Abstract
Background:
The Functional Movement Screen (FMS™) is a widely used seven-test battery used by practitioners working in sport medicine. The FMS™ composite score (sum of seven tests) in soccer athletes from different competitive levels has been well explored in literature, but the specific movement deficits presented by young high competitive level players remains unclear.
Purpose:
The aim of the present study was to provide a detailed description of the performance of elite young soccer players (age 14-20 years) on the FMS™ testing battery.
Study design:
Cross-sectional observational study.
Methods:
One-hundred and three young soccer players (14-20 years) from a premier league club were assessed by two experienced raters using the FMS™ testing battery. FMS™ composite score, individual-test scores and asymmetries were considered for analysis, and comparisons between age categories were performed.
Results:
FMS™ composite scores ranged from 9 to 16 points (median=13 points). 82% of the athletes had a composite score ≤14 points, and 91% were classified into the “Fail” group (score 0 or 1 in at least one test). Almost half of athletes (48%) had poor performance (i.e., individual score < 2) in “deep squat” test. Most of athletes in the younger categories (under-15 and under-16) had poor performance in the “trunk stability push-up” test (70%) and in the “rotary stability” test (74%). Asymmetry in at least one of five unilateral FMS™ tests was found in 65% of athletes.
Conclusion:
High-performance young soccer players have important functional deficits, especially in tasks involving deep squat and trunk stability, as well as high prevalence of asymmetry between right and left body side.
Level of evidence:
3a.
Keywords: Athletic performance, FMS™, human movement, injury prevention, movement system, soccer
INTRODUCTION
The Functional Movement Screen (FMS™) is a movement-competency-based test battery aimed to provide a clinically interpretable measure of “movement quality”. For a comprehensive review of the screening test battery and it's scoring see Cook et al.1,2 Despite the subjectivity on the visual assessment of human movement, the FMS™ presents acceptable levels of inter-rater and intra-rater reliability.3 Therefore, the FMS™ has been used as a screening tool for developing exercise programs focused on injury prevention, rehabilitation, and performance enhancement in sports. Kiesel et al.4 first examined the ability of the FMS™ to predict injury in American football players. Thereafter, the use of the FMS™ has spread to a range of sports, and athletes with a FMS™ composite score ≤ 14 points are usually classified as those with high injury risk. However, systematic reviews have provided conflicting conclusions on this cut-point.5,6
The FMS™ has also attracted considerable attention by researchers as evidenced by the increasing number of publications involving recreational,7 college,8 and Olympic9 athletes from different sports. Regarding soccer, McCall et al.10 investigated strategies related to injury prevention adopted by premier league teams in different countries of Europe, America and Oceania; and results indicated that FMS™ is the most commonly used method to identify risk factors for non-contact injuries. In addition, there are studies describing the FMS™ composite score of male soccer players in different competitive levels, such as professionals,11 semi-professionals,12 veterans,13 college,14 and adolescent15,16 athletes.
Portas et al.16 performed a cross-sectional study with 1,163 young soccer players (age 8-18 years) and demonstrated that most athletes presented composite scores ≤14 points. However, since the injury predictive value of the FMS™ composite score is inconsistent,5,6 more attention should be paid to individual athlete performance in each task rather than the simple sum of scores. Coaches, conditioning trainers, athletic trainers, physiotherapists and other practitioners of the coaching/medical staff are increasingly interested in identifying specific deficits of athletes, aiming to plan and implement corrective programs to improve movement quality. In this way, scores in each one of the seven FMS™ tests (i.e., individual scores) and different scores between right and left side in the unilateral FMS™ tests (i.e., asymmetries) may provide more accurate information about the functional deficits of the evaluated athletes.17
The aim of the present study was to provide a detailed description on the performance of elite young soccer players (age 14-20 years) on FMS™ testing battery. FMS™ composite score, individual-test scores and asymmetries were addressed to provide relevant deficits observed in soccer athletes engaged in the highest competitive level of their age category.
METHODS
Study Design
Young soccer players from a Brazilian Series A professional club were invited to participate in this cross-sectional observational study. The study was approved by the institutional ethics committee (#1.196.139), and all volunteers (subjects ≥ 18 years old) or their legal representatives (subjects < 18 years old) provided informed consent before starting study participation. Each athlete performed the full battery of FMS™ in a single day. Tests were performed in their own training center and always before practice sessions. All evaluations were carried out between August and October (Brazilian season starts at February and ends at December).
Participants
One-hundred and three male soccer athletes, 14 to 20 years old, with experience in national and international competitions participated in this study. All athletes played in the youth categories of an elite Brazilian soccer club, recognized by the Brazilian Football Confederation as one of the main player development programs in Brazil. According to the organizational structure of the club, these athletes were divided into four competitive categories: U-15 (age ≤ 15 years, n=28), U-16 (age ≤ 16 years, n=26), U-17 (age ≤ 17 years, n=24) and U-20 (age ≤ 20 years, n=25). The U-15 and U-16 athletes trained once a day, six days a week, with each training session lasting approximately two hours (approximately 12 hours of on-field training per week). The U-17 and U-20 athletes trained in two additional shifts, completing about 16 hours of on-field training per week. All athletes performed gym training two to three times per week.
Participants with the following conditions were excluded from the study: (1) athletes with less than two years of competitive sport practice; (2) athletes currently undergoing rehabilitation of musculoskeletal injuries; or (3) athletes away from the team's training routine for >30 days within the six-month period prior to the study due to musculoskeletal injuries or any other health conditions.
Procedures
Anthropometric data from each participant was completed by the coaching staff that regularly performed these measurements as part of their evaluation routine. Body mass and height were respectively obtained from a calibrated scale (Urano, Brazil) and a stadiometer (Sanny, Brazil). Information regarding tactical position were also provided by the coaching staff. When the athlete played in more than one tactical position, the most frequently position was considered for analysis.
Participants were previously informed about the day and time they would be evaluated, and received the following recommendations: (1) not to perform high-intensity physical activities in the 24 hours prior to the tests; (2) not to drink alcohol within 48 hours prior to testing; (3) not to take any kind of analgesic and/or anti-inflammatory drugs within 48 hours prior to testing; (4) not to consume stimulant substances (e.g., caffeine) within 12 hours prior to testing; and (5) wear adequate clothing to perform the tests (shorts, t-shirt and sneakers).
Athletes were assessed using the full FMS™ protocol, comprised by seven movement patterns, following the order described by the creators of the method: (1) “Deep squat”; (2) “Hurdle step”; (3) “In-line lunge”; (4) “Shoulder mobility”; (5) “Active straight-leg raise”; (6) “Trunk stability push-up”; And (7) “Rotary stability”.1,2 The specific clearing tests were performed after tests #4, #6 and #7. Detailed explanation regarding each test and scoring procedures can be found in Cook et al.1,2 Evaluations were conducted by two experienced raters and carried out with an official FMS™ kit (Sanny, Brazil).
The raters explained each movement pattern in a standard way to the participants. Athletes performed three trials of each movement, and the best performance was considered for analysis. The ability to perform the movement pattern was observed by the two raters, who independently scored the task performance in a 4-point scale (0, 1, 2 or 3 points). The highest score from three trials was recorded in a specific worksheet. At the end of the test battery, both raters verified the agreement of the given scores for each pattern of movement performed. When there was disagreement in any scored test, player was asked to repeat the movement pattern.
Statistical Analyses
Descriptive statistics (mean, standard deviation, median, interquartile range, minimum and maximum values) were performed for the FMS™ composite scores. Participants who scored a 0 in the FMS™ (indicating pain) or a 1 (indicating dysfunction) in any test movement were classified into a “Fail” group; while athletes who scored only 2 or 3's were classified into a “Pass” group. Percentage distribution of individual scores (each one of the seven tests) and the presence of asymmetries in unilateral tests were also calculated. Categories (U-15, U-16, U-17 and U-20) were compared using one-way ANOVA followed by post-hoc Least Significant Difference (LSD) test for the following variables: body mass, height, FMS™ total score and the individual scores. All analyses were computed via SPSS® 17.0, and the level of significance for all tests was set at p<0.05.
RESULTS
As shown on Table 1, no significant differences in height between age categories were observed (p=0.902). However, the U-20 athletes had greater body mass compared to U-15 (p=0.001) and U-16 (p=0.001) athletes. The distribution in the tactical positions of players was similar among the categories.
Table 1.
Athletes’ characteristics.
| U-15 | U-16 | U-17 | U-20 | All | |
|---|---|---|---|---|---|
| (n=28) | (n=26) | (n=24) | (n=25) | (n=103) | |
| Height (m) | 1.78 ± 0.09 | 1.78 ± 0.07 | 1,79 ± 0,08 | 1.79 ± 0.08 | 1.78 ± 0.08 |
| Body mass (kg) | 68.79 ± 8.96 | 68.93 ± 8.47 | 72.69 ± 8.11 | 77.06 ± 9.77 | 71.74 ± 9.36 |
| Position [n(%)] | |||||
| Goalkeepers | 2 (7%) | 4 (15%) | 2 (8%) | 2 (8%) | 10 (10%) |
| Side backs | 4 (14%) | 3 (12%) | 3 (13%) | 4 (16%) | 14 (14%) |
| Central backs | 5 (18%) | 4 (15%) | 4 (17%) | 3 (12%) | 16 (16%) |
| Defender midfielders | 8 (29%) | 6 (23%) | 5 (21%) | 6 (24%) | 25 (24%) |
| Attacking midfielders | 4 (14%) | 7 (27%) | 3 (13%) | 4 (16%) | 18 (17%) |
| Forwards | 5 (18%) | 2 (8%) | 7 (29%) | 6 (24%) | 20 (19%) |
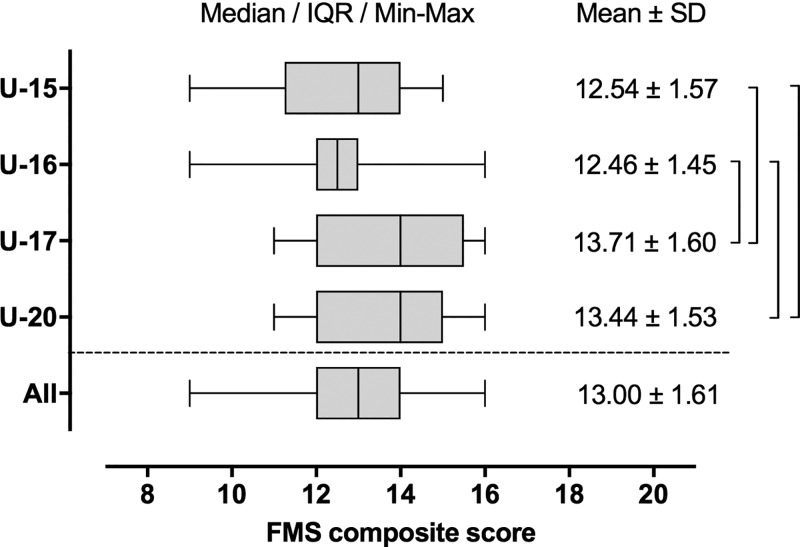
Eighty-two percent of the athletes had a FMS™ composite score ≤ 14 points (89% of U-15; 92% of U-16; 75% of U-17; and 72% of U-20). Ninety-one percent of players were classified into the “Fail” group (96% of U-15; 96% of U-16; 83% of U-17; and 88% of U-20). As observed in Figure 1, both U-15 and U-16 athletes presented lower values of composite score than the U-17 (p=0.007; p=0.005) and U-20 (p=0.035; p=0.025) players. Additional information regarding the FMS™ composite score are presented in Figure 1.
Figure 1.
FMS composite score: mean and standard deviation (right column); median and interquartile range (grey box); minimum and maximum values (whisker). Brackets indicate significant difference (p<0.05).
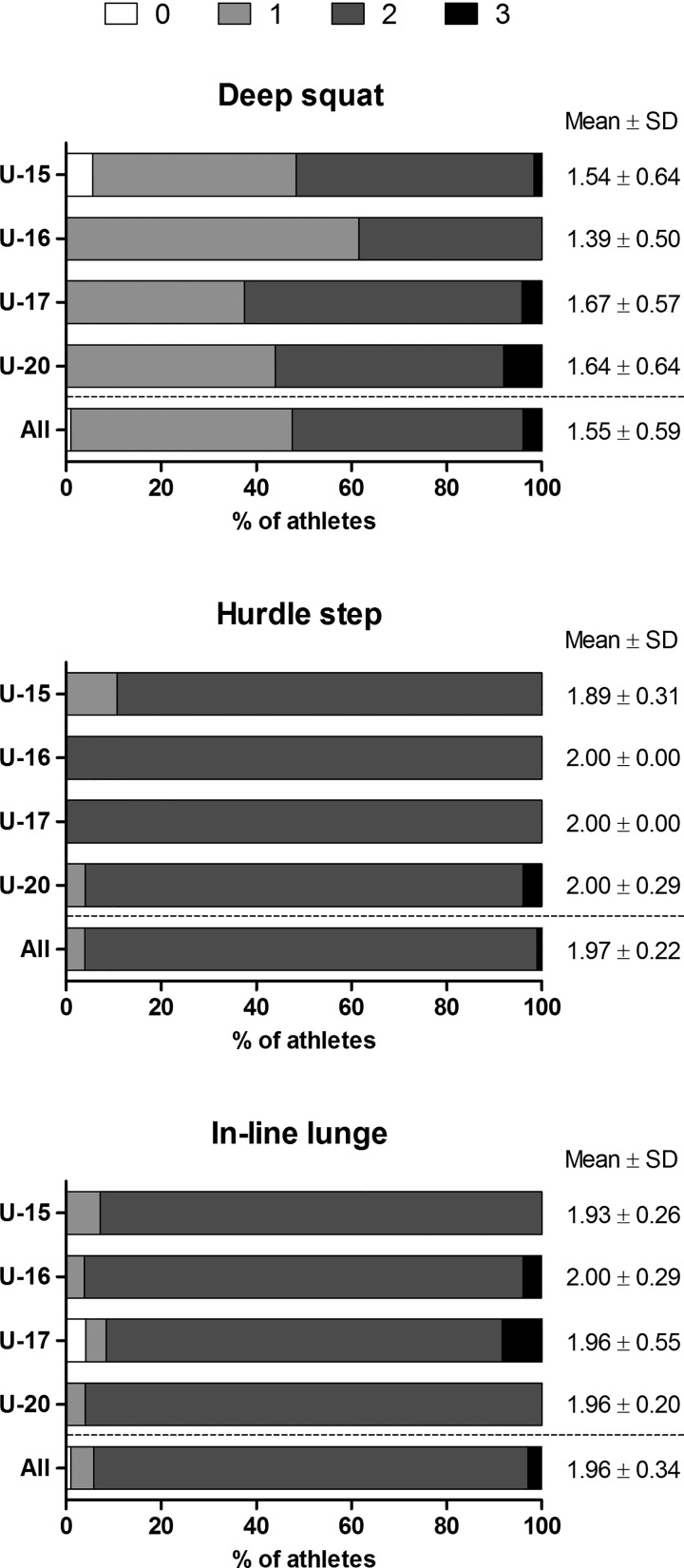
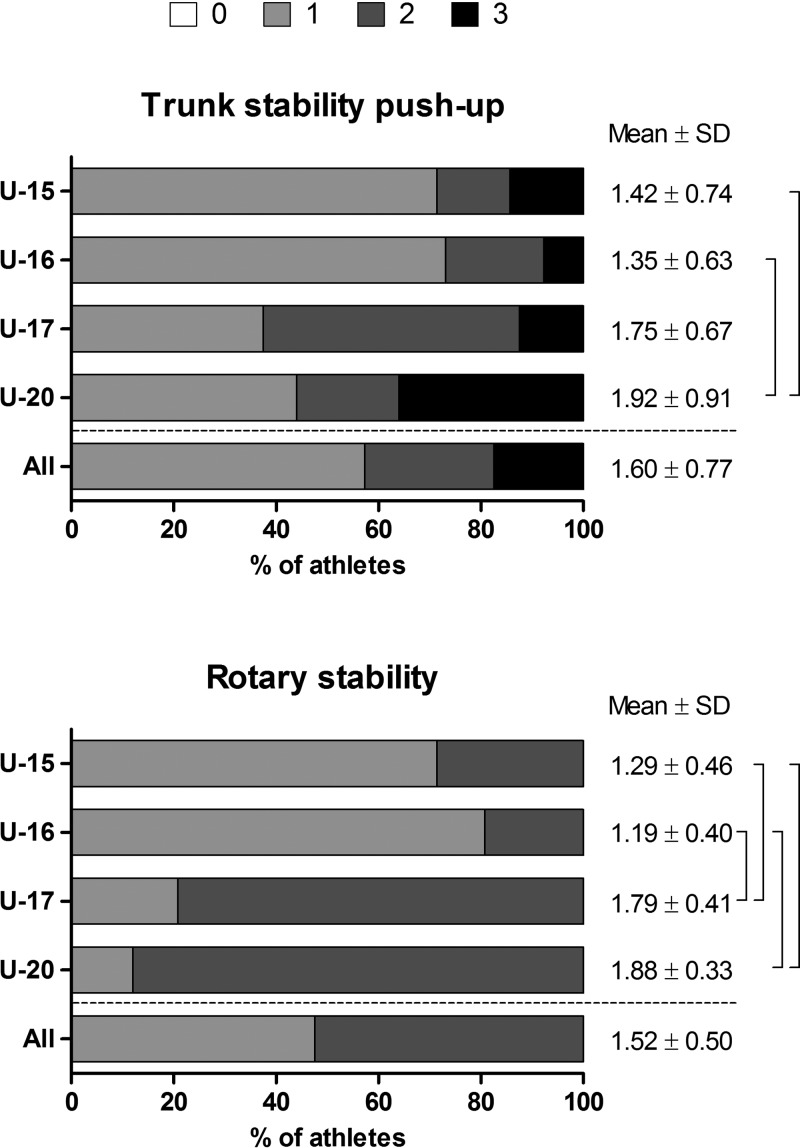
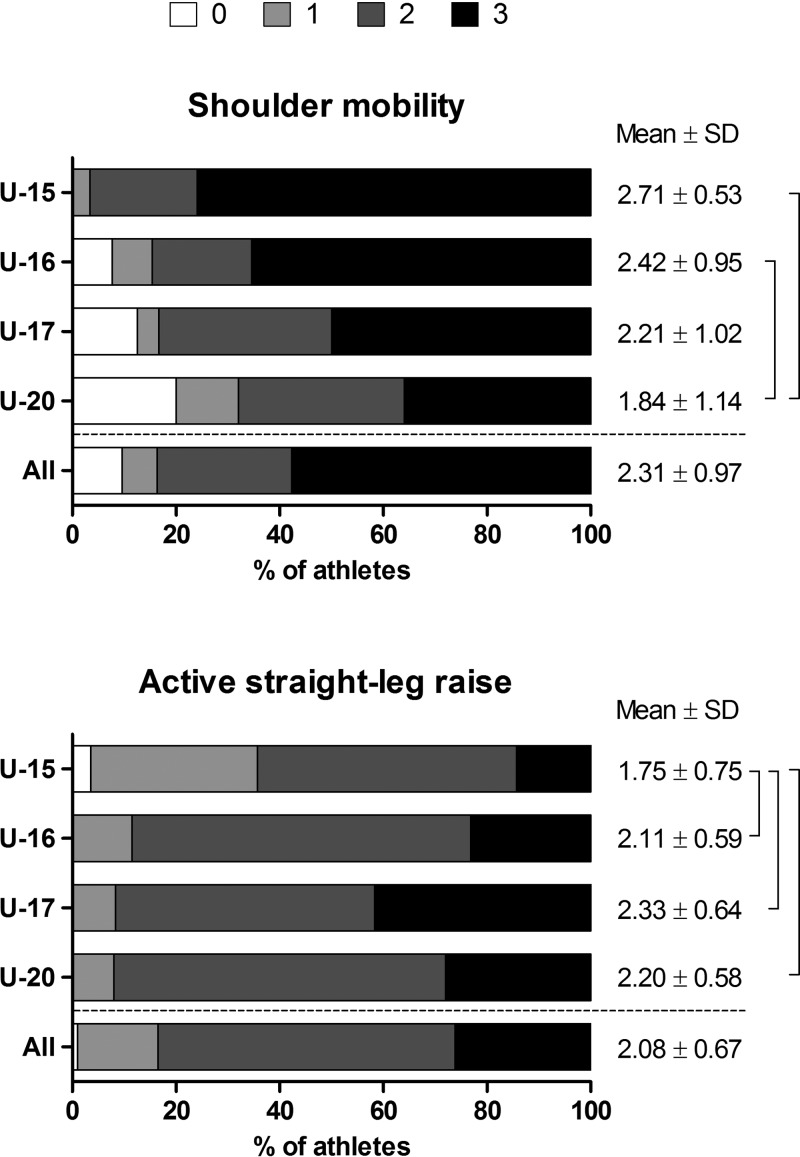
Distribution of the individual scores in each of the seven tests of FMS™ is presented in Figures 2 to 4. There were no significant differences between the categories considering the movement tests (Figure 2): “deep squat” (p=0.314), “hurdle step” (p=0.183), “in-line lunge” (p=0.900). On the mobility tests (Figure 3): U-15 and U-16 players had higher scores compared to U-20 category on “shoulder mobility” test (p=0.001; p=0.027); and the U-15 players had lower scores compared to any other categories in the active “straight-leg raise” test (p=0.040; p=0.002; p=0.013). Regarding the stability tests (Figure 4): U-20 athletes presented superior values compared to both U-15 (p=0.019) and U-16 (p=0.007) players on “trunk stability push-up” test; and the U-17 and U-20 athletes had higher individual scores compared to the U-15 and U-16 players in the “rotary stability” test (p<0.001 for all comparisons).
Figure 2.
FMS movement tests: percentage distribution (bars); mean and standard deviation (right column). No significant differences (p<0.05).
Figure 4.
FMS stability tests: percentage distribution (bars); mean and standard deviation (right column). Brackets indicate significant difference (p<0.05).
Figure 3.
FMS mobility tests: percentage distribution (bars); mean and standard deviation (right column). Brackets indicate significant difference (p<0.05).
The absolute number and percentage of athletes from each category presenting asymmetries can be observed in Table 2. A total of 65% of the participants presented asymmetry between right and left side in at least one of the five unilateral FMS™ tests.
Table 2.
Athletes’ characteristics.
| U-15 | U-16 | U-17 | U-20 | All | |
|---|---|---|---|---|---|
| (n=28) | (n=26) | (n=24) | (n=25) | (n=103) | |
| Hurdle step | 2 (7%) | 2 (8%) | 0 (0%) | 1 (4%) | 5 (5%) |
| In-line lunge | 2 (7%) | 1 (4%) | 2 (8%) | 1 (4%) | 6 (6%) |
| Shoulder mobility | 5 (18%) | 5 (19%) | 8 (33%) | 10 (40%) | 28 (27%) |
| Active straight-leg raise | 9 (32%) | 1 (4%) | 4 (17%) | 3 (12%) | 17 (17%) |
| Rotary Stability | 4 (14%) | 3 (12%) | 2 (8%) | 1 (4%) | 10 (10%) |
DISCUSSION
The objective of the present study was to describe the functional movement performance of high competitive level youth soccer players using the FMS™ test battery. The main findings of the current study were: (1) the athletes achieved composite scores ranging from 9 to 16 points; (2) most of athletes had a composite score ≤14 points; (3) almost half of athletes presented a poor performance (i.e., individual score < 2) on the “deep squat” test; (4) most of athletes in the younger categories (U-15 and U-16) had a poor performance on “trunk stability push-up” and on “rotary stability” tests; and (5) most of athletes presented asymmetry in at least one of the five unilateral tests.
Similarly to the present study, Portas et al.16 described an age-related effect on FMS™ composite scores in youth players of English Football League (from 11 to 14 points); while mean composite scores reported in adult players ranged between 1511 and 1612 points. A similar age-related performance seems to occur among female athletes, since collegiate18 and professional19 players obtained mean FMS™ composite scores of 13 and 16 points, respectively. Taken together, these findings suggest that younger athletes show greater deficits in functional movement patterns compared to older adolescent or adult players.
Of interest is the high percentage of athletes with total score ≤14 points in the present study. This cut-point was firstly proposed by Kiesel et al.4 in 2007, and a systematic review from Bonazza et al.5 also suggested a higher incidence of injuries in individuals with FMS™ composite scores ≤ 14 points. On the other hand, a recent systematic review by Moran et al.6 found a “moderate” evidence to recommend against the use of FMS™ total score as an injury prediction test in soccer, while the evidence was ‘”limited” or “conflicting” for other sport populations (including American football, college athletes, basketball, ice hockey and running). Therefore, the current literature does not consistently support the injury predictive value of the FMS™ composite score.
According the cohort study of Mocka et al.,17 college athletes with FMS™ composite scores ≤ 14 points were not at greater risk of musculoskeletal injury than those with higher scores, but athletes with an asymmetry or a score ≤1 on any individual test of the FMS™ were at 2.73 times greater risk of a musculoskeletal injury than others. Thus, the high incidence of players into the “Fail” group (91%) and with bilateral asymmetries (65%) found in the current study could present a real concern for the coaching/medical staff. The results reported here and in other studies with young male15,16 and female18 soccer athletes suggest that adaptations promoted by the specific training required by this sport does not lead players to adequate levels of functional movement. This hypothesis is strengthened by findings indicating that FMS™ composite scores are unaffected throughout the competitive soccer season at the university competitive level.14 In other words, a specific intervention program (in addition to the usual training performed in soccer) seems necessary to increase the FMS™ scores, as already demonstrated in American football players.20
The analysis of individual scores provides a deeper understanding on the movement deficits of athletes. Almost half of athletes did not reach satisfactory levels in the “deep squat” test, which can be explained by limitation of ankle dorsiflexion in most cases. Moreover, it seemed that the highest composite scores observed in the oldest athletes (U-17 and U-20) may be partially explained by the better performance of these players in the stability tests (trunk stability push-up and rotary stability). While 84% of the athletes of the two most advanced categories scored 2 points in rotary stability, only 26% of youngest athletes (U-15 and U-16) achieved this score. A similar pattern occurred in the “trunk stability push-up” test, although with a less expressive difference (59% vs. 30%). Considering that all four age categories investigated in the present study followed the same training routine in terms of technical preparation and injury prevention, it cannot be considered as an intervening factor on the observed results. Therefore, biological maturation seems to be the key factor providing better conditions for the accomplishment of movement patterns that require stability of the trunk, also considering that upper limb strength contributes to a good performance in the trunk stability push-up test.
Rotary stability was the only test in which none of the 103 athletes evaluated reached the maximum score. It has been already argued that the absence of well-conditioned stabilizing muscles contributes to the development of joint and/or muscle pain21. Evidences suggest that poor trunk stability is related with an increased risk of lower limb injuries22 and reduced sports performance.23 Therefore, trunk stabilization exercises were included in injury prevention programs, such as “FIFA 11 + ”, which was designed to reduce the most common injuries in soccer and has been widely used in the field.24 Strengthening of stabilizing muscles is considered one of the three most efficient strategies for injury prevention among practitioners working in elite soccer clubs,10 and the findings observed in the present study reinforce the importance of working out this muscle group in young soccer players.
Interestingly, age appears to have adversely affected the performance of athletes in upper extremity mobility (shoulder mobility test), but not in lower limbs (active straight-leg raise test). Generally, flexibility reaches its peak during childhood and tends to decrease gradually from adolescence.25 However, flexibility can be preserved and even increased with specific training programs;26 thus athletes involved in activities that demand movements with large range of motion have shown increased levels of flexibility compared to the general population.27 Although soccer does not require constant movements with exaggerated range of motion, it is important to note that posterior chain muscle flexibility deficits has traditionally been considered an intrinsic risk factor for hamstring muscle injury,28 considered the most prevalent injury in soccer.29 For this reason, flexibility of posterior thigh muscles has been emphasized in injury prevention programs in soccer.30 This concern does not apply to upper limbs due to its low injury rate, which may contribute to the more dramatic losses of range of motion in shoulders than legs observed in U-17 and U-20 categories. In addition, the resistance exercises for upper trunk (e.g., bench press, lat pull down) may also contribute to diminshed shoulder mobility in these athletes.
Kiesel et al.31 demonstrated that asymmetries in the unilateral tests of FMS™ could be an injury predictive factor. Although these asymmetries have already been shown in elite11 and semi-professional12 soccer players, the present study seems to be the first to report asymmetries in young soccer players and to discriminate which of the tests present these asymmetries. The high percentage of athletes presenting asymmetry in at least one of the five unilateral tests (65%) suggests that coaching/medical staff should pay attention to the imbalances generated by soccer practice, which is characterized by the predominance of motor gestures with a preferred lower limb (e.g., pass and kick). Surprisingly, the “shoulder mobility” test presented the highest number of asymmetries among the athletes, which can be considered the least representative movement demand on soccer practice (excepted for goalkeepers). The asymmetries on functional movement patterns induced by soccer training and its repercussions on sports performance and injuries should be further investigated.
One limitation of the present study is that the authors were not able to access the full history of athletes’ injuries, which is a possible confounding factor for FMS™ results. However, all athletes were deemed healthy during data collection and had no periods of absence ≥30 days in the previous six months, which gave confidence regarding the conditions in which each athlete performed the tests during the study.
CONCLUSION
In summary, most elite young soccer players (age 14-20 years) have important functional deficits, especially in tasks involving deep squat and trunk stability, as well as high prevalence of asymmetry between right and left sides of the body. The present study provides reference values on the FMS™ performance of high-level competitive soccer players in their respective age categories. Coaches, conditioning trainers, athletic trainers, physiotherapists, and other practitioners involved with soccer should be aware that young athletes seem to have greater functional deficits compared to adults,11,12,19 which may lead to a reduced technical capacity and increased injury risk. As a practical application, the authors recommend coaching/medical staff apply collective training programs with emphasis on trunk stabilization improvement (especially in younger players), while other specific deficits evidenced by FMS™ may be worked individually or in sub-groups.
REFERENCES
- 1.Cook G Burton L Hoogenboom BJ Voight M. Functional movement screening : the use of fundamental movements as an assssment of function - part 2. Int J Sports Phys Ther. 2014;9(3):549-563. [PMC free article] [PubMed] [Google Scholar]
- 2.Cook G Burton L Hoogenboom BJ Voight M. Functional movement screening: the use of fundamental movements as an assessment of function - part 1. Int J Sports Phys Ther. 2014;9(3):396-409. [PMC free article] [PubMed] [Google Scholar]
- 3.Moran RW Schneiders AG Major KM Sullivan SJ. How reliable are functional movement screening scoresϿ. A systematic review of rater reliability. Br J Sports Med. 2016;50(9):527-536. [DOI] [PubMed] [Google Scholar]
- 4.Kiesel K Plisky PJ Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther. 2007;2(3):147-158. [PMC free article] [PubMed] [Google Scholar]
- 5.Bonazza NA Smuin D Onks CA Silvis ML Dhawan A. Reliability, validity, and injury predictive value of the functional movement screen: a systematic review and meta-analysis. Am J Sports Med. 2017;45(3):725-732. [DOI] [PubMed] [Google Scholar]
- 6.Moran RW Schneiders AG Mason J Sullivan SJ. Do functional movement screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. Br J Sports Med. 2017;ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Agresta C Slobodinsky M Tucker C. Functional movement screen - normative values in healthy distance runners. Int J Sports Med. 2014;35(14):1203-1207. [DOI] [PubMed] [Google Scholar]
- 8.Bardenett SM Micca JJ DeNoyelles JT Miller SD Jenk DT Brooks GS. Functional movement screen normative values and validity in high school athletes: can the FMS™ be used as a predictor of injury? Int J Sports Phys Ther. 2015;10(3):303-308. [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y Wang X Chen X Dai B. Exploratory factor analysis of the functional movement screen in elite athletes. J Sports Sci. 2015;33(11):1166-1172. [DOI] [PubMed] [Google Scholar]
- 10.McCall A Carling C Nedelec M Davison M Le Gall F Berthoin S Dupont G. Risk factors, testing and preventative strategies for non-contact injuries in professional football: current perceptions and practices of 44 teams from various premier leagues. Br J Sports Med. 2014;48(18):1352-1357. [DOI] [PubMed] [Google Scholar]
- 11.Zalai D Panics G Bobak P Csáki I Hamar P. Quality of functional movement patterns and injury examination in elite-level male professional football players. Acta Physiol Hung. 2015;102(1):34-42. [DOI] [PubMed] [Google Scholar]
- 12.Smith P Hanlon M. Assessing the effectiveness of the functional movement screen (FMS™) in predicting non-contact injury rates in soccer players. J Strength Cond Res. 2016;ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Hammes D Aus der Fünten K Bizzini M Meyer T. Injury prediction in veteran football players using the functional movement screen™. J Sports Sci. 2016;34(14):1371-1379. [DOI] [PubMed] [Google Scholar]
- 14.Sprague PA Mokha GM Gatens DR. Changes in functional movement screen scores over a season in collegiate soccer and volleyball athletes. J Strength Cond Res. 2014;28(11):3155-3163. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd RS Oliver JL Radnor JM Rhodes BC Faigenbaum AD Myer GD. Relationships between functional movement screen scores, maturation and physical performance in young soccer players. J Sports Sci. 2015;33(1):11-19. [DOI] [PubMed] [Google Scholar]
- 16.Portas MD Parkin G Roberts J Batterham AM. Maturational effect on functional movement screen score in adolescent soccer players. J Sci Med Sport. 2016;19(10):854-858. [DOI] [PubMed] [Google Scholar]
- 17.Mokha M Sprague PA Gatens DR. Predicting musculoskeletal injury in National Collegiate Athletic Association division II athletes from asymmetries and individual-test versus composite functional movement screen scores. J Athl Train. 2016;51(4):276-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chorba RS Chorba DJ Bouillon LE Overmyer CA Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sport Phys Ther. 2010;5(2):47-54. [PMC free article] [PubMed] [Google Scholar]
- 19.Grygorowicz M Piontek T Dudzinski W. Evaluation of functional limitations in female soccer players and their relationship with sports level--a cross sectional study. PLoS One. 2013;8(6):e66871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kiesel K Plisky P Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sport. 2011;21(2):287-292. [DOI] [PubMed] [Google Scholar]
- 21.Hodges PW Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77(2):132-144. [DOI] [PubMed] [Google Scholar]
- 22.Leetun DT Ireland ML Willson JD Ballantyne BT Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926-934. [DOI] [PubMed] [Google Scholar]
- 23.Imai A Kaneoka K Okubo Y Shiraki H. Comparison of the immediate effect of different types of trunk exercise on the star excursion balance test in male adolescent soccer players. Int J Sports Phys Ther. 2014;9(4):428-435. [PMC free article] [PubMed] [Google Scholar]
- 24.Bizzini M Junge A Dvorak J. Implementation of the FIFA 11 + football warm up program: How to approach and convince the Football associations to invest in prevention. Br J Sport Med. 2013;47(12):803-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Medeiros HB De Araújo DSMS De Araújo CGS. Age-related mobility loss is joint-specific: an analysis from 6,000 flexitest results. Age (Omaha). 2013;35(6):2399-2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Decoster LC Cleland J Altieri C Russell P. The effects of hamstring stretching on range of motion: A systematic literature review. J Orthop Sports Phys Ther. 2005;35(6):377-387. [DOI] [PubMed] [Google Scholar]
- 27.Sands WA. et al. Stretching the spines of gymnasts: a review. Sports Medicine. 2016;46(3):315-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Witvrouw E Danneels L Asselman P D’Have T Cambier D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. Am J Sports Med. 2003;31(1):41-46. [DOI] [PubMed] [Google Scholar]
- 29.Ekstrand J Hägglund M Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553-558. [DOI] [PubMed] [Google Scholar]
- 30.Arnason A Andersen TE Holme I Engebretsen L Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sport. 2008;18(1):40-48. [DOI] [PubMed] [Google Scholar]
- 31.Kiesel KB Butler RJ Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. J Sport Rehabil. 2014;23(2):88-94. [DOI] [PubMed] [Google Scholar]