Abstract
This study examines attention-deficit/hyperactivity disorder (ADHD) and callous-unemotional (CU) traits as moderators of the association between conduct problems (CP) and young adult functioning. Young adults (n=283; Mage=20.82 years; 53.4% female), oversampled for attention and behavior problems, provided self-ratings of ADHD, CP, and CU, and adaptive functioning and psychopathology. ADHD and CU simultaneously moderated relationships between CP and family functioning, tobacco use, and internalizing symptoms. In addition, ADHD moderated the relation between CP and job functioning, and main effects of ADHD in the expected direction were found for educational performance and drug use. CU was associated with poorer educational outcomes. Interestingly, no ADHD, CU, or CP effects were observed for reported alcohol use. Our results highlight the importance of considering ADHD and CU in understanding the impact of CP on young adult functioning and psychopathology, and point to the importance of continued work on this topic.
1. Introduction
Rates of criminal behavior peak in late adolescence and then steadily decline as adolescents age into adulthood (Loeber and Stallings, 2011). More than 70% of adolescents report committing at least one delinquent act by age 18 (Sibley et al., 2011), although by age 25, less than half of individuals previously involved in delinquency continue to engage in aggressive and violent behavior (Loeber and Stallings, 2011). While the course of aggressive behavior is transient for many, adolescents who continue to exhibit aggressive behavior into adulthood follow a chronic course of offending that may worsen over time (Loeber and Stallings, 2011). In spite of this, more remains to be learned about conduct problems (CP) in young adulthood, and even less is known about factors associated with persistent CP or how CP is associated with functional impairments during this critical developmental period.
Numerous studies of childhood report that the course of CP is more persistent and severe in the presence of attention-deficit/hyperactivity disorder (ADHD). The combination of ADHD and CP is associated with interpersonal difficulties and academic problems that are more severe than impairments in children with CP or ADHD alone (Waschbusch, 2002). Further, the co-occurrence of CP and ADHD is related to an earlier emergence and more stable course of delinquent behavior (Mohr-Jensen and Steinhausen, 2016), and both ADHD and CP contribute to the initiation and maintenance of cigarette, alcohol, and marijuana use in adolescents (Sibley et al., 2014). Although little is known about the co-occurrence of CP and ADHD into young adulthood, it is likely that the impact of co-occurring ADHD and CP on daily life functioning is quite severe. In fact, of prison inmates arrested for drug and violent offenses, 40% have been reported to have a diagnosis of ADHD (Ginsberg et al., 2010).
Childhood research has identified callous-unemotional traits (CU) to be an important moderator of CP (Salekin and Frick, 2005). CU traits, which include lack of remorse, shallow affect, not caring about performance on important tasks, and lack of empathy, are associated with severe and persistent antisocial behavior, as well as distinct patterns of dysfunction across multiple domains (Frick et al., 2014). It is estimated that at least a third of children with CP exhibit CU traits (Houghton et al., 2005), and co-occurring CP/CU foreshadows a more severe course of aggressive and violent behavior compared to either CP or CU alone. Given the importance of CU traits, the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2015) now includes a specifier to identify individuals with conduct disorder and CU traits. CU traits have been documented from early childhood (Graziano et al., 2016) into early adulthood (Byrd et al., 2013). However, little work has specifically examined the impact of CU on functioning in young adulthood, and the few existing studies have shown contrasting findings (Bartol and Miller, 2014; Byrd et al., 2013). For example, one study examining CU traits among college students receiving special education accommodations found no unique association between CU and impairment among university students (Bartol and Miller, 2014). In contrast, examination of CU in an at-risk community sample of boys (ages 12–20) yielded distinct associations between CU and a range of adverse outcomes, including self-reported and official records of delinquent behavior, heavy drinking, drug use, depression, employment difficulties, and interpersonal difficulties (Byrd et al., 2013).
CP, ADHD, and CU often begin in childhood and continue into adulthood. These constructs often overlap (Haas and Waschbusch, 2012), and the combination of CP and ADHD or CP and CU appears to portend substantial risk for the course of violent and aggressive behavior and functioning in daily life, more generally. Specifically, Waschbusch and Willoughby (2008), found that ADHD and CU simultaneously moderate the association between CP and academic impairment, classroom functioning, and reactive aggression. The effect of CU on CP was more pronounced at lower versus higher levels of ADHD, although both ADHD and CU increased the severity of impairment associated with CP. Apart from this one study, little is known about the simultaneous impact of CP, ADHD, and CU on functional impairment, and no studies have examined whether this same pattern of simultaneous moderation occurs among young adults.
It is critical to examine the impact of CU and ADHD on CP in young adulthood, as these factors have been shown to worsen the course and severity of CP in childhood, and the consequences of CP in young adulthood, primarily arrest, incarceration, and other contacts with law enforcement, have grave consequences on long-term functioning (Loeber and Stallings, 2011). The increased independence and decreased parental monitoring associated with young adulthood (Arnett, 2007) may magnify the impact of ADHD and CU on CP and it is important to examine how these factors impact important areas of young adult functioning, including interpersonal relationships, school and job functioning, drug and alcohol use, and internalizing problems.
The goal of this study is to examine ADHD and CU as moderators of the association between CP and daily life functioning and psychopathology in emerging adults. To provide the most comprehensive examination, simultaneous moderation of ADHD and CU on CP and peer and family functioning, academic and job performance, tobacco, alcohol, and drug use, as well as internalizing problems were examined. Given emerging literature demonstrating simultaneous moderation in childhood (Waschbusch and Willoughby, 2008), it was hypothesized that ADHD and CU would simultaneously moderate associations between CP and impairment in young adults, with the effect of CU on CP magnified at lower rather than higher levels of ADHD.
2. Methods
Participants were 283 young adults from a rural town in the mid-Atlantic United States, recruited through radio advertisements, announcements made in courses at the University at which the study was conducted, fliers posted on community and campus bulletin boards and in local medical clinics, websites, and word of mouth. Two groups of participants were recruited: those who self-identified as ever being diagnosed with ADHD (n=98) and those who had never been diagnosed with ADHD (n=185). This was done to oversample for attention and behavior problems. Eligibility criteria for the non-ADHD sample included no previous diagnosis of ADHD, 18–25 years of age (inclusive), Native English speakers, and at least a high school education. All participants were required to have a medical history without: concussion or loss of consciousness for more than 10 minutes, seizures, epilepsy, encephalitis, meningitis, autism spectrum disorder, musculoskeletal or neurological disorder, stroke or transient ischemic attack, psychiatric disorder involving psychosis, or immediate family members with a history of psychosis, movement disorder or autism. These criteria also applied to young adults with ADHD, who were also required to self-report a previous formal diagnosis of ADHD. Interested individuals were screened for eligibility in person, over the phone, or via a web-based survey platform (Qualtrics, LLC) prior to obtaining consent, which was obtained through the same website. Participants completed ratings of their current symptoms and adaptive functioning via the secure online website. Data were collected from June 2015 to May 2016. All procedures were approved by the university Institutional Review Board and were consistent with the 1964 Declaration of Helsinki.
Participants in the non-ADHD and ADHD groups were combined for the current study, and included 151 women and 132 men with a mean age of 20.82 (SD=1.87). The majority (84.1%) were White and not Hispanic/Latino (91.5%). Additionally, 6.7% of the sample identified as Asian, 3.2% identified as Black, and 6.0% identified as mixed race, which is consistent with the demographics of the community from which the sample was drawn. The majority of the sample identified as college students (85.9%), while 11.7% identified as employed, and the remainder reported they were neither employed nor in school. A total of 62 (21.09%) participants reported currently taking stimulant medication for ADHD. An additional 3 more participants were medicated with nonstimulant medication (i.e., atomoxetine), for a total of 22.97% of the sample receiving medication for ADHD.
2.1. Measures
2.1.1. Independent variables
2.1.1.1. CP
The Aggressive Behavior subscale of the Adult Self Report Scale (Achenbach and Rescorla, 2003) measured CP. Items are rated using 3-point Likert scales with the following anchors: 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true). This measure is widely used and employs age-based normative data to identify problematic behavior. Previous research has reported excellent psychometric properties of the aggressive behavior subscale, including internal consistency of 0.86 and test-retest reliability of 0.87 (Achenbach et al., 2005). Similarly strong psychometric properties are reported for other subscales, described below. For our study, the aggressive behavior T-score was used in analyses, with scores 65–69 in the borderline clinical range and scores 70 and greater indicating clinically elevated conduct problems.
2.1.1.2. ADHD
The Conners Adult ADHD Rating Scale (CAARS) measured self-reported ADHD. The CAARS is a 66-item measure, with items scored on a 4-point Likert scale ranging from 0 (not at all), 1 (just a little), 2 (pretty much), to 3 (very much). The CAARS produces DSM-IV subscales, and the total symptoms T-score was used for the current study, with higher scores indicating greater ADHD symptoms (Erhardt et al., 1999). T-scores greater than 65 are considered to be in the clinical range. The CAARS has demonstrated high internal consistency and test-retest reliability (Erhardt et al., 1999).
2.1.1.3. CU
CU was calculated using the adolescent/adult self-report version of the Inventory for Callous-Unemotional Traits (ICU; Frick et al., 2004). The ICU includes 24 items rated on a 4-point scale from 0 (not at all true) to 3 (definitely true). Previous research has demonstrated strong psychometric properties for the ICU in samples of children and young adults (Byrd et al., 2013). The total score, which is computed by reverse coding items that assess positive traits and then summing all items, was used for this study. Higher scores indicate more severe CU traits.
2.1.2. Dependent variables
2.1.2.1. Adaptive functioning
Peer, family, academic, and job functioning were measured using the adaptive functioning subscales on the ASR (described above). Items are rated on a 3-point scale from 0 (not true) to 2 (very true or often true), with higher scores indicating better functioning.
2.1.2.2. Psychopathology
ASR subscales measuring tobacco, alcohol, and drug use, as well as internalizing problems (i.e., depression/anxiety symptoms) were also used for analyses. Items are rated on a three-point scale from 0 (not true) to 2 (very true or often true). T-scores were used in analyses, with higher scores indicating greater use and greater symptomology.
2.2. Data Analytic Plan
Associations between CP, CU, and ADHD with all dependent variables were quantified using correlation coefficients. Then, separate ordinary least squares regression models were run, simultaneously regressing CP, CU, and ADHD and their interactions on each outcome of interest. Significant three-way interactions were followed-up with simple slopes difference tests using values of the moderators one standard deviation above and below their mean value. The high score for ADHD of 68.04 (calculated by the mean plus 1 standard deviation: 51.80 + 16.24) was in the clinical range, and the high score for CP of 59.95 (calculated by the mean plus 1 standard deviation: 53.58 + 6.37), approached the clinically elevated range. The high score for CU was 27.21 (calculated by the mean plus 1 standard deviation: 18.82 + 8.39), which was consistent with CU levels reported among at-risk adults (Byrd et al., 2013) and adolescent criminal offenders (Kimonis et al., 2008), suggesting that analyses include young adults with clinically elevated psychopathology. Significant two-way interactions were analyzed similarly.
3. Results
Descriptive statistics and bivariate correlations for independent and dependent variables appear in Table 1. Significant (p<0.05) associations between independent variables and functioning scales and internalizing symptoms emerged. Few significant associations between independent variables and substance use emerged. Regression analyses are reported in Table 2.
Table 1.
Descriptive statistics and bivariate correlations
| Descriptive statistics | Bivariate correlations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| N | M | Range | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Independent variable | |||||||||||||||
| 1. ADHD | 283 | 51.80 | 30–90 | 16.24 | -- | ||||||||||
| 2. CP | 283 | 53.58 | 50–100 | 6.37 | 0.58** | -- | |||||||||
| 3. CU | 283 | 18.82 | 3–45 | 8.39 | 0.28** | 0.30** | -- | ||||||||
| Functioning | |||||||||||||||
| 4. Peer | 283 | 50.65 | 23–60 | 7.39 | −0.10+ | −0.20** | −0.23** | -- | |||||||
| 5. Family | 282 | 43.07 | 20–58 | 11.04 | −0.25** | −0.24** | −0.17** | 0.21** | -- | ||||||
| 6. Education | 261 | 49.61 | 23–60 | 9.77 | −0.51** | −0.39** | −0.33** | 0.25** | 0.29** | -- | |||||
| 7. Job | 232 | 49.03 | 24–58 | 7.61 | −0.46** | −0.42** | −0.25** | 0.23** | 0.29** | 0.63** | -- | ||||
| Psychopathology | |||||||||||||||
| 8. Tobacco use | 282 | 50.66 | 50–67 | 1.99 | 0.07 | 0.07 | 0.14* | −0.04 | 0.05 | −0.06 | −0.04 | -- | |||
| 9. Alcohol use | 283 | 60.07 | 50–84 | 7.96 | 0.09 | 0.02 | 0.01 | 0.19** | 0.02 | −0.10 | −0.18* | 0.11+ | -- | ||
| 10. Drug use | 283 | 54.42 | 50–100 | 8.76 | 0.22** | 0.08 | 0.07 | 0.03 | 0.08 | −0.16* | −0.08 | 0.17** | 0.41** | -- | |
| 11. Internalizing | 283 | 55.66 | 50–100 | 8.75 | 0.55** | 0.70** | 0.21** | −0.30** | −0.27** | −0.54** | −0.54** | −0.05 | −0.05 | 0.08 | -- |
Note. For predictor variables, substance use variables, and internalizing problems higher scores indicate greater impairment. For all other measures, higher scores indicate more adaptive functioning.
p<0.01,
p<0.05,
p<0.10
Table 2.
Unstandardized regression coefficients
| Functioning | Psychopathology | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Effect | Peer | Family | Education | Job | Tobacco Use |
Alcohol Use |
Drug Use |
Internalizing symptoms |
| Intercept | 50.91** | 41.34** | 49.21** | 48.06** | 50.57** | 60.47** | 54.60** | 56.19** |
| CP | −0.12 | −0.65** | −0.34 | −0.59** | 0.01 | 0.04 | >0.01 | 0.94** |
| ADHD | >0.01 | −0.04 | −0.23** | −0.11** | 0.01 | 0.05 | 0.12** | 0.10** |
| CU | −0.20** | −0.07 | −0.22** | 0.04** | 0.04** | −0.04 | −0.02 | −0.06 |
| ADHD * CP | >0.01 | 0.01 | >0.01 | 0.02* | >0.01 | −0.01 | >0.01 | −0.01 |
| CP * CU | −0.03* | 0.05** | >0.01 | >0.01 | 0.02** | 0.02 | −0.01 | −0.02 |
| ADHD * CU | >0.01 | 0.01+ | >0.01 | >0.01 | >0.01 | >0.01 | 0.01+ | >0.01 |
| ADHD * CP * CU | >0.01+ | >0.01* | >0.01 | >0.01 | >0.01** | >0.01 | >0.01 | >0.02* |
Note. Centered independent variables were used in analyses.
p<0.01,
p<0.05,
p<0.10
3.1. Adaptive Functioning
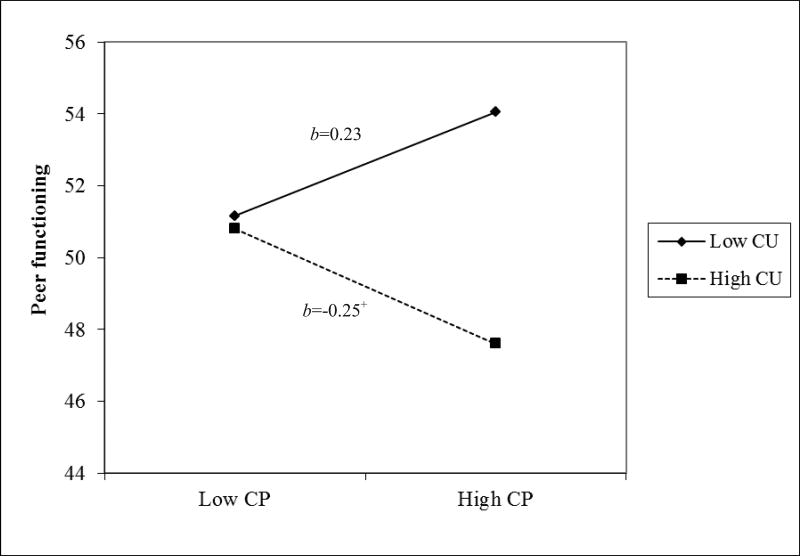
3.1.1. Peer functioning
A significant CP * CU interaction emerged (Figure 1). Simple slope tests revealed that the worsening in peer functioning from low to high CP was significant at the p<0.10 level for young adults with high CU, but the change in peer functioning at low levels of CU was non-significant. ADHD did not moderate associations between CP and peer functioning.
Figure 1. Peer functioning as a function of the two-way interaction between CP and CU.
Note. Higher peer functioning scores indicate more adaptive functioning. **p<0.01, *p<0.05, +p<0.10
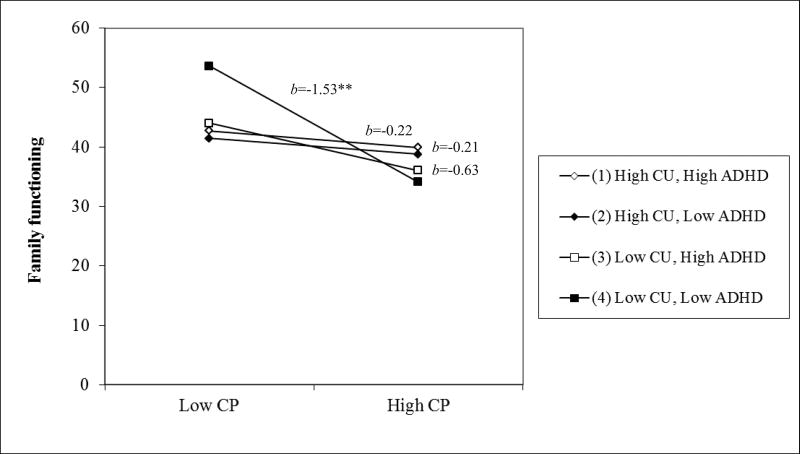
3.1.2. Family functioning
An ADHD * CP * CU effect emerged. Simple slopes tests (Figure 2) showed higher CP was associated with worse family functioning when CU and ADHD were low, but CP and family functioning were not associated when either CU or ADHD was high.
Figure 2. Family impairment as a function of the three-way interaction between CP, ADHD, and CU.
Note. Higher family functioning scores indicate more adaptive functioning. **p<0.01, *p<0.05, +p<0.10
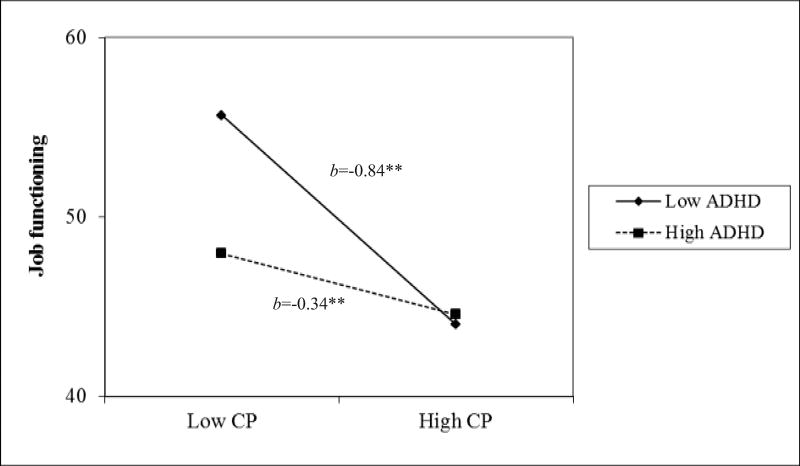
3.1.3. Academic and job performance
No interaction effects emerged for academic performance, although main effects of ADHD and CU emerged, with both associated with poorer performance. CP was not associated with academic functioning. A significant ADHD*×CP interaction emerged regarding job impairment (Figure 3); higher CP was associated with poorer work performance and this was intensified when ADHD was low versus high.
Figure 3. Job performance impairment as a function of the two-way interaction between ADHD and CP.
Note. High job functioning scores indicate more adaptive functioning. **p<0.01, *p<0.05, +p<0.10
3.2. Psychopathology
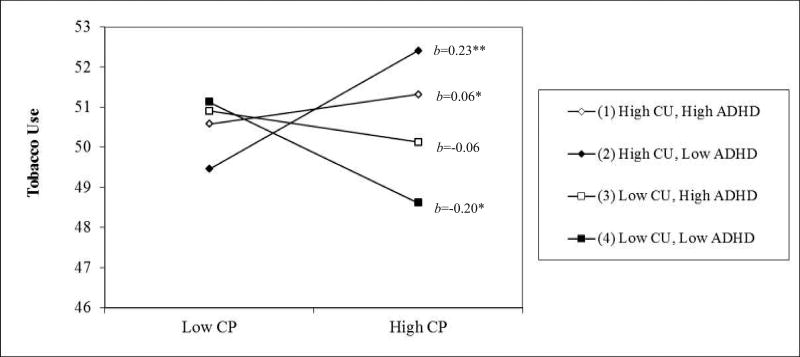
3.2.1. Tobacco use
An ADHD * CP * CU effect emerged for tobacco use (Figure 4). Tobacco use increased when going from low to high CP when CU was high, regardless of ADHD. However, tobacco use increased more drastically for low versus high ADHD, when CU is high. Tobacco use decreased when going from low to high CP when CU is low, regardless of ADHD. However, use decreased more drastically for low versus high ADHD, when CU is low.
Figure 4. Tobacco use as a function of the three-way interaction between CP, ADHD, and CU.
Note. Higher tobacco use scores indicate greater use. **p<0.01, *p<0.05, +p<0.10
3.2.2. Alcohol and drug use
No statistically significant effects emerged related to alcohol use. A significant effect of ADHD emerged for drug use, but neither CP nor CU effects emerged.
3.2.3. Internalizing symptoms
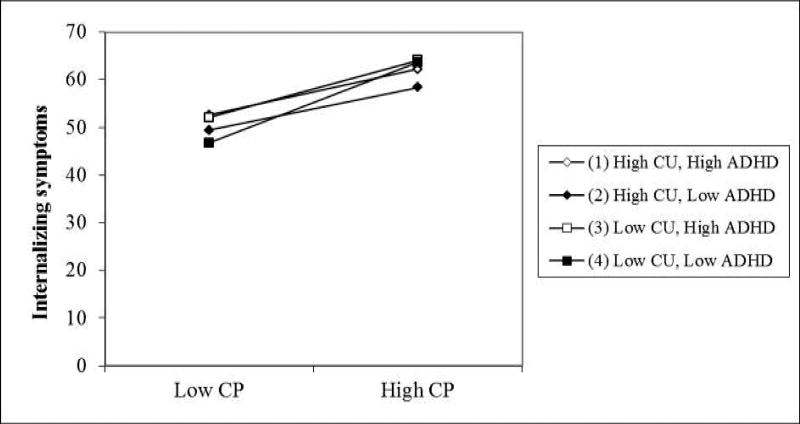
With regard to internalizing symptoms, a significant ADHD * CP * CP interaction emerged. Internalizing symptoms increased when going from low to high CP regardless of CU and ADHD (Figure 5). However, internalizing symptoms increased more drastically when CU was low and ADHD is low.
Figure 5. Internalizing symptoms as a function of the three-way interaction between CP, ADHD, and CU.
Note. Higher internalizing symptom scores indicate greater symptom severity. Simple slopes tests were all significantly different than zero: (High CU, High ADHD): b=0.76**; (High CU, Low ADHD): b=0.71**; (Low CU, High ADHD): b=0.95**; (Low CU, Low ADHD): b=1.34**. **p<0.01, *p<0.05, +p<0.10
4. Discussion
This study examined the moderating effects of ADHD and CU on associations between CP and young adult functioning. ADHD and CU simultaneously moderated relationships between CP and family functioning, tobacco use, and internalizing symptoms, although the direction of effects varied. ADHD moderated the relation between CP and job functioning, and effects of ADHD in the expected direction were found for educational performance and drug use. Greater CU was associated with poorer academic functioning. Interestingly, no effects of ADHD, CU, or CP were observed for reported alcohol use. These results are discussed herein.
4.1. Adaptive Functioning
Individuals reporting CP, CU, or ADHD experienced poorer family functioning compared to individuals reporting low levels on all of these variables. Thus, the decline in family functioning from low to high CP was most dramatic for individuals reporting low ADHD and low CU. These findings are consistent with the well-documented parent-child difficulties of children with ADHD, CP (Johnston and Chronis-Tuscano, 2014), and emerging work on CU (Waller et al., 2013). However, we did not find additive effects of ADHD and CU on CP as anticipated. It may be that difficulties in self-perception, particularly overestimating functioning, in objectively impaired domains, documented among individuals with ADHD and CP (Owens et al., 2007), reduced our ability to detect these effect. Thus, different results may emerge had collateral ratings from family members been collected. Examination of the mean level of family functioning in the entire sample (Table 2) demonstrates lower than normative family functioning. Therefore it may be that the family functioning of young adults in our sample, regardless of ADHD, CU, and CP was associated with family strain, perhaps due to financial strain and conflict related to developing independence at this developmental age. A different pattern emerged for peer functioning, as CU moderated the effect of CP. With increasing CP, peer functioning decreased more drastically when CU was high versus low, which fits with childhood research (Waschbusch and Willoughby, 2008), and some work showing a link between CU and romantic relationship functioning (Byrd et al., 2013). It is notable that these effects emerged when CU did not worsen effects on family functioning. Peer relationships are highly salient to young adults (e.g., Swenson et al., 2010), potentially more than their relationships with parents and family, as many of the individuals in the current study were living at with peers, away from their parents.
Neither ADHD nor CU moderated associations between CP and academic and job performance. Instead, ADHD and CU predicted academic functioning and ADHD moderated the impact of CP on job performance. Our findings linking ADHD with academic and job performance are consistent with many studies (e.g., Kuriyan et al., 2013). Similarly, links between ADHD and CP on occupational functioning have been reported (Kuriyan et al., 2013). While less is known about CU and academic deficits, some studies demonstrate links between CU and academic problems (Waschbusch and Willoughby, 2008). Although evidence of simultaneous moderation did not emerge as hypothesized, and we did not find effects of CU on job functioning, our sample, consisting primarily of college students not yet employed, may have had reduced variability to detect more effects in these areas.
4.2. Psychopathology
The pronounced effect of CU on CP and tobacco use at low levels of ADHD is consistent with childhood research examining simultaneous moderation of ADHD and CU on CP (Waschbusch and Willoughby, 2008). Interestingly, tobacco use decreased from low to high CP when CU was low, and the magnitude of this effect was pronounced when ADHD was low versus high. This decrease in tobacco use when CP increased was unexpected, as ADHD and CP have been shown to increase the risk of tobacco use (Molina and Pelham, 2003). However, cigarette use has declined considerably nationwide (Bauer et al., 2000), and the university at which data were collected had a university-wide policy confining smoking to designated areas, which may have limited opportunities for tobacco use. More nuanced assessment of tobacco use, including e-cigarette and hookah use, may have yielded a different pattern of findings, as their use has been increasing substantially among young adults (Holtzman et al. 2013; Sutfin et al., 2013).
While we found an effect of ADHD on drug use, consistent with previous research (Molina and Pelham, 2003), no effects on alcohol use emerged. Our composite measure of alcohol use in the ASR may not have been sensitive to subtle differences in general alcohol use versus problematic use. Alternatively, our null findings may be related to the normative increase in alcohol use reported among young adults, regardless of CP, ADHD, or CU, and it may be expected that effects would emerge as young adults transition to more professional activities, such as obtaining a job and home, marriage, and parenthood, as has been shown in at least one study of young adults with ADHD (Molina et al., 2007).
Higher levels of CP were associated with greater depressive symptoms regardless of ADHD and CU, although depressive symptoms increased more drastically when CU was low and ADHD was low. In fact, results suggested that ADHD and CU may be somewhat protective of internalizing problems. Given associations between CP (Lahey et al., 2002), ADHD (Meinzer et al., 2014), and one study documenting a link between the callousness subscale of the ICU and depression (Byrd et al., 2013), it was expected that the effect of CP on internalizing symptoms may be more pronounced when both ADHD and CU were high. However, our measure of internalizing problems included both depression and anxiety symptoms. Some literature (e.g., Kubak and Salekin, 2009) shows that individuals high in CU experience especially low levels of anxiety, and our measure of internalizing problems may have been too coarse to detect potentially unique variance in internalizing psychopathology.
Several limitations of the current study deserve mention. First, these findings are based solely on self-report. Adults with ADHD have been shown to have self-perception difficulties (e.g., Sibley et al., 2012), and emerging work in adult ADHD has shown that collateral ratings of ADHD provide incremental value in the assessment of ADHD and other areas of functioning (Sibley et al., 2011). In addition, shared method variance due to our sole reliance on self-report may potentially inflate the magnitude of relations demonstrated in this study. Given the overlap between ADHD and other forms of psychopathology (e.g., inattention may be a symptom of ADHD and/or depression), we cannot rule out that the relations reported herein uniquely reflect ADHD effects. However, the significant associations that emerged between ADHD and internalizing symptoms and ADHD and drug use are of a similar magnitude in studies that have included more comprehensive evaluations of ADHD (Chronis-Tuscano et al., 2011; Lee et al., 2011; Seymour et al., 2012). Despite the limitations of self-report, the majority of young adult research is based on self-report and the measures used here have demonstrated adequate psychometric properties by self-report (Kessler et al., 2005; Adler et al., 2006). Our study focused on ADHD and CU as moderators of CP. However, it is also possible that other variables that we did not assess, including narcissism, are important to consider as moderators of CP in future work. The generalizability of findings may be limited because the sample was comprised primarily of college-attending students in a narrow age band. The majority of work in adults with CP/CU is based on forensic samples, and the level of CP, CU, and ADHD documented in our study may be less severe than what is documented in other samples. Also, our measures of functioning were collected from a broad based rating scale, and we do not have more nuanced assessments of impairment to contextualize results. Furthermore, analyses do not account for potential treatment effects, although existing research suggests that treatment utilization for externalizing problems in young adulthood is quite low (McCarthy et al., 2009).
In sum, our findings show that CU and ADHD are important considerations in understanding the effects of CP on impairment in young adulthood. Both CU and ADHD were important moderators for the relation between CP and young adult functioning, particularly tobacco use, family functioning, and internalizing symptoms. Replication of these findings is important, as very little research has focused on CP in young adults, despite the serious consequences of CP at this time in development. Our findings raise important questions to guide future research. In particular, our results highlight the need for continued work on CP, CU, and ADHD, which considers the interrelations of these overlapping, yet distinct factors, and examines their effects on adaptive functioning with a developmental lens.
Highlights.
This is one of the first studies to examine ADHD and CU as moderators of CP in young adults.
Effects of CP, ADHD and CU emerged in most areas except alcohol use.
ADHD×CP×CU effects emerged for family functioning, tobacco use, and internalizing symptoms.
Effects of ADHD, CU, or CP effects were not observed for reported alcohol use.
Future work must consider ADHD and CU as moderators on CP in young adults
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institutes of Health under BIRCWH award number 2 K12 HD055882, “Career Development Program in Women’s Health Research at Penn State” and by NIH NCATS TR000126.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Bernstein A, Dumenci L. DSM-oriented scales and statistically based syndromes for ages 18 to 59: linking taxonomic paradigms to facilitate multitaxonomic approaches. Journal of Personality Assessment. 2005;84:49–63. doi: 10.1207/s15327752jpa8401_10. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms and Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington, VT: 2003. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: 2013. [Google Scholar]
- Arnett JJ. Emerging adulthood: what is it, and what is it good for? Child Development Perspectives. 2007;1:68–73. [Google Scholar]
- Bartol FE, Miller CJ. Callous-unemotional traits in individuals receiving accommodations in university. Journal of Psychopathology and Behavioral Assessment. 2014;36:510–518. [Google Scholar]
- Bauer UE, Johnson TM, Hopkins RS, Brooks RG. Changes in youth cigarette use and intentions following implementation of a tobacco control program: findings from the Florida Youth Tobacco Survey, 1998–2000. J.A.M.A. 2000;294:723–728. doi: 10.1001/jama.284.6.723. [DOI] [PubMed] [Google Scholar]
- Byrd AL, Kahn RE, Pardini DA. A validation of the inventory of callous-unemotional traits in a community sample of young adult males. Journal of Psychopathology and Behavioral Assessment. 2013;35:20–34. doi: 10.1007/s10862-012-9315-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erhardt D, Epstein JN, Conners CK, Parker JDA, Sitarenios G. Self-ratings of ADHD symptoms in adults II: reliability, validity, and diagnostic sensitivity. Journal of Attention Disorders. 1999;3:153–158. [Google Scholar]
- Frick PJ. The inventory of callous-unemotional traits. The University of New Orleans; New Orleans, LA: 2004. [Google Scholar]
- Frick PJ, Ray JV, Thornton LC, Kahn RE. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychological Bulletin. 2014;140:1–57. doi: 10.1037/a0033076. [DOI] [PubMed] [Google Scholar]
- Ginsberg Y, Hirvikoski T, Lindefors N. Attention deficit hyperactivity disorder (ADHD) among longer-term prison inmates is a prevalent, persistent and disabling disorder. BMC Psychiatry. 2010;10:1–13. doi: 10.1186/1471-244X-10-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano PA, Ros R, Haas S, Hart K, Slavec J, Waschbusch DA, Garcia A. Assessing callous-unemotional traits in preschool children with disruptive behavior problems using peer reports. Journal of Clinical Child and Adolescent Psychology. 2016;45:201–214. doi: 10.1080/15374416.2014.971460. [DOI] [PubMed] [Google Scholar]
- Haas SM, Waschbusch DA. Callous-unemotional traits and their relevance to ADHD. The ADHD Report. 2012;20(3):5–9. [Google Scholar]
- Holtzman AL, Babinski D, Merlo LJ. Knowledge and attitudes toward hookah usage among university students. Journal of American College Health. 2013;61:362–370. doi: 10.1080/07448481.2013.818000. [DOI] [PubMed] [Google Scholar]
- Houghton S, West J, Tan C. The nature and prevalence of psychopathic tendencies among mainstream school children and adolescents: traditional and latent-trait approaches. In: Waugh RF, editor. Frontiers in Educational Psychology. Nova Science Publishers; Hauppague, NY: 2005. pp. 259–280. [Google Scholar]
- Johnston C, Chronis-Tuscano A. Families and ADHD. In: Barkley RA, editor. Attention-Deficit/Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. The Guilford Press; New York, NY: 2014. pp. 191–209. [Google Scholar]
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, Aucoin KJ, Morris AS. Assessing callous-unemotional traits in adolescent offenders: validation of the Inventory of Callous-Unemotional Traits. International Journal of Law and Psychiatry. 2008;31:241–252. doi: 10.1016/j.ijlp.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Kubak FA, Salekin RT. Psychopathy and anxiety in children and adolescents: new insights on developmental pathways to offending. Journal of Psychopathology and Behavioral Assessment. 2009;31:271–284. [Google Scholar]
- Kuriyan AB, Pelham WE, Molina BSG, Waschbusch DA, Gnagy EM, Sibley MH, Babinski DE, Walther C, Cheong J, Yu J, Kent KM. Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology. 2013;41:27–41. doi: 10.1007/s10802-012-9658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke J, Rathouz PJ, McBurnett K. Waxing and waning in concert: dynamic comorbidity of conduct disorder with other disruptive and emotional problems over 17 years among clinic-referred boys. Journal of Abnormal Psychology. 2002;111(4):556–567. doi: 10.1037//0021-843x.111.4.556. [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: A review of the past 10 years, part I. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(12):1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Loeber R, Stallings R. Modeling the impact of interventions on local indicators of offending, victimization, and incarceration. In: Loeber R, Farrington DP, editors. Young Homicide Offenders and Victims. Springer; New York, NY: 2011. pp. 137–152. [Google Scholar]
- McCarthy S, Asherson P, Coghill D, Hollis C, Murray M, Potts L, Sayal K, de Soysa R, Taylor E, Williams T, Wong ICK. Attention-deficit/hyperactivity disorder: treatment discontinuation in adolescents and young adults. The British Journal of Psychiatry. 2009;194:273–277. doi: 10.1192/bjp.bp.107.045245. [DOI] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: a meta-analytic review. Clinical Psychology Review. 2014;34:595–607. doi: 10.1016/j.cpr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Mohr-Jensen C, Steinhausen H. A meta-analysis and systematic review of the risks associated with childhood attention-deficit hyperactivity disorder on long-term outcome of arrests, convictions, and incarcerations. Clinical Psychology Review. 2016;48:32–42. doi: 10.1016/j.cpr.2016.05.002. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112:497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, Marshal MP. Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcoholism: Clinical and Experimental Research. 2007;31:643–654. doi: 10.1111/j.1530-0277.2007.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10:335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Salekin RT, Frick PJ. Psychopathy in children and adolescents: the need for a developmental perspective. Journal of Abnormal Child Psychology. 2005;33:403–409. doi: 10.1007/s10802-005-5722-2. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Gnagy EM, Waxmonsky JG, Waschbusch DA, Derefinko KJ, Wymbs BT, Garefino AC, Babinski DE, Kuriyan AB. When diagnosing ADHD in young adults emphasize informant reports, DSM items, and impairment. Journal of Consulting and Clinical Psychology. 2012;80:1052–1061. doi: 10.1037/a0029098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Coxe S, Kipp H, Gnagy EM, Meinzer M, Ross JM, Lahey BB. The role of early childhood ADHD and subsequent CD in the initiation and escalation of adolescent cigarette, alcohol, and marijuana use. Journal of Abnormal Psychology. 2014;123:362–374. doi: 10.1037/a0036585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BS, Gnagy EM, Waschbusch DA, Biswas A, McLean MG, Babinski DE, Karch KM. The delinquency outcomes of boys with ADHD with and without comorbidity. Journal of abnormal child psychology. 2011;39:21–32. doi: 10.1007/s10802-010-9443-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutfin EL, McCoy TP, Morrell HER, Hoeppner BB, Wolfson M. Electronic cigarette use by college students. Drug and Alcohol Dependence. 2013;131:214–221. doi: 10.1016/j.drugalcdep.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller R, Gardner F, Hyde LW. What are the associations between parenting, callous-unemotional traits, and antisocial behavior in youth? A systematic review of evidence. Clinical Psychology Review. 2013;33:598–608. doi: 10.1016/j.cpr.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128:118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Willoughby MT. Attention-deficit/hyperactivity disorder and callous-unemotional traits as moderators of conduct problems when examining impairment and aggression in elementary school children. Aggressive Behavior. 2008;34:139–153. doi: 10.1002/ab.20224. [DOI] [PubMed] [Google Scholar]