Abstract
Objective
An understanding of the levels and trends of medical cost is made for breast cancer patients with different medical insurance coverages in China (mainland), in an attempt to offer a clue to further control the costs.
Methods
The inpatient payments of 9,716,180 breast cancer patients spent in medical institutions of different types and grades during 2011–2015 were collected from the inpatient medical record home page (IMRHP) dataset. The data were then processed with SAS (Version 9.3; SAS Institute, Cary, NC, USA). Indicators like means, increase (decrease) percentages were used to descriptively analyze the average hospitalization expense of each time (AHEET) and its trends of breast cancer patients with different medical insurance coverages treated in medical institutions of different types and grades.
Results
In 2011–2015, the AHEET borne by breast cancer patients in China had been constantly increasing. Specifically, the self-pay inpatients had the largest increase, inpatients covered by Urban Employee Basic Medical Insurance (UEBMI) and Urban Resident Basic Medical Insurance (URBMI) were the next, and those covered by New Rural Cooperative Medical System (NRCMS) had the least increase. Breast cancer inpatient treated in public hospitals had quite greater increase and higher expenditure level than those in private hospitals. The AHEET borne by the inpatients in Grade 3 hospitals had greater increase and higher cost than those in Grade 2 hospitals.
Conclusions
The inpatient payments of breast cancer patients will be wisely controlled by reducing the number of self-pay inpatients, taking advantage of restriction mechanism of the medical insurances, and promoting healthy competition between private hospitals and public hospitals. The economic burden imposed on the society by breast cancer can be relieved through further control of inpatient payments of UEBMI- and URBMI-covered breast cancer patients and of Grade 3 hospitals.
Keywords: Breast cancer, inpatient payments, medical insurance
Introduction
Breast cancer is the most common malignant tumor in women, topping the incidence rate of malignant tumor in women across the world (1,2). According to the data released by National Central Cancer Registry (NCCR) of China, breast cancer has been the tumor with the highest incidence rate among women in China during the past years (3-5). With the development of society, changes of living styles and reproductive concepts, as well as extended life expectancy, the incidence rate of breast cancer shows a gradual upward trend. In 2015, the total inpatient payments for treating breast cancer in China ranked the fourth among all tumor diseases (6). Long treatment period and high costs bring large economic burden to both the society and families (7).
Basic medical insurance coverage in China is above 95% (8). Although the Specifications for Pricing Items of National Medical Services tends to define the same prices for medical services in China, overall treatment costs of breast cancer still vary due to the difference of medical insurance policies by region and of actions taken by medical institutions (9,10). At present, the researches on inpatient payments of breast cancer patients in China are often based on the accumulative data of patients costs collected by individual medical institutions or on the spot check data gathered by some medical institutions in certain regions. The researches have studied major factors that might have impact on the inpatient payments through regression analysis (11-15). Some have concluded that inpatient payments are under the influence of the type of medical insurances or payment (12,13). This paper attempts to have an understanding for levels and trends of inpatient payments of hospitals of different types (public and private) and grades (Grade 3 and Grade 2), by means of analyzing the overall situation of payments of breast cancer patients with different types of medical insurances during 2011–2015. We also indirectly analyze treatments taken by these medical institutions by comparing the payments of patients with different medical insurance coverages, both offer a clue to further control the costs and provide information for the insurance funds to draft specific payment policies in China (mainland).
Materials and methods
Data source
The data come from the inpatient medical record home page (IMRHP) dataset of Center for Health Statistics and Information (CHSI) of National Health and Family Planning Commission (NHFPC). The hospitals above Grade 2 are required to report their IMRHP data quarterly. The main information of IMRHPs includes: patient’s demographic information, code of diagnosis, types of health insurance, hospitalization expenses, code of surgery, etc. The validity and completeness of IMRHPs are controlled hierarchically. The data validity control mainly focuses on the logic check (i.e. male patients get female disease, infants get chronic disease). The completeness of IMRHPs is evaluated by two dimensions. One is about the completeness of item reporting for each IMRHP. The other dimension is about the completeness of the quantity of IMRHPs reporting. Provincial CHSIs check the quality of IMRHPs quarterly and give feedbacks to hospitals. The national CHSI examines the data quality yearly and gives feedback to provincial CHSIs. Besides, data quality control meetings, data quality supervision and inspections are carried out regularly. Information of the medical institutions is from the national hospital information database (HID) of NHFPC’s CHSI, covering nature, type and grade of all hospitals in China. In this study, the IMRHPs of 9,716,180 breast cancer inpatients in 2011–2015 have been collected.
Data analyses
The IMRHPs of breast cancer inpatients were retrieved from the database by ICD-10 codes. The data were processed with SAS (Version 9.3; SAS Institute, Cary, NC, USA). Indicators like means, increase (decrease) percentages were used to descriptively analyze the average hospitalization expense of each time (AHEET) of the breast cancer patients with different medical insurance coverages in medical institutions of different types and grades.
Since the IMRHP database from 2011 to 2015 only included the data from grade 2 and 3 hospitals (hospitals with more than 100 beds) and the duty of Grade 1 hospitals is mainly about the provision of clinic treatment on very common diseases (such as influenza and high blood pressure), disease prevention and patients referral services (6), this study only includes the payments in Grade 2 and Grade 3 hospitals.
Results
Overall situation and trends of breast cancer patients’ medical expense
All breast cancer patients’ AHEET and its ratio in resident income
From 2011 to 2015, both the absolute values of AHEET and the adjusted values of comparable prices of the breast cancer patients have generally showed an upward trend year on year in China (Table 1). The absolute ones have increased by 14,362 RMB, a rise of 14.87% from 2011 to 2015. The adjusted ones have increased by 668 RMB, a rise of 5.50% in the same period. The ring growth rate of the comparable prices has slowed down from 2014 to 2015. According to the China Health Statistics Yearbook (16,17), urban residents’ average disposable income per capita was 21,809.8 RMB and 31,194.8 RMB respectively in the year 2011 and 2015, and rural residents’ average disposable income per capita reached 6,977.3 RMB and 11,421.7 RMB separately in 2011 and 2015. In 2011 the AHEET of breast cancer patients was 57.33% of urban residents’ disposable income per capita, and 1.79 times of rural residents’ net income. While in 2015 the figures reached 46.04% and 1.26 individually.
1.
AHEET of breast cancer patients in China (mainland) in 2011–2015 (RMB)
| AHEET | 2011 | 2012 | 2013 | 2014 | 2015 |
| AHEET, average hospitalization expense of each time; CPI, consumer price index. | |||||
| Expense | 12,503 | 13,022 | 13,741 | 14,056 | 14,362 |
| Adjusted expense | 12,503 | 12,692 | 13,054 | 13,091 | 13,191 |
| Ring growth of adjusted expense based on CPI | – | 1.51% | 2.85% | 0.29% | 0.76% |
AHEET and its trends of breast cancer patients with different medical insurance coverages [Urban Employee Basic Medical Insurance (UEBMI), Urban Resident Basic Medical Insurance (URBMI), New Rural Cooperative Medical System (NRCMS) and self-pay]
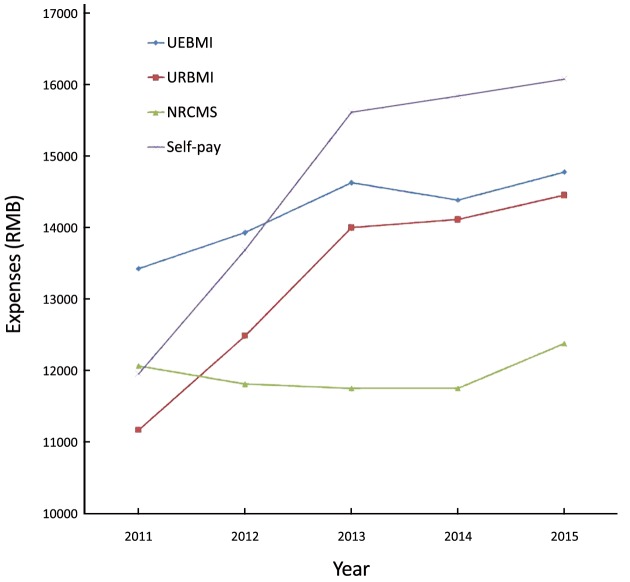
The AHEET of the four types of breast cancer patients generally took on an upward trend. In 2011, the lowest payment was observed in URBMI (at 11,167 RMB) and the highest one in UEBMI (at 13,430 RMB). In 2015, the lowest payment was seen in NRCMS (at 12,382 RMB) and the highest in self-pay (at 16,084 RMB). From 2013 to 2015, the self-pay patients saw a higher AHEET than those covered by medical insurances (UEBMI, URBMI and NRCMS), which is identical to the results of researches conducted by other researchers (9,18) and indicates that medical insurance has certain control over the growth of medical costs. It should also be noted that the payments of NRCMS-covered breast cancer patients had been decreasing from 2011 to 2014, which may have something to do with the fact that the expenses that can be virtually reimbursed by NRCMS-covered inpatients are quite low (19) (Figure 1).
1.
Average hospitalization expense of each time (AHEET) trends of breast cancer patients with different medical insurance coverages.
AHEET and its trends of breast cancer patients in different types of hospitals
From 2011 to 2015 the AHEETs of the breast cancer patients spent in public hospitals were 12,510 RMB, 13,037 RMB, 13,763 RMB, 14,081 RMB and 14,424 RMB respectively, and those in private hospitals were 11,672 RMB, 11,763 RMB, 12,054 RMB, 11,659 RMB and 11,172 RMB respectively. The AHEET in public hospitals was found to be always higher than that in private hospitals, with a greater increase of 15.30%. Private hospitals showed a downward trend, dropping by 4.30% during the five years.
According to Blue Book of Private Hospitals: Annual Report on China’s Private Hospitals Development (2016) (20), the average length of stay in hospital and average inpatient payments for treating major diseases, representative diseases and difficult and complicated cases in private hospitals were lower than those in public hospitals. In addition, according to statistics in China (21,22), the average hospitalization expense of public hospitals was 6,909.90 RMB in 2011 and 8,290.50 RMB in 2015, a growth of 19.98% in the five years. According to another research (23), the outpatient & emergency costs and inpatient payments of private hospitals were lower than those of public hospitals. The AHEET of private hospitals increased from 3,797.96 RMB in 2010 to 5,033.82 RMB in 2014, a growth of 32.54%. In comparison, no matter in public or private hospitals, the AHEET growth rate of breast cancer patients is lower than that of all patients in China.
AHEET and its trends of breast cancer patients in different grades of hospitals
From 2011 to 2015 the AHEET of the breast cancer patients spent in Grade 3 general hospitals was 13,960 RMB, 14,316 RMB, 14,871 RMB, 14,966 RMB and 15,508 RMB respectively, and 8,676 RMB, 8,518 RMB, 8,560 RMB, 9,532 RMB and 8,409 RMB respectively in Grade 2 general hospitals. The AHEET of the inpatients spent in Grade 3 hospitals was always higher than that in Grade 2 hospitals, with a larger growth of 11.90%. Grade 2 hospitals generally presented a downward trend, decreasing by 3.08% in the five years.
According to the Statistical Communique of China on the Health and Family Planning Development (21,22), the average hospitalization expenses were 10,935.9 RMB in Grade 3 hospitals and 4,564.2 RMB in Grade 2 hospitals in 2011, and in 2015, the payments were 12,599.3 RMB in Grade 3 hospitals and 5,358.2 RMB in Grade 2 hospitals. From 2011 to 2015, the AHEET increased by 15.21% in Grade 3 hospitals and 17.40% in Grade 2 hospitals in China. In comparison, the growth rates of inpatient payments of the breast cancer patients at both Grade 3 and Grade 2 hospitals were lower than that of all patients in China, and the inpatient payment at Grade 2 hospitals even witnessed a downward trend.
Categorization and trends of the payments of breast cancer patients with different medical insurance coverages
AHEET and its trends in the same type of hospitals
The AHEETs of the breast cancer patients with the four types of medical insurance coverages spent in public and private hospitals are shown in Table 2. The AHEET trend of the patients with different medical insurance coverages treated in public hospitals are identical to that in Figure 1. The AHEET and its trend in private hospitals are quite different from those in Figure 1. As for public hospitals, the payment of self-pay patients was the highest in 2015, and the growth rate was the highest (at 34.82%) compared with the figure in 2011; the payment of NRCMS-covered patients was the lowest, and the growth rate was the lowest (at 2.95%) compared with the figure in 2011. As for private hospitals, the payment of self-pay patients was the highest in 2015, and the growth rate was quite high (at 14.24%) compared with the figure in 2011; the payment of NRCMS-covered patients was the lowest, and the growth rate was also the lowest (at –6.87%) compared with the figure in 2011. From 2011 to 2013, the payment of NRCMS-covered patients spent in public hospitals took on a downward trend, while that in private hospitals showed an upward trend over the same period.
2.
AHEET of breast cancer patients spent in different types of hospitals in 2011–2015 (RMB)
| Hospital type | Type of medical insurance coverage | 2011 | 2012 | 2013 | 2014 | 2015 |
| AHEET, average hospitalization expense of each time; UEBMI, Urban Employee Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; NRCMS, New Rural Cooperative Medical System. | ||||||
| Public | UEBMI | 13,438 | 13,953 | 14,669 | 14,407 | 14,864 |
| URBMI | 11,191 | 12,498 | 14,006 | 14,135 | 14,515 | |
| NRCMS | 12,097 | 11,833 | 11,769 | 11,774 | 12,454 | |
| Self-pay | 11,940 | 13,702 | 15,665 | 15,891 | 16,097 | |
| Private | UEBMI | 12,376 | 12,368 | 12,560 | 12,853 | 10,973 |
| URBMI | 9,083 | 11,292 | 13,702 | 11,952 | 11,897 | |
| NRCMS | 8,912 | 9,465 | 10,217 | 10,117 | 8,300 | |
| Self-pay | 13,557 | 13,111 | 12,865 | 11,996 | 15,488 | |
AHEET and its trends of patients with the same type of medical insurance coverage in different types of medical institutions
The AHEETs of the breast cancer patients with different medical insurance coverages in different types of hospitals are shown in Table 2. It should be noted that except for that the AHEET of the self-pay patients spent in public hospitals was lower than that in private hospitals, the AHEET of the breast cancer patients covered by medical insurances and treated in public hospitals was higher than that in private hospitals. Besides, in the five years, the AHEET growth rate of UEBMI-covered patients in public hospitals increased by 10.61%, while in private hospitals, it dropped by 11.34%. For NRCMS-covered patients, the growth rate of inpatient payment in public hospitals was quite small (at 2.95%) while it dropped by 6.87% in private hospitals. For URBMI-covered patients, the growth rates of inpatient payments in both public and private hospitals were quite high, at 29.70% and 30.98%, respectively. For self-pay patients, the inpatient payment in public hospitals increased gradually year by year, while in private hospitals, it dropped before 2014 and increased afterwards.
AHEET and its trends in the same grade of hospitals
The AHEETs of the breast cancer patients with different medical insurance coverages spent in Grade 2 and Grade 3 hospitals are shown in Table 3. Among them, the trend of the payments of the patients with the four types of medical insurance coverages in Grade 3 hospitals is identical with that in Figure 1, and the trend in Grade 2 hospitals is quite different from that in Figure 1. The AHEETs of the inpatients with the four types of medical insurance coverages spent in Grade 3 hospitals were increasing. Among them, URBMI-covered patients had the largest increase (26.48%), while NRCMS-covered patients had the smallest increase (5.84%). Of the AHEET of the inpatients with the four types of medical insurance coverages at Grade 2 hospitals, some increased and others dropped. Among them, the self-pay patients had the largest growth rate (28.25%), while the NRCMS-covered patients had the smallest growth rate (–9.41%). In addition, since 2013, the payments of self-pay patients spent in Grade 2 and Grade 3 hospitals had been the highest.
3.
AHEET of breast cancer patients spent in different grades of hospitals in 2011–2015 (RMB)
| Hospital grade | Type of medical insurance coverage | 2011 | 2012 | 2013 | 2014 | 2015 |
| AHEET, average hospitalization expense of each time; UEBMI, Urban Employee Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; NRCMS, New Rural Cooperative Medical System. | ||||||
| Grade 2 general | UEBMI | 9,955 | 9,471 | 9,186 | 11,628 | 9,760 |
| URBMI | 7,544 | 8,210 | 9,076 | 10,048 | 9,640 | |
| NRCMS | 7,929 | 7,863 | 7,997 | 7,410 | 7,183 | |
| Self-pay | 8,252 | 8,649 | 9,246 | 12,187 | 10,583 | |
| Grade 3 general | UEBMI | 14,741 | 15,078 | 15,615 | 15,573 | 16,278 |
| URBMI | 12,454 | 13,556 | 14,858 | 15,516 | 15,752 | |
| NRCMS | 13,670 | 13,472 | 13,474 | 13,516 | 14,469 | |
| Self-pay | 13,449 | 14,671 | 16,094 | 16,517 | 16,428 | |
AHEET and its trends of the patients with the same type of medical insurance coverage in different grades of hospitals
The AHEETs of the breast cancer patients with the four types of medical insurance coverages spent in different grades of hospitals are shown in Table 3. Among them, the AHEET of the patients with all four types of medical insurance coverages spent in Grade 3 hospitals was higher than that in Grade 2 hospitals. The AHEET of UEBMI-covered and NRCMS-covered patients spent in Grade 2 hospitals overall took on a downward trend, and that of URBMI-covered and self-pay patients spent in Grade 2 hospitals saw an upward trend.
Discussion
This study shows that, in terms of either overall inpatient payments level or the inpatient payments in different medical institutions, the self-pay breast cancer patients have paid higher AHEET than those covered by medical insurances in recent years in China, particularly since 2013 (Figure 1, Table 2, Table 3). There are mainly two types of self-pay patients: type 1 is those who have no medical insurance at all; and type 2 is those who suffer loss of the medical insurance coverage by seeking treatment at a superior hospital before proper referral procedures have been taken. Type 2 patients usually feature either strong financial capacity or severe or complicated illness. As self-pay patients are not restricted by pertinent cost reimbursement policies and type 2 patients have their own characteristics, medical institutions tend to provide overtreatment, which results in high AHEET consequently. Our suggestions are: firstly, further expanding the coverage of medical insurances; secondly, offering smooth referral channels for inpatients with breast cancer. We should both guarantee that those requiring medical attentions can be treated as long as they are under the coverage of medical insurances, and regulate activities of medical institutions with the help of monitoring and restriction mechanism of medical insurance policies to control the costs for treatment of breast cancer. Besides, the AHEETs and the growth rates of UEBMI- and URBMI-covered patients are generally higher than those of NRCMS-covered patients (Figure 1, Table 2, Table 3). It is suggested that the advantages and reasons of NRCMS control mechanism should be further studied, and more control should be exercised over the inpatient payments of the UEBMI- and URBMI-covered breast cancer patients.
In the five years, the AHEET and its growth rate of breast cancer patients spent in public hospitals have been higher than those treated in private hospitals nationwide, while those in private hospitals present a downward trend. Moreover, the AHEET of the patients with the four types of medical insurance coverages spent in public hospitals is all higher than that in private hospitals. The reasons are, firstly, the patients treated in public hospitals have more complicated conditions than those treated in private hospitals; secondly, public hospitals have advanced treatment approaches and equipment; and thirdly, monopolistic positions that public hospitals are in give them poor awareness to control the costs. Therefore, it is suggested that supports should be granted to private hospitals regarding medical insurance policy and technical improvement. It is therefore hoped to break public hospitals’ monopoly, promote virtuous competition between private and public hospitals, and improve public hospitals’ awareness to control the costs through market competition.
The AHEET of breast cancer patients spent at Grade 3 hospitals is higher than that in Grade 2 hospitals, and the AHEET of the breast cancer patients with the four types of medical insurance coverages spent at Grade 3 hospitals is all higher than that in Grade 2 hospitals over the same period (Table 3). The reasons for the fact may be: 1) The treatment level is much higher in Grade 3 medical institutions, where there are high percentages of patients with severe conditions and complications; 2) Grade 3 hospitals are mostly located in urban areas where the patients have better medical insurance coverage and stronger financial capacity. Therefore, the costs are controlled poorer there than in Grade 2 hospitals. Our suggestions are: firstly, comprehensively utilizing clinical approaches, DRGs payment and other approaches (24) to regulate treatment activities of Grade 3 hospitals. Secondly, guide patients with breast cancer to reasonably use medical resources, by applying the hierarchical diagnosis and treatment mode.
It should be noted that there are some limitations of this study. Firstly, as exclusive patient ID data are incomplete, only the AHEET is discussed in the paper. When quality of the IMRHP dataset improves and the database is upgraded, the practice of exclusive patient ID is hopefully to be exercised in the future for outpatient or hospitalized treatment, and the total costs of a breast cancer patient can be tracked down and analyzed. Secondly, as the classification for illness degree of the breast cancer patients is not available, analysis and comparison of the costs of breast cancer patients by illness degree cannot be conducted accordingly. In the following research, stratified analysis on difficulty level should be made so as to offer more targeted strategies to control the costs.
Conclusions
The inpatient payments of breast cancer patients will be wisely controlled by expanding the medical insurance coverage, keeping the referral channels smooth, reducing the number of self-pay inpatients, and taking advantage of restriction mechanism of the medical insurances. The costs in public hospitals can be reduced after incorporating those private hospitals whose diagnosis & treatment and management levels are up to pertinent requirements into the list of designated medical insurance hospitals to engage in virtuous competition with public ones. The economic burden imposed on the society by breast cancer can be relieved through further control of inpatient payments of UEBMI- and URBMI-covered breast cancer patients and of Grade 3 hospitals.
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 71403189).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Zuo T, Chen W. Advances in research on population-based female breast cancer survival in China. Zhongguo Zhong Liu Lin Chuang (in Chinese) 2016;43:639–42. doi: 10.3969/j.issn.1000-8179.2016.14.503. [DOI] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.Chen W, Zheng R, Zeng H, et al. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27:2–12. doi: 10.3978/j.issn.1000-9604.2015.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen W, Zheng R, Zou T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res. 2016;28:1–11. doi: 10.3978/j.issn.1000-9604.2016.02.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res. 2017;29:1–10. doi: 10.21147/j.issn.1000-9604.2017.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai Y, Xue M, Chen W, et al. Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. 2017;29:253–62. doi: 10.21147/j.issn.1000-9604.2017.03.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaidi AA, Ansari TZ, Khan A. The financial burden of cancer: estimates from patients undergoing cancer care in a tertiary care hospital. Int J Equity Health. 2012;11:60. doi: 10.1186/1475-9276-11-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The State Council Information Office of the People’s Republic of China. Right to Development: China’s Idea, Practice and Contribution. Available online: http://www.scio.gov.cn/ztk/dtzt/34102/35549/35553/Document/1532310/1532310.htm
- 9.Chen Z, Leng J, Gao G, et al. Analysis on hospitalization expense of five kinds of cancers and its influencing factors. Zhongguo Wei Sheng Jing Ji (in Chinese) 2014;33:57–60. doi: 10.7664/CHE20140717. [DOI] [Google Scholar]
- 10.Zhu R, Feng X, Yang H, et al. Analysis on hospitalization costs in 886 breast-cancer cases. Zhonghua Ji Bing Kong Zhi Za Zhi (in Chinese) 2014;18:247–51. [Google Scholar]
- 11.Zhao X, Zhang X, Tang Y, et al. Analysis on the hospitalization expense of breast cancer operation patients and its influencing factors. Zhongguo Wei Sheng Jing Ji (in Chinese) 2009;28:41–3. doi: 10.3969/j.issn.1003-0743.2009.01.013. [DOI] [Google Scholar]
- 12.Xiao J, Yang M, Wei S, et al. Pathway analysis of the hospitalization expense influencing factors of the 2020 breast cancer in Nantong city. Zhongguo Fu You Bao Jian (in Chinese) 2012;27:1617–20. [Google Scholar]
- 13.Wang L, Bi X, Li Q. An analysis of hospitalized expenses and the influencing factors in patient with breast cancer. Zhongguo Zhong Liu (in Chinese) 2012;21:337–9. [Google Scholar]
- 14.MA JB. A Comparative study on hospitalization expenditure and its reimbursement level among breast cancer patients with different kinds of basic health insurance. Jinan: Shandong University, 2015.
- 15.Wang H, Bai Y, Hu X, et al. Trend analysis on direct economic burden of 3042 patients with breast cancer in Lanzhou city. Zhongguo Fu You Bao Jian (in Chinese) 2012;27:5677–80. [Google Scholar]
- 16.Health Ministry of the People’s Republic of China. China’s Health and Family Planning Statistical Yearbook. Beijing: China Union Medical University Press, 2013.
- 17.National Health and Family Planning Commission of the People’s Republic of China. China’s Health and Family Planning Statistics Yearbook 2016. Beijing: China Union Medical University Press, 2016.
- 18.Zhou C, Zhang L, Xiong H, et al. A retrospective survey and analysis of hospitalization expenses and related factors of lung cancer in cancer hospitals. Zhongguo Yi Yuan Guan Li (in Chinese) 2010;30:37–8. doi: 10.3969/j.issn.1001-5329.2010.07.015. [DOI] [Google Scholar]
- 19.Center for Health Statistics and Information, NHFPC. An Analysis Report of National Health Service Survey in China, 2013. Available online: http://www.nhfpc.gov.cn/mohwsbwstjxxzx/s8211/201610/9f109ff40e9346fca76dd82cecf419ce.shtml
- 20.Xue XL, Zhao C, Ye QF. Blue Book of Private Hospitals: Annual Report on China’s Private Hospitals Development (2016). Beijing: Social Sciences Academic Press, 2016. Available online: http://www.ssap.com.cn/c/2017-03-31/1052792.shtml
- 21.Statistical bulletin of China health development in 2011. Available online: http://www.nhfpc.gov.cn/mohwsbwstjxxzx/s7967/201204/54532.shtml
- 22.Statistical bulletin on the development of health and family planning in China in 2015. Available online: http://www.nhfpc.gov.cn/guihuaxxs/s10748/201607/da7575d64fa04670b5f375c87b6229b0.shtml
- 23.Jiang W, Li Q, Zhu Z. Research on the development status of private hospitals in China. Zhongguo Wei Sheng Jing Ji (in Chinese) 2016;35:29–31. doi: 10.7664/CHE20160507. [DOI] [Google Scholar]
- 24.DeMario MD, Ratain MJ. Oral chemotherapy: rationale and future directions. J Clin Oncol. 1998;16:2557–67. doi: 10.1200/JCO.1998.16.7.2557. [DOI] [PubMed] [Google Scholar]