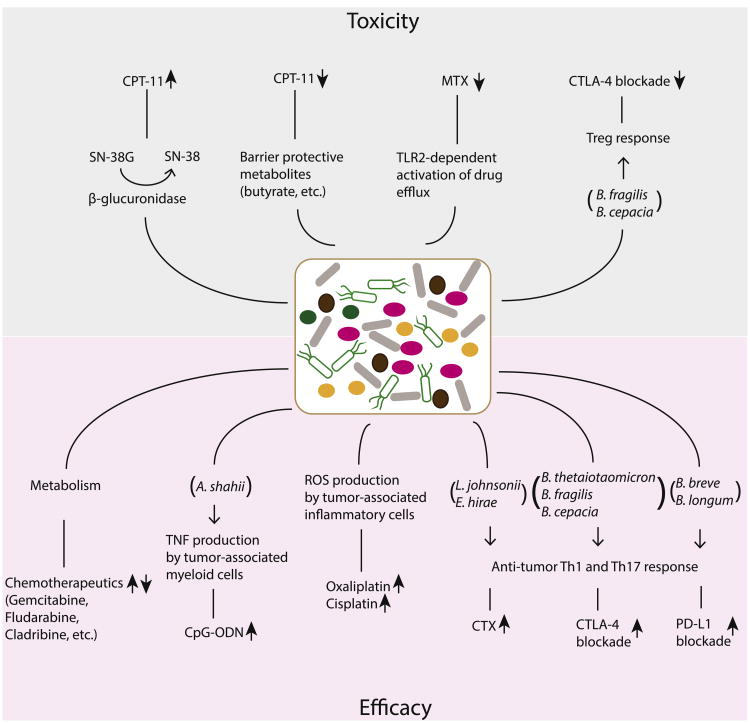
Fig 3.
Interaction between bacteria and anticancer drugs. The microbiota influences anticancer drug efficacy and toxicity through direct or indirect mechanisms. Bacterial β-glucuronidases convert SN-38G to active SN-38, leading to the toxic effect of CPT-11. Microbiota can generate barrier-protective metabolites such as butyrate and activate TLR2/drug efflux response to attenuate CPT-11 and MTX toxicity, respectively. B. fragilis (via Treg response) and B. cepacia can ameliorate CTLA-4-blockade–induced intestinal inflammation. On the other hand, bacteria profoundly influence the efficacy of chemotherapeutics via a metabolic route. Microbial-driven ROS production by tumor-associated inflammatory cells promotes the antitumor effect of oxaliplatin and cisplatin. A. shahii induces TNF production by tumor-associated myeloid cells, which contributes to the antitumor effect of CpG-ODN. Efficacies of CTX, CTLA-4 blockade, and PD-L1 blockade can be enhanced by specific and distinct bacteria. CpG-ODN, CpG-oligonucleotide; CPT, irinotecan; CTLA, cytotoxic T-lymphocyte–associated protein 4; MTX, methotrexate; ROS, reactive oxygen species; TLR, toll-like receptor; TNF, tumor necrosis factor.