Fig. 1.
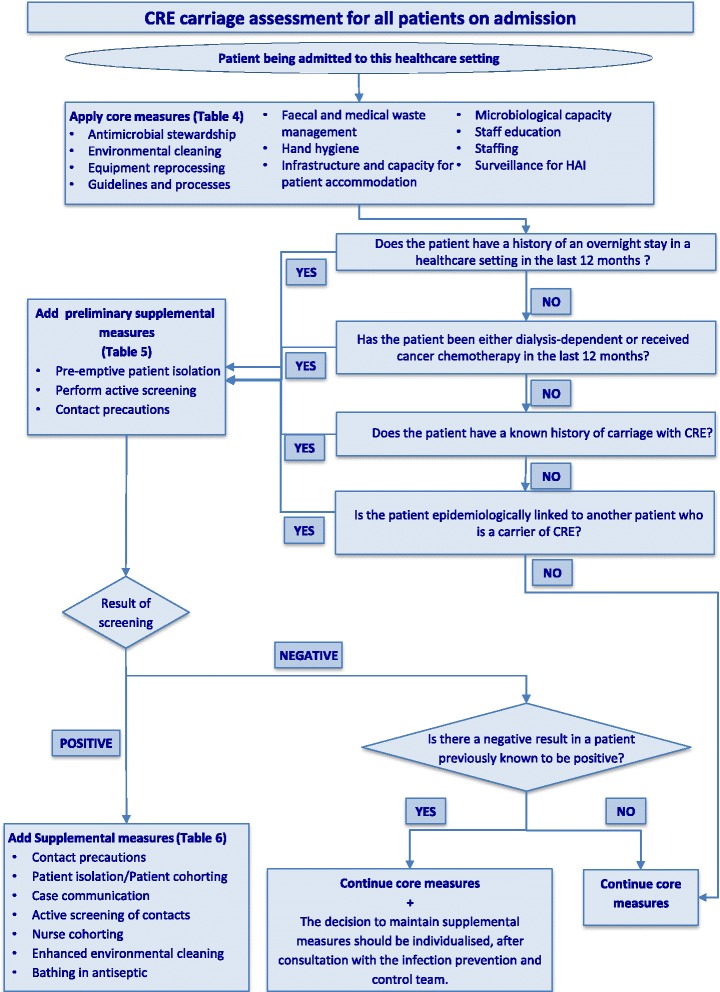
Flowchart for assessment of carriage of carbapenem-resistant Enterobacteriaceae in patients being admitted to healthcare settings.
Instructions for use of flowchart in Figure 1 for the management of “at-risk” patients being admitted to healthcare settings
This guidance document was created as a practical tool, for use by frontline HCWs and IPC and control professionals, for the evaluation and management of patients admitted to a healthcare setting. The goal is to identify the “at-risk” patients carrying CRE and to implement measures to prevent the transmission of these bacteria to other patients in the healthcare setting.
On admission to the healthcare setting, frontline HCWs should evaluate all patients to see whether they fall into any one of the four risk categories outlined in Table 3 and the flowchart in Fig. 1, and whether they have prior microbiological evidence for CRE carriage. See flowchart on how to manage patients who are potential carriers.
All admitted patients should have core measures applied regardless of their carrier status. These should be continued for the duration of their stay.
Any patient who is a potential carrier should have the following three preliminary supplemental measures implemented:
a) pre-emptive isolation in a single room while waiting for results of screening
b) active screening for CRE by obtaining swabs from rectal or perirectal areas and any other site that is either actively infected or considered to be colonised
c) contact precautions implemented and used by anyone entering the room.
If the result of the active screening is positive for CRE, the measures (patient isolation and contact precautions) are continued and additional supplemental measures are added. Timely communication of the latest microbiological results with the clinical and IPC teams is critical, the patient’s contacts should be screened for CRE carriage, enhanced environmental cleaning applied and consideration given to designated nurse cohorting, based on the clinical situation and location.
If the results of active screening are negative for CRE and there is no other indication to continue contact precautions (e.g., patient colonised with another MDRO or patient with a transmissible infection, such as C. difficile) contact precautions can be discontinued, but core measures should be continued.
For the patient with a previous positive result for CRE, but from whom CRE is not detected on readmission screening, the decision to continue supplemental measures should be based on a case-by-case risk assessment, in consultation with the IPC team. Factors to be taken into consideration include: the clinical area to which the patient is admitted (e.g., critical care, transplant, oncology), patient age, underlying comorbidity, invasive device use, skin breaks, incontinence, recent antimicrobial use, microbiological tests and schema used for assessing carriage, taking into account the possibility of a false negative screening test result, and interval since the last positive culture for CRE, among others
