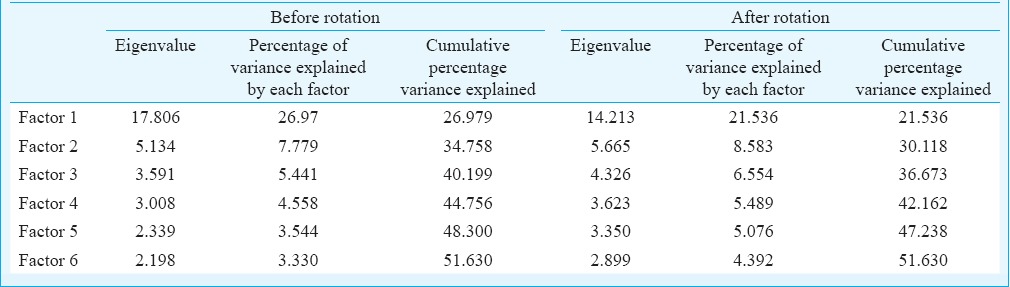
Multiple factor analyses were run to decide about the best fit model, which retained the maximum number of items of WCC, explained maximum variance and each factor had at least three or more items. Finally, a six-factor model was accepted, which explained 51.63 per cent of variance. Table I shows the variance explained by each of the six factors before and after rotation.
Table I.
Six-factor model depicting the eigenvalue and percentage of variance explained
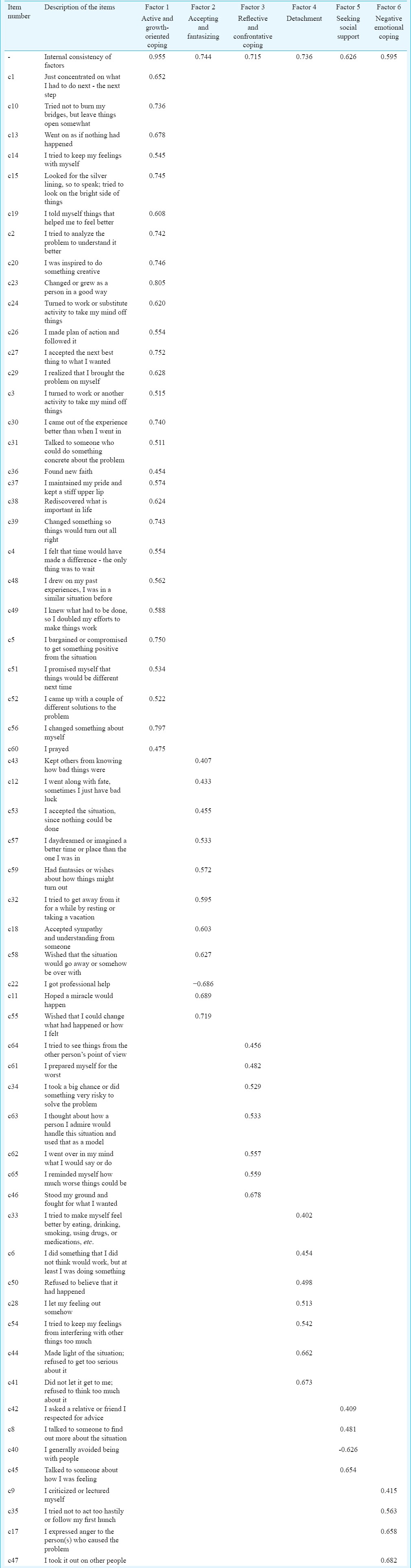
Twenty eight items were loaded on factor 1, 11 items on factor 2, 7 items on factor 3 and factor 4 each and 4 items each loaded on factor 5 and factor 6 (Table II). Five items did not load on any of the factors and these items were dropped. Based on the type of items loaded, the six factors were named as active and growth-oriented coping, accepting and fantasizing, reflective and confrontative coping, detachment, seeking social support and negative emotional coping. The first factor was designated as ‘active and growth-oriented coping’ because it included behavioural and cognitive ways in which a person actively tries to decrease his/her distress by redefining the situation with focus on the positive aspects or actively tries to resolve a problem with faith on God. The second factor was termed ‘accepting and fantasizing’, as it represented acceptance of situation and fantasy about something happening on its own to resolve the problem. The third factor was designated ‘reflective and confrontative’, because it included items suggesting active effort on the part of the person to reflect on the circumstances and face the situation. The fourth factor was designated as ‘detachment’ because it included ways in which a person distances himself/herself from the stressful situation. The fifth factor was ‘seeking social support’ that suggested the use of actively exploiting social network for emotional and logistic support. The sixth factor was named as ‘negative emotional coping’ as it predominantly included items suggesting expression of anger towards oneself and others.
Table II.
Factor analysis with different factor loading on varimax rotation and internal consistency
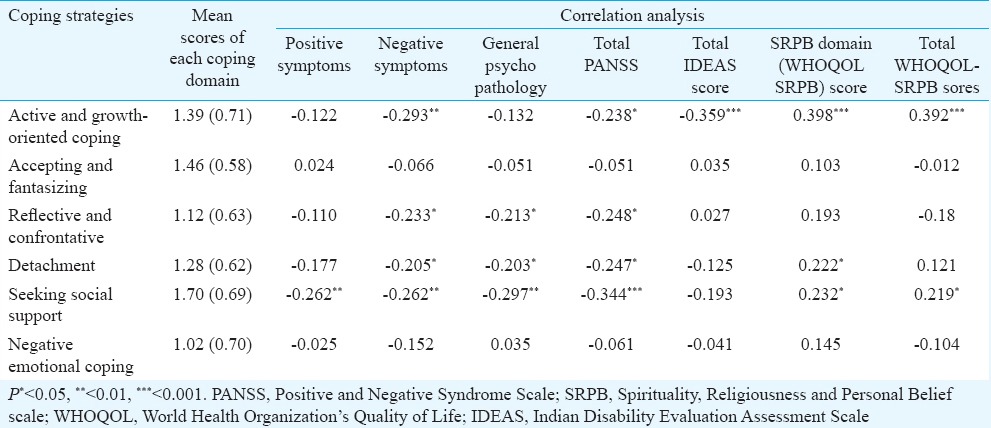
Weighted scores were calculated for all the six factors. Equal weight was given to each item. Thus, the scores calculated were sum of the item scores in each factor divided by the number of items in that factor. As the item 40 had negative loading, the scoring was reversed for this item. Table III depicts the mean scores of the six coping strategies. These findings suggested that patients most often used coping strategy of seeking social support, followed by ‘accepting and fantasizing’ and ‘active coping and growth-oriented coping’. Correlation analysis showed that those who more often used ‘active coping and growth-oriented coping’ had less negative symptoms, lower level of disability and higher spiritual and overall QOL. Those who more often used reflective and confrontative, detachment and seeking social support as a coping strategy had lower level of negative symptoms and general psychopathology and resultant lower total PANSS scores. Additionally, use of seeking social support was associated with lower level of positive symptoms and higher QOL, and use of detachment was associated with higher SRPB QOL.
Table III.
Mean scores of the coping strategies and results of correlation analysis
Discussion
In this study the factor structure of WCC was evaluated in patients with schizophrenia having residual psychopathology. The final exploratory model of coping derived in the present study had six factors from 61 items. The total number of items which were retained in the factor analysis was more than the number of items (50 items) included in the eight-factor model of WCC (revised) in the community sample26. The six factors derived in the present study had acceptable-to-good internal consistency30 with Cronbach's alpha ranging from 0.59 to 0.95. This was high compared to the internal consistency of the factors derived by Folkman and Lazarus26.
Factor 1 of the present study was considered nearest to the concepts of ‘planful problem-solving’ and ‘positive reappraisal’ of WCC. The strategies representing this factor allow a person to learn and grow while dealing with the situation. Theoretically, active and growth-oriented coping should contribute to resolution of the stress response and also may promote long-term benefits; and hence it is an adaptive coping technique31. This factor also had some items in common with acting and positive reappraisal subscales devised by Lysaker et al14. This factor included religion-/faith-based coping strategies. The second factor included items which represented coping through wishful thinking i.e., expecting the situation to improve on its own. This way of coping can be considered maladaptive as, though it may reduce emotional distress in the short term, it may affect the psychological health adversely in the long term31. The third factor ‘reflective and confrontive’ included active efforts on the part of the patient to reflect on the situation and face the problem head-on had few common items with the ‘self-controlling’ and ‘confrontive’ factors defined in the original factor analysis by Folkman and Lazarus26, and with the ‘considering’ factor generated by Lysaker et al14. The fourth factor ‘detachment’ also reflects adaptive coping in the realm of psychopathology. This factor includes items which actually reflect efforts of the patients to distance themselves from their symptoms. The factor ‘seeking social support’ was similar to that of the original scale except the noteworthy difference that the item ‘I got professional help’ did not load on this factor in our study. This can be explained in two ways, social/cultural and illness related. First, in a collectivistic society like ours, family and friends form the strongest and most readily available social support resource. The availability of social resources for patients with schizophrenia has been speculated and supported in studies from India32,33. All our patients were living with their spouses or families of origin or both. Hence, it would be natural to seek help from members of one's community rather than seek help from professionals. In addition, professional help may not be readily available and accessible due to financial constraints. The second explanation may be pertaining to the illness itself. Seeking professional help might require greater initiative on the part of the individual and better social skills when compared to seeking help from relatives and friends. In patients with schizophrenia, negative symptoms and social skills deficit might hamper such an active strategy. The last factor included items which reflected the expression of negative emotion of anger towards oneself or others and could be considered as maladaptive coping.
In general, factors 1, 3, 4 and 5 represented adaptive coping strategies and factors 2 and 6 represented maladaptive coping strategies. It was found that use of active coping, seeking social support, reflective and confrontive coping were associated with lower level of psychopathology and disability, and the first two were also associated with higher QOL. Active and growth-oriented coping had strong positive correlation with QOL. These findings were similar to those by Rudnick and Martins15, where activity coping was associated with better QOL, and support coping was associated with lower level of symptoms. In the study by Lysaker et al7, the patients with considering and acting coping profiles, which was closest to the active and reflective coping derived in the present study, had significantly greater levels of hope and self-esteem. Furthermore, active coping was strongly related to spiritual QOL. This may be partly explained by the presence of faith-based items in the first factor. Also, it suggests that persons with strong spiritual or religious belief systems may find strength in their beliefs so as to face stressful situations, reappraise these and employ problem-solving techniques8 as these beliefs provide a sense of meaning, perceived control and predictability. Use of social support has been proposed to have a buffering effect in the face of stressful situations34. This was supported by findings of the present study as reflected in lower psychopathology and disability.
It was found that seeking social support was the most frequently employed strategy by patients with residual schizophrenia. Other studies from India have also shown that help seeking is the most commonly used coping strategy. Raguram5 found that direct help was sought by patients with non-psychotic symptoms, while distraction and increasing socialization were used by patients to cope with hallucinations. Singh et al6 reported that help seeking, mainly medical help, was common in patients with hallucinations. However, both the studies focused on coping with specific symptoms of schizophrenia. The second most commonly used strategy in the present study was that of ‘accepting and fantasizing’, similar to other studies1,9. In our study, it was also found that active and growth-oriented coping was used frequently by patients, which suggested that, at the time of distress, patients attempted to find positive meaning, resolve the problem and additionally relied on God for the solution. High reliance on ‘faith/God’ reflects the cultural variations in using coping strategies. It is in general suggested that compared to the West, people from the East more commonly rely on religious-based coping35.
Our study had certain limitations. This study had a cross-sectional design, so causal inferences could not be drawn. In addition, the sample size was small. As the study was conducted in patients with residual symptoms and those residing in the community, it would not be possible to generalize the findings to patients suffering from active symptoms or hospitalized patients.
In conclusion, our study conducted in outpatients with residual schizophrenia provided a framework of coping in a cultural context. The findings supported the binary model of adaptive and maladaptive coping. Further, the findings also suggested that culture influenced the framework of coping as well as the employment of specific coping strategies.
Footnotes
Conflicts of Interest: None.
References
- 1.Farhall J, Gehrke M. Coping with hallucinations: Exploring stress and coping framework. Br J Clin Psychol. 1997;36(Pt 2):259–61. doi: 10.1111/j.2044-8260.1997.tb01411.x. [DOI] [PubMed] [Google Scholar]
- 2.Hultman CM, Wieselgren IM, Ohman A. Relationships between social support, social coping and life events in the relapse of schizophrenic patients. Scand J Psychol. 1997;38:3–13. doi: 10.1111/1467-9450.00002. [DOI] [PubMed] [Google Scholar]
- 3.Kumar S, Thara R, Rajkumar S. Coping with symptoms of relapse in schizophrenia. Eur Arch Psychiatry Neurol Sci. 1989;239:213–5. doi: 10.1007/BF01739656. [DOI] [PubMed] [Google Scholar]
- 4.Mueser KT, Valentiner DP, Agresta J. Coping with negative symptoms of schizophrenia: Patient and family perspectives. Schizophr Bull. 1997;23:329–39. doi: 10.1093/schbul/23.2.329. [DOI] [PubMed] [Google Scholar]
- 5.Raguram R. An exploratory study of coping styles in schizophrenic patients. Indian J Psychiatry. 1993;35:22–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Singh G, Sharan P, Kulhara P. Coping with hallucinations in schizophrenia: A correlational study. Hong Kong J Psychiatry. 2002;12:5–11. [Google Scholar]
- 7.Lysaker P, Tsai J, Hammoud K, Davis LW. Patterns of coping preference among persons with schizophrenia: Associations with self-esteem, hope, symptoms and function. Int J Behav Consult Ther. 2009;5:192–208. [Google Scholar]
- 8.Shah R, Kulhara P, Grover S, Kumar S, Malhotra R, Tyagi S. Relationship between spirituality/religiousness and coping in patients with residual schizophrenia. Qual Life Res. 2011;20:1053–60. doi: 10.1007/s11136-010-9839-6. [DOI] [PubMed] [Google Scholar]
- 9.Wilder-Willis KE, Shear PK, Steffen JJ, Borkin J. The relationship between cognitive dysfunction and coping abilities in schizophrenia. Schizophr Res. 2002;55:259–67. doi: 10.1016/s0920-9964(01)00211-0. [DOI] [PubMed] [Google Scholar]
- 10.Cooke M, Peters E, Fannon D, Anilkumar APP, Aasen I, Kuipers E, et al. Insight, distress and coping styles in schizophrenia. Schizophr Res. 2007;94:12–22. doi: 10.1016/j.schres.2007.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meyer B. Coping with severe mental illness: Relations of the brief COPE with symptoms, functioning, and well-being. J Psychopathol Behav Assess. 2001;23:265–77. [Google Scholar]
- 12.Pallanti S, Quercioli L, Pazzagli A. Relapse in young paranoid schizophrenic patients: A prospective study of stressful life events, P300 measures, and coping. Am J Psychiatry. 1997;154:792–8. doi: 10.1176/ajp.154.6.792. [DOI] [PubMed] [Google Scholar]
- 13.Ritsner M, Ben-Avi I, Ponizovsky A, Timinsky I, Bistrov E, Modai I. Quality of life and coping with schizophrenia symptoms. Qual Life Res. 2003;12:1–9. doi: 10.1023/a:1022049111822. [DOI] [PubMed] [Google Scholar]
- 14.Lysaker PH, Johannesen J, Lancaster RS, Davis LW, Zito W, Bell MD. Assessing coping in schizophrenia – A rationally devised scoring scheme to assess coping in schizophrenia. Int J Psychosoc Rehabil. 2004;8:73–83. [Google Scholar]
- 15.Rudnick A, Martins J. Coping and schizophrenia: A re-analysis. Arch Psychiatr Nurs. 2009;23:11–5. doi: 10.1016/j.apnu.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Kuo BCH. Culture's consequences on coping: Theories, evidences, and dimensionalities. J Cross Cult Psychol. 2011;42:1066–83. [Google Scholar]
- 17.Kumar S, Thara R, Rist F. Coping with symptoms of schizophrenia: A cross-cultural comparison. Indian J Soc Psychiatry. 1994;10:4–10. [Google Scholar]
- 18.Chadda RK, Deb KS. Indian family systems, collectivistic society and psychotherapy. Indian J Psychiatry. 2013;55(Suppl 2):S299–309. doi: 10.4103/0019-5545.105555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah R, Kulhara P, Grover S, Kumar S, Malhotra R, Tyagi S. Contribution of spirituality to quality of life in patients with residual schizophrenia. Psychiatry Res. 2011;190:200–5. doi: 10.1016/j.psychres.2011.07.034. [DOI] [PubMed] [Google Scholar]
- 20.Grover S, Shah R, Kulhara P, Malhotra R. Internal consistency & validity of Indian Disability Evaluation and Assessment Scale (IDEAS) in patients with schizophrenia. Indian J Med Res. 2014;140:637–43. [PMC free article] [PubMed] [Google Scholar]
- 21.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 22.Government of India. Guidelines for Evaluation and Assessment of Mental Illness and Procedure for Certification. Office of the Chief Commissioner for Persons with Disabilities, Ministry of Social Justice and Empowerment, Government of India. 2002. [accessed on April 10, 2017]. Available from: http://www.ccdisabilities.nic.in/page.php?s=large&t=yb&p=guide_mental .
- 23.WHOQOL SRPB Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med. 2006;62:1486–97. doi: 10.1016/j.socscimed.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 24.Folkman S, Lazarus RS. Manual for the ways of coping questionnaire. Palo Alto, CA: Consulting Psychologists Press; 1988. [Google Scholar]
- 25.Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- 26.Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21:219–39. [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M. Structured clinical interview for Axis-1 DSM-IV disorders – Clinical version (SCID-CV) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 28.Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39:31–6. [Google Scholar]
- 29.Jolliffe IT. Principal component analysis. Springer series in statistics. 2nd ed. New York: Springer; 2002. [Google Scholar]
- 30.George D, Mallery P. SPSS for windows step by step: A simple guide and reference. 11.0 update. 4th ed. Boston: Allyn & Bacon; 2003. [Google Scholar]
- 31.Bartram D, Gardner D. Coping with stress. In Practice. 2008;30:228–31. [Google Scholar]
- 32.Thara R, Padmavati R, Srinivasan TN. Focus on psychiatry in India. Br J Psychiatry. 2004;184:366–73. doi: 10.1192/bjp.184.4.366. [DOI] [PubMed] [Google Scholar]
- 33.Verghese A, John JK, Rajkumar S, Richard J, Sethi BB, Trivedi JK. Factors associated with the course and outcome of schizophrenia in India. Results of a two-year multicentre follow-up study. Br J Psychiatry. 1989;154:499–503. doi: 10.1192/bjp.154.4.499. [DOI] [PubMed] [Google Scholar]
- 34.Buchanan J. Social support and schizophrenia: A review of the literature. Arch Psychiatr Nurs. 1995;9:68–76. doi: 10.1016/s0883-9417(95)80003-4. [DOI] [PubMed] [Google Scholar]
- 35.Bjorck JP, Cuthbertson W, Thurman JW, Lee YS. Ethnicity, coping, and distress among Korean Americans, Filipino Americans, and Caucasian Americans. J Soc Psychol. 2001;141:421–42. doi: 10.1080/00224540109600563. [DOI] [PubMed] [Google Scholar]


