Version Changes
Revised. Amendments from Version 1
The grant information for this version 2 has been re-worded, although the grants funding this work have not changed.
Abstract
Background: Developing alternative exercise programmes that can alleviate certain barriers to exercise such as psychological, environmental or socio-economical barriers, but provide similar physiological benefits e.g. increases in muscle mass and strength, is of grave importance. This pilot study aimed to assess the efficacy of an unsupervised, 4-week, whole-body home-based exercise training (HBET) programme, incorporated into daily living activities, on skeletal muscle mass, power and strength.
Methods: Twelve healthy older volunteers (63±3 years, 7 men: 5 women, BMI: 29±1 kg/m²) carried out the 4-week “lifestyle-integrated” HBET of 8 exercises, 3x12 repetitions each, every day. Before and after HBET, a number of physical function tests were carried out: unilateral leg extension 1-RM (one- repetition maximum), MVC (maximal voluntary contraction) leg extension, lower leg muscle power (via Nottingham Power Rig), handgrip strength and SPPBT (short physical performance battery test). A D 3-Creatine method was used for assessment of whole-body skeletal muscle mass, and ultrasound was used to measure the quadriceps cross-sectional area (CSA) and vastus lateralis muscle thickness.
Results: Four weeks HBET elicited significant (p<0.05) improvements in leg muscle power (276.7±38.5 vs. 323.4±43.4 W), maximal voluntary contraction (60°: 154.2±18.4 vs. 168.8±15.2 Nm, 90°: 152.1±10.5 vs. 159.1±11.4 Nm) and quadriceps CSA (57.5±5.4 vs. 59.0±5.3 cm 2), with a trend for an increase in leg strength (1-RM: 45.7±5.9 vs. 49.6±6.0 kg, P=0.08). This was despite there being no significant differences in whole-body skeletal muscle mass, as assessed via D 3-Creatine.
Conclusions: This study demonstrates that increases in multiple aspects of muscle function can be achieved in older adults with just 4-weeks of “lifestyle-integrated” HBET, with a cost-effective means. This training mode may prove to be a beneficial alternative for maintaining and/or improving muscle mass and function in older adults.
Keywords: home-based, exercise, muscle mass, muscle function
Introduction
Older age is associated with the loss of skeletal muscle mass. Termed sarcopenia, age-related muscle wasting is associated with loss of muscle strength ( dynapenia), increased morbidity, loss of independence and premature mortality ( Rudrappa et al., 2016). There are however proven means by which to offset these detrimental progressive declines. For example, structured and fully-supervised progressive resistance exercise training (RET) has been shown to improve both muscle mass ( Phillips et al., 2012) and function ( Liu & Latham, 2009).
Despite the established effects of RET on muscle mass and function, compliance is difficult to achieve, due to perceived (and real) socio-economic, psychological and environmental factors ( Zlot et al., 2006). Almost all current evidence for the efficacy of RET is based on 2–3 sessions each week, for up to 12 weeks, at a gym or with specialist equipment, reflecting current physical activity guidelines for adults of 2–3 days per week RET for each of the major muscle groups ( Bull et al., 2010). However, compliance to physical activity recommendations is poor, with recent data suggesting that they are only achieved by 38% of UK adults ( Department of Health, Physical Activity, 2011), a figure that is lesser still in older adults ( Jefferis et al., 2014). As a result, home-based exercise training (HBET) programmes have been suggested as an alternative to overcome some of the barriers associated with poor compliance to exercise ( Hong et al., 2017; Silveira et al., 2013), whilst also providing a platform to develop the benefits of RET for (pre-) sarcopenic individuals ( Maruya et al., 2016).
The majority of HBET studies to date, have focussed on pre- or rehabilitation for specific clinical groups ( Bassett & Prapavessis, 2007; Chang et al., 2017). A small number of studies have specifically investigated the efficacy of HBET on skeletal muscle function in the elderly, although the focus of these studies has mainly been on lower limb exercises to improve walking and balance ( Ito et al., 2015; Yamauchi et al., 2009) in relation to fall and fracture prevention. Other studies in older adults have incorporated the use of specialist aids e.g. dumbbells ( Plotnikoff et al., 2010), elastic bands ( Jette et al., 1999; Ribeiro et al., 2009) or ankle weights ( Gardner et al., 2001) to provide resistance for HBET; rather than attempting to incorporate exercise into tasks of daily living, as is done herein. To date, no studies have attempted to investigate the efficacy of incorporating whole-body exercise into activities of daily living on muscle mass and function in older adults. Consequently, in this pilot study we aimed to assess the effects of a 4-week, progressive, whole-body HBET fully integrated into activities of daily living, on muscle mass and function in healthy older individuals. We also aimed to utilise a recently re-introduced ( Clark et al., 2014) and underexploited creatine method to estimate whole-body muscle mass in humans.
Materials and methods
Ethical statement and recruitment of study participants
Twelve healthy older male and female volunteers (63±3 y, 7 men: 5 women, BMI: 29±1 kg/m 2) with no previous chronic disease history were recruited via an advertisement on a local radio station. Before enrolment into the study, all volunteers had an assessment of previous medical history and an ECG to check for any subclinical arrhythmias. The ECG’s were approved by a clinically qualified physician. All volunteers provided written informed consent prior to the start of this study. This study was approved by The University of Nottingham Medical School Ethics Committee (B28102015 SoMS GEM BBC) and conformed to The Declaration of Helsinki.
Study procedures
The study involved two visits by the study participants, before and after the 4-week HBET ( Figure 1), to the University of Nottingham Medical School, at the Royal Derby Hospital. All assessments at these visits were conducted by researchers from the MRC-ARUK Centre for Musculoskeletal Ageing Research. At each visit, volunteers provided a baseline urine sample for the muscle mass assessment by D 3-Creatine before undergoing measures of height, weight (Marsden Weighing Group, UK), resting heart rate and blood pressure (Omron M5-1 digital BP monitor, Omron, UK). Each volunteer had the thickness, fascicle length ( L f) and pennation angle ( θ pen) of their vastus lateralis muscle , and the cross-sectional area (CSA) of their quadriceps measured by ultrasound (Mylab 70, Esaote Biomedica, Genova, Italy), using the protocol described by Franchi et al. (2014). Volunteers then completed a number of muscle function assessments:
-
•
maximal voluntary contraction (MVC) for seated leg extension and flexion using an isokinetic dynamometer (Isocom; Isokinetic Technologies, Eurokinetics, UK),
-
•
leg extension 1-repetition maximum (1-RM; ISO leg extension, Leisure Lines Ltd., GB),
-
•
leg power (Nottingham Power Rig; Bassey & Short, 1990),
-
•
handgrip strength (Grip D 5401; Takei Scientific Instruments Co. Ltd., Japan); and
-
•
a short physical performance battery test (SPPBT; Guralnik et al., 1994).
Figure 1. Study schematic displaying the two visits before and after home-based exercise training (HBET).
BL: baseline urine sample; HR: resting heart rate; BP: resting blood pressure; SPPBT: short physical performance battery test; US: leg ultrasound; MVC: maximum voluntary contraction; 1-RM: leg extension 1-repetition maximum; D 3-Cr: D 3-Creatine for whole-body muscle mass assessment; 48 and 72h represent the time of urine samples post-tracer consumption.
MVC was measured at two knee angles (60 and 90°), whilst isokinetic (eccentric/concentric) contractions were measured over a 70° range (20–90°) at three different speeds (60, 180 and 240°/sec). For both measures, horizontal seated leg extension was set at 0°. Following the muscle function assessments, volunteers ingested 30mg of D 3-Creatine dissolved in 100ml H 2O for muscle mass assessment, before providing a pooled 24h urine collection and single urine samples at 48 and 72 h post consumption ( Clark et al., 2014).
Home-based exercise training programme (HBET)
Volunteers were required to complete 3 sets of 12 repetitions across 8 different exercises, every day, for 4 weeks. Each exercise was designed to be easily incorporated into activities of daily living to minimise the time-commitment required (e.g. bicep curls whilst cooking, see Figure 1). In total the exercise programme consisted of: squats, lunges, calf raises, bicep curls, triceps extensions, semi-incline press-ups, oblique twists and deadlifts. Participants were instructed to take 2 seconds to perform each phase (eccentric and concentric) of each exercise and to hold for 2 seconds at the mid-point of each exercise. Progression via increased resistance or time-under-tension was encouraged once the full complement of repetitions could be completed. Compliance to exercise was measured by self-report (see self-report log in Figure 1). An exercise would only be marked as complete if 3 sets of 12 repetitions had been performed within a day.
Measurement of whole-body muscle mass using D 3-creatine
Using a creatine-tracer measure of muscle mass ( Clark et al., 2014), D 3-creatine and D 3-creatinine enrichment, plus unlabelled creatine and creatinine in the urine was measured using high-performance liquid chromatography/mass spectrometry (HPLC/MS), as detailed in ( Stimpson et al., 2012). Total muscle mass was calculated using the following equation:
Total muscle mass
where MW Unlabelled and MW labelled represents the molecular weights of both unlabelled and labelled creatine, respectively. The estimated creatine pool size is then divided by 4.3 g/kg, which reflects the concentration of creatine in wet muscle.
Statistical analysis
Descriptive statistics were carried out on all datasets and checked for a normal distribution using the Shapiro-Wilk normality test. Datasets were analysed using paired Student’s t test to assess the effect of HBET, with GraphPad Prism Software v5 (La Jolla, CA, USA). All data is presented as mean ±SEM. Significance was set at P<0.05.
Results
Compliance, body weight and cardiovascular parameters
Using data from the self-report training logs, overall compliance to the HBET was 87.3±3.0% over the 4-week period of training. Adherence to each individual exercise was >86%, with the calf-raises being the most completed exercise (91%). No significant changes were found following HBET for body weight (79.3±4.7 vs. 78.9±4.6 kg), resting heart rate (71.9±3.1 vs. 71.4±3.9 bpm) or blood pressure (systolic: 144.4±3.4 vs. 140.7±4.2, diastolic: 92.2±2.5 vs. 89.0±2.4; average of 3 measurements).
Muscle function
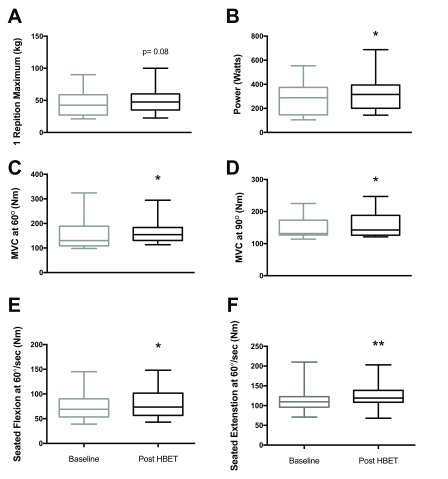
HBET did not elicit significant changes in leg extension 1-RM, handgrip strength or SPPBT; there was however, a trend for an increase in leg extension 1-RM (45.7±5.9 vs. 49.6±6.0 kg, P=0.08; Figure 2A). HBET did elicit significant increases in leg power (276.7±38.5 vs. 323.4±43.4 W, P<0.05; Figure 2B) and MVC at 60° (154.2±18.4 vs. 168.8±15.2 Nm, P<0.05; Figure 2C) and 90° (152.1±10.5 vs. 159.1±11.4 Nm, P<0.05; Figure 2D). There were also significant increases in peak torque recorded at 60°/sec during both seated flexion (74.7±8.3 vs. 80.8±8.6 Nm, P<0.05; Figure 2E) and extension (114.9±10.2 vs. 123.8±9.4 Nm, P<0.01; Figure 2F) after HBET.
Figure 2. Muscle (leg) function assessments, before and after home-based exercise training (HBET).
A) 1-RM leg extension (45.7±5.9 vs. 49.6±6.0 kg, P=0.08), B) Leg power via Nottingham Power Rig (276.7±38.5 vs. 323.4±43.4 W), C) MVC at 60° (154.2±18.4 vs. 168.8±15.2 Nm), D) MVC at 90° (152.1±10.5 vs. 159.1±11.4 Nm), E) Seated leg flexion at 60°/sec (74.7±8.3 vs. 80.8±8.6 Nm), F) Seated leg extension at 60°/sec (114.9±10.2 vs. 123.8±9.4 Nm). Baseline vs. post-HBET (mean ± SEM), n=12, *=p<0.05; **=p<0.01. MVC: Maximal voluntary contraction.
Muscle architecture
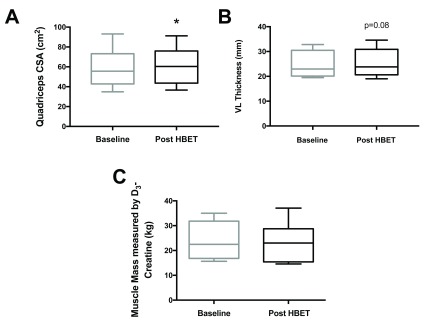
CSA of the thigh at 50% of thigh length significantly increased (57.5±5.4 vs. 59.0±5.3 cm 2, P<0.05; Figure 3A) after HBET. However, there was no significant increase in muscle thickness, fascicle length ( L f) or pennation angle ( θ pen) of the m. vastus lateralis. There was a trend for an increase in muscle thickness (25.0±1.6 vs. 25.5±1.7 mm, P=0.08; Figure 3B) after HBET.
Figure 3.
A) quadriceps cross-sectional area (CSA; 57.5±5.4 vs. 59.0 ± 5.3 cm 2); B) m. vastus lateralis (VL) thickness (25.0±1.6 vs. 25.5±1.7 mm, P=0.08); C) whole-body muscle mass, before and after home-based exercise training (HBET) (23.9±2.1 vs. 22.8±2.2 kg). (mean ± SEM), *=p<0.05, baseline vs. post-HBET.
Whole-body muscle mass measured by D 3-Creatine
Corresponding with no significant change in body weight, there was no significant difference in whole-body muscle mass as estimated by D 3-Creatine ( Figure 3C) after HBET (23.9±2.1 vs. 22.8±2.2 kg).
Sheet 1: Maximum Voluntary Contraction (MVC) at 60° and 90°, pre- and post 4-weeks of home-based whole-body exercise training. Sheet 2: Seated leg extension measures at 60, 180 and 240 deg/sec pre- and post 4-weeks of home-based whole-body exercise training. Sheet 3: Seated leg flexion at 60, 180 and 240 deg/sec pre- and post- 4-weeks of home-based whole-body exercise training. Sheet 4: Handgrip strength, single-leg 1-RM leg extension, SPPBT (short physical performance battery tests) and leg muscle power, measured pre- and post- 4-weeks of home-based whole-body exercise training. Sheet 5: Participant characteristics. Heart rate (HR), systolic and diastolic blood pressure (BP) and body weight, pre- and post- 4-weeks of whole-body home-based exercise training. Sheet 6: Quadriceps cross-sectional area (CSA), vastus lateralis muscle thickness, fascicle length and pennation angle measured by ultrasound pre- and post- 4-weeks of whole-body home-based exercise training. Sheet 7: Muscle mass measured by using D 3-creatine, pre- and post- 4 weeks of whole-body home-based exercise training.
Copyright: © 2017 Cegielski J et al.
Data associated with the article are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Discussion
In this pilot study, we show that lifestyle-integrated, whole-body HBET has the potential to meaningfully improve muscle function in older adults. We have shown that this training mode can increase leg power by 16.9% in just 4-weeks. Although lower than the 37% power increase demonstrated in a solely lower-extremity focused HBET programme, this study was conducted over an 8-week period ( DeBolt & McCubbin, 2004), suggesting that if the magnitude of increase was to continue at a constant rate, our training mode may elicit similar improvements. Additionally, we demonstrate increases in muscle strength (via MVC at 60°) similar to that observed in response to a 6-week, fully-supervised, gym-based training study ( Brook et al., 2016). Furthermore, despite no significant increase, there was a positive trend in the leg extension 1-RM, similar to that seen in an 8-week HBET study by Zion et al. (2003). Thus, while muscle function adaptations to HBET were numerically lesser compared to longer-term structured exercise regimens (some requiring specialist equipment), our data support the notion that just 4-weeks of a ‘lifestyle-integrated’ HBET meaningfully improves muscle function.
Despite these positive results, no changes in handgrip strength were found, a similar result to Nelson et al. (2004), who implemented a 6-month home-based whole-body exercise programme in 70 male and female elderly individuals. This may be due to a lack of exercises specifically targeting the forearm flexors. Indeed, although it is well-established that extant grip strength represents a biomarker of muscle function in older adults ( Bassey & Harries, 1993), our data suggests that it is an insensitive biomarker for important functional and mass gains in other muscle groups (e.g. the legs) following certain exercise interventions.
Importantly, increases in thigh CSA (and a trend towards increased muscle thickness), which may partly explain the functional improvements, were observed. Measures of thigh CSA by ultrasound have been positively correlated with those by MRI ( Reeves et al., 2004), therefore suggesting (leg) muscle hypertrophy in this study. However, since this occurred in the absence of detectable changes in whole-body muscle mass as measured by D 3-Creatine, we speculate i) that preferential hypertrophy of leg muscles occurred, but remained undetectable on a whole-body level; or ii) that measurement of whole-body muscle mass was below the detection threshold for the D 3-creatine method.
We acknowledge limitations to our study design. The use of validated physical activity monitors (e.g. Actiheart, CamNtech, Cambridge, UK) to assess compliance to exercise would have provided greater information on the adoption of, and adherence to our exercise programme. Similarly, the use of interactive technologies (e.g. training applications for tablets/smartphones) for motivation and/or instruction may have improved adherence ( Silveira et al., 2013). The lack of improvements in SPPBT were likely a result of our volunteers achieving optimal scores before the intervention.
To conclude, our findings demonstrate that significant increases in muscle mass, maximal voluntary contraction, maximal power and isokinetic strength can be achieved with just 4-weeks of unsupervised, lifestyle-integrated HBET in older adults. These improvements were achieved via cost-effective means, without the requirement for specialist equipment, facilities or supervision ( DeBolt & McCubbin, 2004; Jette et al., 1996; Zion et al., 2003). With high compliance and beneficial physiological effects in only a 4-week period, this study highlights the potential for lifestyle-integrated HBET to improve skeletal muscle ‘health’ in older adults. As increases in muscle mass and strength are positively correlated with overall physical function ( Liu & Latham, 2009), this novel training mode may be of particular benefit to older frail/(pre-) sarcopenic adults.
Data availability
The data referenced by this article are under copyright with the following copyright statement: Copyright: © 2017 Cegielski J et al.
Data associated with the article are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication). http://creativecommons.org/publicdomain/zero/1.0/
Dataset 1: Raw data supporting the findings in this study.
Sheet 1: Maximum Voluntary Contraction (MVC) at 60° and 90°, pre- and post 4-weeks of home-based whole-body exercise training.
Sheet 2: Seated leg extension measures at 60, 180 and 240 deg/sec pre- and post 4-weeks of home-based whole-body exercise training
Sheet 3: Seated leg flexion at 60, 180 and 240 deg/sec pre- and post- 4-weeks of home-based whole-body exercise training
Sheet 4: Handgrip strength, single-leg 1-RM leg extension, SPPBT (short physical performance battery tests) and leg muscle power, measured pre- and post- 4-weeks of home-based whole-body exercise training
Sheet 5: Participant characteristics. Heart rate (HR), systolic and diastolic blood pressure (BP) and body weight, pre- and post- 4-weeks of whole-body home-based exercise training.
Sheet 6: Quadriceps cross-sectional area (CSA), vastus lateralis muscle thickness, fascicle length and pennation angle measured by ultrasound pre- and post- 4-weeks of whole-body home-based exercise training.
Sheet 7: Muscle mass measured by using D 3-creatine, pre- and post- 4 weeks of whole-body home-based exercise training.
DOI, 10.5256/f1000research.11894.d170288 ( Cegielski et al., 2017).
Funding Statement
This work was supported by a Medical Research Council [MR/K00414X/1] and Arthritis Research UK [19891] infrastructure award. The stable-isotope methodologies used in in this work were developed and funded via Medical Research Council Confidence in Concept Awards [CiC12019, CiC2014035]. JC is supported by a PhD studentship [RGS117347] from The Abbeyfield Research Foundation (charity number 1167685).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; referees: 2 approved]
References
- Bassett SF, Prapavessis H: Home-based physical therapy intervention with adherence-enhancing strategies versus clinic-based management for patients with ankle sprains. Phys Ther. 2007;87(9):1132–43. 10.2522/ptj.20060260 [DOI] [PubMed] [Google Scholar]
- Bassey EJ, Short AH: A new method for measuring power output in a single leg extension: feasibility, reliability and validity. Eur J Appl Physiol Occup Physiol. 1990;60(5):385–390. 10.1007/BF00713504 [DOI] [PubMed] [Google Scholar]
- Bassey EJ, Harries UJ: Normal values for handgrip strength in 920 men and women aged over 65 years, and longitudinal changes over 4 years in 620 survivors. Clin Sci (Lond). 1993;84(3):331–337. [DOI] [PubMed] [Google Scholar]
- Brook MS, Wilkinson DJ, Mitchell WK, et al. : Synchronous deficits in cumulative muscle protein synthesis and ribosomal biogenesis underlie age-related anabolic resistance to exercise in humans. J Physiol. 2016;594(24):7399–7417. 10.1113/JP272857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull FC, Biddle S, Buchner D, et al. : Physical activity guidelines in the U.K.: Review and Recommendations. School of Sport, Exercise and Health Sciences, Loughborough University,2010;1–72. Reference Source [Google Scholar]
- Cegielski J, Brook M, Quinlan J, et al. : Dataset 1 in: A 4-week lifestyle-integrated home-based exercise training programme elicits improvements in physical function and lean mass in older men and women: a pilot study. F1000Research. 2017. Data Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CF, Lin KC, Chen WM, et al. : Effects of a Home-Based Resistance Training Program on Recovery From Total Hip Replacement Surgery: Feasibility and Pilot Testing. J Nurs Res. 2017;25(1):21–30. 10.1097/jnr.0000000000000128 [DOI] [PubMed] [Google Scholar]
- Clark RV, Walker AC, O'Connor-Semmes RL, et al. : Total body skeletal muscle mass: estimation by creatine ( methyl-d 3) dilution in humans. J Appl Physiol (1985). 2014;116(12):1605–13. 10.1152/japplphysiol.00045.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBolt LS, McCubbin JA: The Effects of Home-Based Resistance Exercise on Balance, Power, and Mobility in Adults with Multiple Sclerosis. Arch Phys Med Rehabil. 2004;85(2):290–297. 10.1016/j.apmr.2003.06.003 [DOI] [PubMed] [Google Scholar]
- Department of Health, Physical Activity, H.I. and P.: Start Active, Stay Active - A report on physical activity for health from the four home countries’ Chief Medical Officers.2011. Reference Source [Google Scholar]
- Franchi MV, Atherton PJ, Reeves ND, et al. : Architectural, functional and molecular responses to concentric and eccentric loading in human skeletal muscle. Acta Physiol (Oxf). 2014;210(3):642–54. 10.1111/apha.12225 [DOI] [PubMed] [Google Scholar]
- Gardner MM, Buchner DM, Robertson MC, et al. : Practical implementation of an exercise-based falls prevention programme. Age Ageing. 2001;30(1):77–83. 10.1093/ageing/30.1.77 [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, et al. : A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Hong J, Kim J, Kim SW, et al. : Effects of home-based tele-exercise on sarcopenia among community-dwelling elderly adults: Body composition and functional fitness. Exp Gerontol. 2017;87(Pt A):33–39. 10.1016/j.exger.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Ito S, Hashimoto M, Aduma S, et al. : Effectiveness of locomotion training in a home visit preventive care project: one-group pre-intervention versus post-intervention design study. J Orthop Sci. 2015;20(6):1078–1084. 10.1007/s00776-015-0760-2 [DOI] [PubMed] [Google Scholar]
- Jefferis BJ, Sartini C, Lee IM, et al. : Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14(1):382. 10.1186/1471-2458-14-382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jette AM, Harris BA, Sleeper L, et al. : A Home-based Exercise Program for Nondisabled Older Adults. J Am Geriatr Soc. 1996;44(6):644–649. 10.1111/j.1532-5415.1996.tb01825.x [DOI] [PubMed] [Google Scholar]
- Jette AM, Lachman M, Giorgetti MM, et al. : Exercise--It’s never too late: The strong-for-life program. Am J Public Health. 1999;89(1):66–72. 10.2105/AJPH.89.1.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CJ, Latham NK: Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;3(CD002759):1–227. 10.1002/14651858.CD002759.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruya K, Asakawa Y, Ishibashi H, et al. : Effect of a simple and adherent home exercise program on the physical function of community dwelling adults sixty years of age and older with pre-sarcopenia or sarcopenia. J Phys Ther Sci. 2016;28(11):3183–3188. 10.1589/jpts.28.3183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson ME, Layne JE, Bernstein MJ, et al. : The Effects of Multidimensional Home-Based Exercise on Functional Performance in Elderly People. J Gerontol A Biol Sci Med Sci. 2004;59(2):154–60. 10.1093/gerona/59.2.M154 [DOI] [PubMed] [Google Scholar]
- Phillips B, Williams J, Atherton P, et al. : Resistance exercise training improves age-related declines in leg vascular conductance and rejuvenates acute leg blood flow responses to feeding and exercise. J Appl Physiol (1985). 2012;112(3):347–53. 10.1152/japplphysiol.01031.2011 [DOI] [PubMed] [Google Scholar]
- Plotnikoff RC, Eves N, Jung M, et al. : Multicomponent, home-based resistance training for obese adults with type 2 diabetes: a randomized controlled trial. Int J Obes (Lond). 2010;34(12):1733–41. 10.1038/ijo.2010.109 [DOI] [PubMed] [Google Scholar]
- Reeves ND, Maganaris CN, Narici MV: Ultrasonographic assessment of human skeletal muscle size. Eur J Appl Physiol. 2004;91(1):116–118. 10.1007/s00421-003-0961-9 [DOI] [PubMed] [Google Scholar]
- Ribeiro F, Teixeira F, Brochado G, et al. : Impact of low cost strength training of dorsi- and plantar flexors on balance and functional mobility in institutionalized elderly people. Geriatr Gerontol Int. 2009;9(1):75–80. 10.1111/j.1447-0594.2008.00500.x [DOI] [PubMed] [Google Scholar]
- Rudrappa SS, Wilkinson DJ, Greenhaff PL, et al. : Human Skeletal Muscle Disuse Atrophy: Effects on Muscle Protein Synthesis, Breakdown, and Insulin Resistance-A Qualitative Review. Front Physiol. 2016;7:361. 10.3389/fphys.2016.00361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveira P, van de Langenberg R, van Het Reve E, et al. : Tablet-based strength-balance training to motivate and improve adherence to exercise in independently living older people: a phase II preclinical exploratory trial. J Med Internet Res. 2013;15(8):e159. 10.2196/jmir.2579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpson SA, Turner SM, Clifton LG, et al. : Total-body creatine pool size and skeletal muscle mass determination by creatine-( methyl-D 3) dilution in rats. J Appl Physiol (1985). 2012;112(11):1940–1948. 10.1152/japplphysiol.00122.2012 [DOI] [PubMed] [Google Scholar]
- Yamauchi J, Nakayama S, Ishii N: Effects of bodyweight-based exercise training on muscle functions of leg multi-joint movement in elderly individuals. Geriatr Gerontol Int. 2009;9(3):262–269. 10.1111/j.1447-0594.2009.00530.x [DOI] [PubMed] [Google Scholar]
- Zion AS, De Meersman R, Diamond BE, et al. : A home-based resistance-training program using elastic bands for elderly patients with orthostatic hypotension. Clin Auton Res. 2003;13(4):286–292. 10.1007/s10286-003-0117-3 [DOI] [PubMed] [Google Scholar]
- Zlot AI, Librett J, Buchner D, et al. : Environmental, Transportation, Social, and Time Barriers to Physical Activity. J Phys Act Health. 2006;3(1):15–21. 10.1123/jpah.3.1.15 [DOI] [Google Scholar]