Abstract
High-frequency ultrasonography (HFUS) is a common method to non-invasively monitor the real-time development of the human fetus in utero. The mouse is routinely used as an in vivo model to study embryo implantation and pregnancy progression. Unfortunately, such murine studies require pregnancy interruption to enable follow-up phenotypic analysis. To address this issue, we used three-dimensional (3-D) reconstruction of HFUS imaging data for early detection and characterization of murine embryo implantation sites and their individual developmental progression in utero. Combining HFUS imaging with 3-D reconstruction and modeling, we were able to accurately quantify embryo implantation site number as well as monitor developmental progression in pregnant C57BL6J/129S mice from 5.5 days post coitus (d.p.c.) through to 9.5 d.p.c. with the use of a transducer. Measurements included: number, location, and volume of implantation sites as well as inter-implantation site spacing; embryo viability was assessed by cardiac activity monitoring. In the immediate post-implantation period (5.5 to 8.5 d.p.c.), 3-D reconstruction of the gravid uterus in both mesh and solid overlay format enabled visual representation of the developing pregnancies within each uterine horn. As genetically engineered mice continue to be used to characterize female reproductive phenotypes derived from uterine dysfunction, this method offers a new approach to detect, quantify, and characterize early implantation events in vivo. This novel use of 3-D HFUS imaging demonstrates the ability to successfully detect, visualize, and characterize embryo-implantation sites during early murine pregnancy in a non-invasive manner. The technology offers a significant improvement over current methods, which rely on the interruption of pregnancies for gross tissue and histopathologic characterization. Here we use a video and text format to describe how to successfully perform ultrasounds of early murine pregnancy to generate reliable and reproducible data with reconstruction of the uterine form in mesh and solid 3-D images.
Keywords: Developmental Biology, Issue 128, Three dimensional, high frequency ultrasound, mouse, implantation, pregnancy
Introduction
Recurrent early pregnancy loss is one of the most common complications after conception and affects approximately 1% of couples trying to conceive1,2. The underlying mechanisms of early pregnancy loss are varied: from intrinsic embryonic abnormalities and maternal comorbidities to defects in endometrial receptivity1,3,4. Because of their genetic tractability, mouse models have been widely utilized for investigations of early embryo implantation and pregnancy. Furthermore, the short gestational time of the mouse and the ability to perform large-scale studies have ensured the growing utility of the mouse in addressing key clinical questions in human reproductive medicine5. That said, the vast majority of murine experimental designs still require numerous dams to be euthanized on sequential gestational days to quantify and analyze implantation site location, number, size, and spacing patterns during pregnancy6,7,8, thereby precluding longitudinal studies on the same animal.
In the clinic, ultrasound is a reliable and invaluable tool to monitor human fetal viability and development in a non-invasive manner9,10,11. More recently, high-frequency ultrasound (HFUS) has begun to find limited applications in the mouse as a method for monitoring fetal viability and growth during pregnancy12,13,14. The recent technological advances in ultrasound imaging have permitted the application of three-dimensional (3-D) data for visual reconstruction of animal organs and subsequent monitoring of pathologies15,16,17. Use of this advanced imaging technology has markedly improved the power to detect smaller volume fluctuations, to reduce inter-animal variability, and to monitor the progression of a pathology or the efficacy of a therapeutic intervention17. While the primary utility of this technology has been to monitor malignancy progression in oncomouse models15,16, 3-D HFUS imaging has only recently been used to quantitate and monitor the active growth of embryo implantation and fetal development in the mouse uterus18.
Here, we demonstrate how to perform HFUS imaging to produce 2-D and 3-D data to generate reconstructions of the early pregnant mouse uterus. We demonstrate the utility of this novel method to detect these early embryonic implantation events without the need for pregnancy termination, allowing researchers to collect data in a non-invasive manner.
Protocol
These studies were conducted in accordance with the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health and animal protocols approved by the Institutional Animal Care and Use Committee (IACUC) of Baylor College of Medicine under protocol number AN-4203.
1. Preparation of the Pregnant Mouse for Ultrasound
- Timed mating
- Place the dam with a proven fertile male mouse overnight beginning after 1700. Separate dam and male by 0700 hours (h), regardless if vaginal plug is present, to ensure accurate dating of pregnancy. NOTE: The morning after mating is considered 0.5 day post coitum (d.p.c.).
- Preparation for ultrasound
- Place the pregnant mouse in a sealed anesthesia induction container.
- Sedate with isoflurane (2%) inhaled anesthetic and oxygen (1 L/min) until the animal loses the righting reflex (approximately 1-2 min depending on the size of the mouse) and spontaneous movements are not observed (besides respiration).
- Place sedated mouse in supine position in nose cone with isoflurane (2%) inhaled anesthetic and oxygen (1 L/min). Apply ophthalmic ointment to the animal's eyes.
- With a cotton swab, apply depilatory cream to entire abdomen, sternum to vagina, and lateral to the flanks.
- Allow cream to remain for a maximum of 3 min, and then remove cream and hair with tissue. Ensure that all hair is removed, as any remaining hair will decrease image quality.
2. Preparation of the Ultrasound Stage
Turn on the transducer.
- Attach 3-D motor stage motor stage to the transducer.
- Plug into 3D motor by connecting the 3D motor cable to the 3D motor connector on the rear panel. Attach the 3D motor system to the mounting system using the quick release post on the top to connect to the imaging station, and the quick release mount on the bottom to affix the transducer clamp.
Attach the probe to the transducer clamp.
3. Begin Imaging the Pregnant Mouse
- Place mouse supine on the monitoring platform. The mouse continuously receives isoflurane anesthetic (between 1.5-2.5%) and oxygen (1 L/min) via the nose cone. Gently tape all paws to heart rate monitoring pads on the platform.
- Apply 1-2 mL of ultrasound transmission gel on abdomen.
- Using the manual motor stage, position the ultrasound probe on the lower abdomen.
- Locate the bladder, which should appear as a fluid-filled dark circle just cephalad to the vaginal opening.
- Once the bladder is located, move the probe very slowly cephalad to visualize the pregnant uterus, which should appear as a cylindrical shape with round areas at pregnancy sites. This can be described as looking like pearls on a chain.
- Once the pregnant uterus has been identified, begin 2-D imaging.
4. The 2-D Ultrasound Imaging (Figure 1)
Once the pregnant uterus has been identified, begin at the pregnancy site closest to the bladder and slowly and sequentially move cephalad to determine number and location of pregnancy sites.
If the kidney, spleen, or liver are visualized, reposition the probe closer caudal (closer to the bladder) as the user has gone too far cephalad.
Image the contralateral uterine horn in the same manner.
Freeze the image when the ultrasound frame is in the center of the implantation/pregnancy site to save for later analysis and measurements. NOTE: It takes less than one second for the image to be frozen and saved for later analysis.
Measure implantation distance using the hyperechoic decidualization reaction as a marker by manually clicking on the "measure" tool first, and then clicking on the location of one implantation site. Next, drag the cursor to next implantation site and click to draw a line that the computer will automatically report its distance. The software will then report what the manual measurement is. This step is not computerized, but relies on the user to mark the distance between decidualized sites by drawing a line between the decidualized sites, which the program will provide a measurement for.
Measure implantation size, gestational sac size, and fetal pole size.
5. Fetal Heart Rate
NOTE: At 9.5 d.p.c., the fetal heart beat should be clearly visualized.
While keeping the probe very still, turn on the pulse wave Doppler and position this over the visible heartbeat.
Record the cardiac heart beat pulsations. NOTE: Apart from the heart, this procedure can also record pulsations in the umbilical cord.
6. 3-D Ultrasound Acquisition
After the pregnant uterus has been visualized on 2-D imaging, position the probe in an area that is in the approximate mid-point of the desired 3-D image. For example, if one were imaging an apple in 3-D, the probe should initially be placed where the apple core is predicted to be located (i.e. middle of object).
With the probe in a position in the middle of the desired image, obtain a 3-D acquisition. The 3-D motor stage will travel this distance across the uterus in a series of steps or frames, with the intention of capturing in entirety what the investigator desires.
Confirm that the intended structures are completely captured in the 3-D scanning before completing the real-time ultrasound portion. Save this 3-D information for post-processing at a later time. The total time for 2-D and 3-D ultrasound acquisition is approximately 10-20 minutes when performed by an experienced user.
7. 3-D Reconstitution Post-processing (Figure 2)
Load the desired data for 3-D image processing.
- Choose "parallel and rotational methods", which will load all the 3D image frames into one 3-D "box" that the user will then trace the desired object in, frame-by-frame. Choose step size 0.08 mL. Begin at one end of the image block and scroll through to familiarize with the images that have been captured within space.
- Start at one end of the image and manually trace the outline of the object.
- Scroll to next 2-D image slice or "frame" and manually trace the outline of the object.
- Continue this process until all frames have been manually annotated/traced by the user.
- Click "finish" to obtain the 3-D image and total volume calculations.
Choose between mesh and solid overlay, which is an arrow in the top left corner.
Choose to keep or remove the surrounding ultrasound image information for clarity. Each 3-D reconstruction may take between 10 and 20 min.
8. Post-procedural Care
When the ultrasound is complete, turn off the anesthesia gas, remove the mouse from the platform and gently wipe and wash away any ultrasound gel from the animal.
Place the mouse back in the cage in a prone position in a padded area. Monitor until the animal is awake and moving spontaneously.
Representative Results
As demonstrated in Figure 1, the high frequency ultrasound can detect implantation site development beginning as early as the 5.5 d.p.c time point. Using the lighter hyperechoic decidualized endometrium as a marker of implantation sites at 6.5 d.p.c allows the number of implantation sites and spacing of these sites to be quantified. As the pregnancy progresses to 7.5 d.p.c., a darker hypoechoic gestational sac and fetal pole are also easily identifiable.

As shown in Figure 2, the completed post-processing composition of the three-dimensional reconstruction of the mouse uterus is able to be visualized. At 6.5 d.p.c, the 3-D high frequency ultrasound composition in both mesh and solid overlay formats can be used to provide a visual depiction. Another example, this time at 7.5 d.p.c, demonstrates the final composite image of another uterus with both mesh and solid overlay.
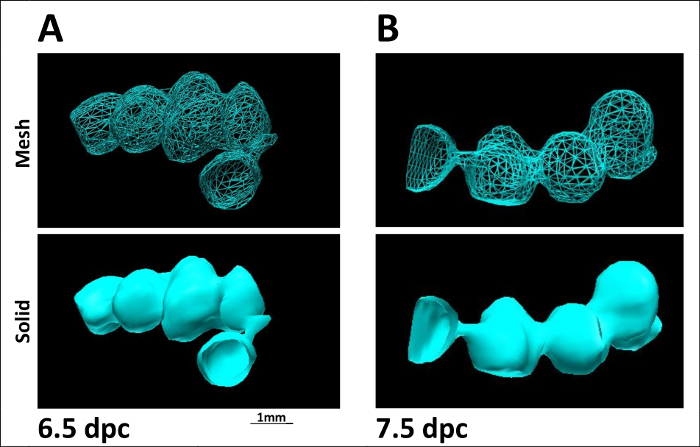
Figure 1: High Frequency Ultrasound detection of implantation site development and monitoring of fetal growth throughout gestation. As shown in Figure 1A, on 5.5 d.p.c. the lighter hyperechoic decidualized endometrium (D) allows the number of implantation sites and spacing to be quantified. As shown in Figure 1B, the decidualization sites (D) in another uterine horn are joined by the uterine horn (U). By 7.5 d.p.c., the darker hypoechoic sac (GS) and fetal pole (F) are easily identifiable Figure 1C. Please click here to view a larger version of this figure.
Figure 2: The three-dimensional reconstruction of the mouse uterus during early pregnancy. At 6.5 d.p.c, as shown in Figure 2A, 3-D high frequency ultrasound in both mesh and solid overlay formats are shown. At 7.5 d.p.c, as shown in Figure 2B, 3-D high frequency ultrasound images with both mesh and solid overlay formats are shown. Please click here to view a larger version of this figure.
Discussion
This novel use of 3-D HFUS imaging demonstrates the ability to successfully detect, visualize, and characterize embryo-implantation sites during early murine pregnancy in a non-invasive manner. The technology offers a significant improvement over current methods, which rely on the interruption of pregnancies for gross tissue and histopathologic characterization. However it should be noted that histological methods would still be considered more optimal when characterization at a more magnified and more cellular level is desired, or when gene and protein analysis is required. With a growing number of new mouse models displaying implantation defects and early pregnancy loss19,20,21,22, the ability of this advanced ultrasound technique to detect early pregnancies from 5.5 d.p.c onwards provides clear advantages over earlier ultrasound methods that were limited to detection at mid-pregnancy12,13. Moreover, this method detects cardiac motion as soon as the heart starts to beat, between 8.5-9.5 d.p.c23,24 allowing for confirmation of viable fetuses. The ability to follow early pregnancy events in the same animal means fewer animals are required per experiment and more accurate analysis can be performed with such longitudinal experimental designs25,26,27.
It should be noted that the three most critical steps in the protocol are: (1) knowing the exact gestational day; (2) the ability of the operator to locate the uterus and position the probe over the correct anatomical site; and (3) accurate techniques to produce a 3-D reconstruction. The following trouble shooting guidelines have proven helpful: When it is difficult to locate the uterus on ultrasound, the user can start by ensuring that the bladder is identified first. The bladder is usually seen as a black circle, and is immediately cephalad to the vaginal opening. Even in mice that have undergone micturition immediately prior to the ultrasound, the bladder is never completely empty and thus (in our experience) can be a reliable marker. Once the bladder is identified, the probe should be slowly moved cephalad until the uterus is seen. If the bladder is small or unable to be visualized, the user can also attempt to visualize the uterus by starting at the ovary, which can be found at the flanks, inferior to the kidney. Using this systematical approach, each implantation site and fetal development can be observed, as in Figure 1. On occasion, it may be difficult to obtain the desired region of the uterus during ultrasonography due to the manner in which the uterus is positioned in the abdomen, as shown in Figure 2 by different shapes and positions of the uterus in vivo. The user can tilt the mouse platform plane to shift or realign the uterus internally to a more favorable position in which the desired uterine region can be captured by ultrasound. Finally, the user can confirm that the desired uterine images were obtained during ultrasonography by quickly scrolling through the acquired ultrasound images soon after the ultrasound session is completed. A minor limitation is that the 3-D mesh/solid overlay for visual reconstruction cannot be performed during the ultrasound session. To ensure that the ultrasound images being obtained are accurate, we recommend that as the researchers are gaining proficiency, the animals are euthanized after ultrasound in order to correlate the accuracy of the ultrasound findings to gross tissue specimen measurements and anatomy.
While we describe here the modeling of normal murine pregnancy, future applications of this technique will be applied to quantify abnormal early pregnancy events. HFUS and 3-D reconstruction will permit investigators to detect and monitor the number, size and locations of pregnancies which are abnormal in growth and/or development. For example, non-invasive phenotypic characterization of abnormalities—i.e. defective endometrial decidualization, aberrant embryo implantation distribution, and inadequate trophoblastic invasion and growth—displayed by an increasing number of genetically engineered mice can now be longitudinally analyzed without pregnancy interruption using this imaging methodology.
Disclosures
The authors have nothing to disclose.
Acknowledgments
We very much appreciate the assistance of Rong Zhao, Jie Li, and Yan Ying.
References
- Rai R, Regan L. Recurrent miscarriage. Lancet. 2006;368(9535):601–611. doi: 10.1016/S0140-6736(06)69204-0. [DOI] [PubMed] [Google Scholar]
- Sugiura-Ogasawara M, Ozaki Y, Suzumori N. Management of recurrent miscarriage. J Obstet Gynaecol Res. 2014;40(5):1174–1179. doi: 10.1111/jog.12388. [DOI] [PubMed] [Google Scholar]
- Kutteh WH. Novel strategies for the management of recurrent pregnancy loss. Semin Reprod Med. 2015;33(3):161–168. doi: 10.1055/s-0035-1552586. [DOI] [PubMed] [Google Scholar]
- Page JM, Silver RM. Genetic Causes of Recurrent Pregnancy Loss. Clin Obstet Gynecol. 2016;59(3):498–508. doi: 10.1097/GRF.0000000000000217. [DOI] [PubMed] [Google Scholar]
- Zhang J, Croy BA. Using ultrasonography to define fetal-maternal relationships: moving from humans to mice. Comp Med. 2009;59(6):527–533. [PMC free article] [PubMed] [Google Scholar]
- Li SJ, et al. Differential regulation of receptivity in two uterine horns of a recipient mouse following asynchronous embryo transfer. Sci Rep. 2015;5:15897. doi: 10.1038/srep15897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding YB, et al. 5-aza-2'-deoxycytidine leads to reduced embryo implantation and reduced expression of DNA methyltransferases and essential endometrial genes. PLoS One. 2012;7(9):e45364. doi: 10.1371/journal.pone.0045364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusakabe K, Naka M, Ito Y, Eid N, Otsuki Y. Regulation of natural-killer cell cytotoxicity and enhancement of complement factors in the spontaneously aborted mouse placenta. Fertil Steril. 2008;90(4 Suppl):1451–1459. doi: 10.1016/j.fertnstert.2007.07.1331. [DOI] [PubMed] [Google Scholar]
- Demianczuk NN, et al. The use of first trimester ultrasound. J Obstet Gynaecol Can. 2003;25(10):864–875. doi: 10.1016/s1701-2163(16)30680-6. [DOI] [PubMed] [Google Scholar]
- Thompson HE. Evaluation of the obstetric and gynecologic patient by the use of diagnostic ultrasound. Clin Obstet Gynecol. 1974;17(4):1–25. doi: 10.1097/00003081-197412000-00001. [DOI] [PubMed] [Google Scholar]
- Unterscheider J, et al. Definition and management of fetal growth restriction: a survey of contemporary attitudes. Eur J Obstet Gynecol Reprod Biol. 2014;174:41–45. doi: 10.1016/j.ejogrb.2013.11.022. [DOI] [PubMed] [Google Scholar]
- Greco A, et al. High frequency ultrasound for in vivo pregnancy diagnosis and staging of placental and fetal development in mice. PLoS One. 2013;8(10):e77205. doi: 10.1371/journal.pone.0077205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores LE, Hildebrandt TB, Kuhl AA, Drews B. Early detection and staging of spontaneous embryo resorption by ultrasound biomicroscopy in murine pregnancy. Reprod Biol Endocrinol. 2014;12:38. doi: 10.1186/1477-7827-12-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TM, et al. Estimation of mouse fetal weight by ultrasonography: application from clinic to laboratory. Lab Anim. 2012;46(3):225–230. doi: 10.1258/la.2012.011117. [DOI] [PubMed] [Google Scholar]
- Singh S, et al. Quantitative volumetric imaging of normal, neoplastic and hyperplastic mouse prostate using ultrasound. BMC Urol. 2015;15:97. doi: 10.1186/s12894-015-0091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, et al. Ultrasound-mediated destruction of paclitaxel and oxygen loaded lipid microbubbles for combination therapy in ovarian cancer xenografts. Cancer Lett. 2015;361(1):147–154. doi: 10.1016/j.canlet.2015.02.052. [DOI] [PubMed] [Google Scholar]
- Ni J, et al. Monitoring Prostate Tumor Growth in an Orthotopic Mouse Model Using Three-Dimensional Ultrasound Imaging Technique. Transl Oncol. 2016;9(1):41–45. doi: 10.1016/j.tranon.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peavey MC, et al. Three-Dimensional High-Frequency Ultrasonography for Early Detection and Characterization of Embryo Implantation Site Development in the Mouse. PLoS One. 2017;12(1):e0169312. doi: 10.1371/journal.pone.0169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H, et al. Cytosolic phospholipase A2alpha is crucial [correction of A2alpha deficiency is crucial] for 'on-time' embryo implantation that directs subsequent development. Development. 2002;129(12):2879–2889. doi: 10.1242/dev.129.12.2879. [DOI] [PubMed] [Google Scholar]
- Nallasamy S, Li Q, Bagchi MK, Bagchi IC. Msx homeobox genes critically regulate embryo implantation by controlling paracrine signaling between uterine stroma and epithelium. PLoS Genet. 2012;8(2):e1002500. doi: 10.1371/journal.pgen.1002500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirate Y, et al. Mouse Sox17 haploinsufficiency leads to female subfertility due to impaired implantation. Sci Rep. 2016;6:24171. doi: 10.1038/srep24171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TS, et al. Dysregulated LIF-STAT3 pathway is responsible for impaired embryo implantation in a Streptozotocin-induced diabetic mouse model. Biol Open. 2015;4(7):893–902. doi: 10.1242/bio.011890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji RP, et al. Onset of cardiac function during early mouse embryogenesis coincides with entry of primitive erythroblasts into the embryo proper. Circ Res. 2003;92(2):133–135. doi: 10.1161/01.res.0000056532.18710.c0. [DOI] [PubMed] [Google Scholar]
- Srinivasan S, et al. Noninvasive, in utero imaging of mouse embryonic heart development with 40-MHz echocardiography. Circulation. 1998;98(9):912–918. doi: 10.1161/01.cir.98.9.912. [DOI] [PubMed] [Google Scholar]
- Franco NH, Olsson IA. Scientists and the 3Rs: attitudes to animal use in biomedical research and the effect of mandatory training in laboratory animal science. Lab Anim. 2014;48(1):50–60. doi: 10.1177/0023677213498717. [DOI] [PubMed] [Google Scholar]
- Pratap K, Singh VP. A training course on laboratory animal science: an initiative to implement the Three Rs of animal research in India. Altern Lab Anim. 2016;44(1):21–41. doi: 10.1177/026119291604400109. [DOI] [PubMed] [Google Scholar]
- Landi MS, Shriver AJ, Mueller A. Consideration and checkboxes: incorporating ethics and science into the 3Rs. J Am Assoc Lab Anim Sci. 2015;54(2):224–230. [PMC free article] [PubMed] [Google Scholar]


