Abstract
Introduction
Respiratory syncytial virus (RSV) is the leading cause of hospitalization among infants in the United States, and the risk for RSV hospitalizations is greater for infants born preterm. Recent studies in preterm and term infants have shown that RSV hospitalization rates vary considerably depending on infant chronologic age. This study sought to aggregate the data available from published literature and from nationally representative databases of US infant hospitalizations to generate a composite description of the effect of young chronologic age on RSV hospitalizations among US preterm and term infants by individual month of age.
Methods
Data describing the relative incidence of RSV hospitalizations by individual month of chronologic age during the first year of life were obtained from recently published studies, the 2006–2011 National Inpatient Sample databases, and the 2006 and 2009 Kids Inpatient Databases.
Results
All data sources showed that ≥20% of infant RSV hospitalizations occurred in the second month of life and >50% and >75% of RSV hospitalizations were observed during the first 3 and 6 months of life, respectively. These findings were consistent for both preterm and term infants.
Conclusion
Data from multiple sources demonstrate that the greatest risk of RSV hospitalization occurs during the first 6 months of life among US preterm and term infants. Strategies to prevent infant RSV hospitalizations should be targeted to infants during the first months of life.
Funding
AstraZeneca.
Keywords: Infant, Hospitalization, Preterm, Respiratory syncytial virus, RSV
Introduction
Respiratory syncytial virus (RSV) is the most common cause of bronchiolitis and pneumonia in infants and is the leading cause of hospitalization among infants [1–3], responsible for nearly 16 times more infant hospitalizations than influenza [1]. However, RSV hospitalization rates in the United States are highest for infants aged <1 year, with rates estimated at 2345 per 100,000 person-years compared with 178 per 100,000 person-years for 1- to 4-year-old children and even lower rates for children aged ≥5 years [1].
The risk for RSV hospitalization is greater for infants born preterm, or with chronic lung disease, congenital heart disease, or other comorbid conditions, and can be further increased by factors such as being born during the RSV season, attending daycare, and/or having preschool-aged siblings [4–12]. A multicenter prospective surveillance study demonstrated that the greatest risk of RSV hospitalization for US infants occurs during the second month of life [13]. Similarly, a recent systematic literature review conducted among healthy preterm infants born at 29–35 weeks gestational age (wGA) concluded that preterm infants were at elevated risk of RSV hospitalization relative to term infants and that young chronologic age during the RSV season was one of the most important risk factors for RSV hospitalization in this population [14].
This study sought to aggregate the data available from published literature and from nationally representative databases of US infant hospitalizations to generate a composite description of the effect of chronologic age by individual month on RSV hospitalizations among US term and preterm infants.
Methods
Data Sources
This article is based on previously available data, and does not involve any new studies of human or animal subjects performed by any of the authors. We included studies published between 2012 and 2017 that were conducted in the US, evaluated RSV hospitalization proportions using data after the year 2000, and provided data by age in months (e.g., <1, 1 to <2, 11 to <12 months). This strategy resulted in the inclusion of data from 3 studies in the analysis: Hall et al. [15], Helfrich et al. [16], and Anderson et al. [17]. These studies represent the relative incidence of RSV hospitalizations among preterm and term infants as a function of chronologic age in individual months. No data were available regarding the incidence of RSV hospitalization by individual month of age among children with chronic medical conditions. Specific details of the published studies included in this analysis are listed in Table 1.
Table 1.
Details of infants included in previously published studies
| Study | Characteristics of infants included and study | |||
|---|---|---|---|---|
| Author/year | Age criteria | Specific inclusion criteria | Data source/location | Study period |
| Hall et al. (2013) [12] | All children aged <24 months | Hospitalized for laboratory-confirmed RSV infection | New Vaccine Surveillance Network from Nashville, TN, Rochester, NY, and Cincinnati, OH | October 1, 2000 to March 31, 2001; October 1, 2001 to March 31, 2002; October 1, 2002 to March 31, 2003; October 1, 2003 to March 31, 2004; October 1, 2004 to March 31, 2005 |
| Helfrich et al. (2015) [13] | Non-high-risk infants 33–36 wGA and term infants | No receipt of palivizumab | Military Health System | October 1, 2005 to April 30, 2011 |
| Anderson et al. (2017) [14] | 29–35 wGA | No RSV immunoprophylaxis received and hospitalized for laboratory-confirmed RSV infection | Data from 43 diverse US practices | October 1, 2014 to April 30, 2015 |
RSV respiratory syncytial virus, wGA weeks gestational age
Data Analysis
All analyses for this study were restricted to infants (i.e., children aged 0–12 months). Data from published studies and the National Inpatient Sample (NIS) and Kids Inpatient Database (KID) were analyzed to compute proportions of RSV hospitalizations by month of age relative to the total number of RSV hospitalizations during the first year of life [18, 19]. Data on the number of RSV hospitalizations by age in months from Hall et al. were obtained from table 2 of that study (n = 462) [15], and proportions by age in months were calculated. The number of hospitalizations by age in months were also calculated from fig. 2 of the Helfrich et al. [16] study. Proportions were calculated separately for infants 33–34 wGA at birth, 35–36 wGA at birth, and term infants. Data on 702 community-acquired RSV hospitalizations from Anderson et al. [17] were obtained from the authors. The proportion of hospitalizations for each month of age were calculated for all 702 hospitalizations as well as in strata of gestational age at birth [i.e., 29–32 wGA (n = 237), 33–34 wGA (n = 283), and 35 wGA (n = 182)].
To complement data from the published studies, an analysis of the NIS and KID data was performed. The NIS and KID are US-based, nationally representative de-identified datasets developed and maintained by the Healthcare Cost and Utilization Project, sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest dataset currently available that provides national estimates for all inpatient stays (i.e., includes children, adults, and the elderly), whereas the KID provides national estimates specifically for pediatric (age ≤20 years) inpatient stays. Information to calculate age in months (i.e., “age in days” variable) for hospitalized infants has not been collected since 2012 in these databases (age only reported in years from 2012); therefore, the 2006–2011 NIS and the 2006 and 2009 KID databases were analyzed. Infant RSV hospitalizations in the NIS and KID data (after excluding birth hospitalizations) were identified using primary or secondary diagnoses of RSV (i.e., International Classification of Diseases, Ninth Revision, Clinical Modification codes 480.1, 466.11, 079.6).
Certain states were excluded because “age in days” was not reported (Florida, Massachusetts, Maine, New Hampshire, South Carolina, and Texas in the NIS data, and hospitalizations from Connecticut, Florida, Massachusetts, Maine, New Hampshire, South Carolina, and Texas in the KID data). To provide a national estimate of RSV hospitalization by age in months, weights were rescaled. Rescaling was conducted by summing the weights within each sampling stratum (with all states included) and then calculating the number of hospitalizations remaining within each sampling stratum after removing the states with no “age in days” variable. Subsequently, rescaled weights for each stratum were obtained by dividing the sum of weights by the number of remaining hospitalizations. After excluding states without “age in days,” all strata had more than one hospital and thereby no collapsing of strata was required. To compare NIS data with KID data, an additional analysis using only 2006 and 2009 NIS data was conducted. All analyses were performed using SAS statistical software, v.9.4 (SAS Institute, Cary, NC, USA).
Results
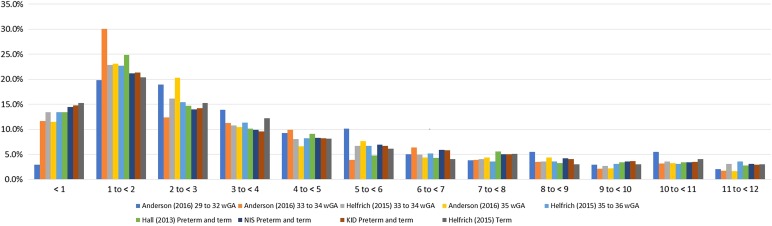
Overall data from all the included published studies and the analyses of NIS and KID data showed that nearly 50% of all RSV hospitalizations during the first year of life happened during the first 3 months of life, and 75–80% happened during the first 6 months of life (Fig. 1).
Fig. 1.
Proportion of infant RSV hospitalizations by age in months, across various data sources. RSV hospitalization proportions sums to 100%. RSV respiratory syncytial virus
Data on preterm and term infants combined from the Hall et al. [15] study showed that 13.4% (n = 62) of hospitalizations were observed for infants aged 0 to <1 month old, 24.9% (n = 115) for infants aged 1 to <2 months, and 14.7% (n = 68) for infants aged 2 to <3 months old. The Helfrich et al. [16] data showed that, among term infants, the greatest number of RSV hospitalizations [20.4% (n = 1147)] was also observed when the infants were in the second month of life. Among preterm infants born at 33–34 and 35–36 wGA in the Helfrich study, the greatest number of RSV hospitalizations was similarly observed during the second month of life [22.9% (n = 30) and 22.7% (n = 88), respectively] (see Fig. 1).
Using the data from Anderson et al. [14], one-quarter [25% (n = 174)] of all RSV hospitalizations among infants born at 29 to 35 wGA occurred during the second month of life (i.e., age 1 to <2 months), versus 9% (n = 61) and 17% (117) in the first and third months, respectively. The proportion of hospitalizations by wGA at birth is shown in Fig. 1. For infants born at 33–34 wGA, 12% (n = 33), 30% (n = 85), and 12% (n = 35) of RSV hospitalizations were observed during each of the first 3 months of life, respectively; for infants born at 35 wGA, the proportions were 12% (n = 21), 23% (n = 42), and 20% (n = 37), respectively. Among infants born at 29–32 wGA, the proportion during the first month of life was much lower, while the proportion of RSV hospitalizations during each of the first 3 months of life were 3% (n = 7), 20% (n = 47), and 19% (n = 45), respectively.
Characteristics of preterm and term infants with RSV hospitalization in the NIS and KID data are shown in Table 2. Across all RSV hospitalizations included in the NIS data from 2006 through 2011 (n = 361,685), 14.5% (n = 52,310) of RSV hospitalizations occurred when the infant was aged <1 month, 21.2% (n = 76,545) when aged 1 to <2 months, and 14.0% (n = 50,606) when aged 2 to <3 months (Table 3). Restricting data to only RSV hospitalizations during the RSV season (November–March) also showed that the highest proportion of hospitalizations was observed during the infant’s second month of life, and the proportions ranged from 20.4% (n = 11,969; November 2009 to March 2010) to 21.8% (n = 12,858; November 2007 to March 2008). Likewise, of all infant RSV hospitalizations in the 2006 and 2009 KID data (n = 136,344), 14.8% (n = 20,119) of RSV hospitalizations occurred when the infant was <1 month old, 21.3% (n = 29,067) when the infant was 1 to <2 months old, and 14.3% (n = 19,444) when the infant was 2 to <3 months old. Additional analyses restricting the NIS data to 2006 and 2009 found results similar to KID data, with 14.7% (n = 17,758) of all hospitalizations observed among those aged <1 month, 20.9% (n = 25,139) among those aged 1 to <2 months, and 14.0% (n = 16,878) among those aged 2 to <3 months old.
Table 2.
Characteristics of infants hospitalized for RSV in the National Inpatient Sample and Kids Inpatient Database
| NIS | KID | |||
|---|---|---|---|---|
| Weighted n a | % | Weighted n b | % | |
| Total | 361,685 | 100.0 | 136,344 | 100.0 |
| Sex | ||||
| Male | 206,214 | 57.0 | 77,114 | 56.6 |
| Female | 155,428 | 43.0 | 59,215 | 43.4 |
| Missing | 43 | 0.0 | 14 | 0.0 |
| Race/ethnicity | ||||
| White, non-Hispanic | 146,803 | 40.6 | 52,572 | 38.6 |
| Black, non-Hispanic | 39,806 | 11.0 | 14,886 | 10.9 |
| Native American | 3773 | 1.0 | 1167 | 0.9 |
| Hispanic | 60,732 | 16.8 | 23,506 | 17.2 |
| Asian | 6336 | 1.8 | 2178 | 1.6 |
| Other | 16,776 | 4.6 | 6053 | 4.4 |
| Unknown/missing | 87,457 | 24.2 | 35,981 | 26.4 |
| Payer type | ||||
| Private | 126,568 | 35.0 | 46,661 | 34.2 |
| Public | 211,939 | 58.6 | 81,333 | 59.7 |
| Self-pay | 11,426 | 3.2 | 4175 | 3.1 |
| Other | 10,779 | 3.0 | 3819 | 2.8 |
| No charge/unknown | 973 | 0.3 | 356 | 0.3 |
| Hospital/site region | ||||
| Northeast | 63,270 | 17.5 | 22,883 | 16.8 |
| Midwest | 84,040 | 23.2 | 35,774 | 26.2 |
| South | 130,880 | 36.2 | 43,966 | 32.2 |
| West | 83,494 | 23.1 | 33,721 | 24.7 |
| Household incomec | ||||
| 1st quartile | 119,605 | 33.1 | 46,983 | 34.5 |
| 2nd quartile | 95,435 | 26.4 | 36,373 | 26.7 |
| 3rd quartile | 76,469 | 21.1 | 28,750 | 21.1 |
| 4th quartile | 61,275 | 16.9 | 20,617 | 15.1 |
| Missing | 8902 | 2.5 | 3621 | 2.7 |
KID Kid Inpatient Database, NIS National Inpatient Sample, RSV respiratory syncytial virus
aAfter excluding the states (Florida, Massachusetts, Maine, New Hampshire, South Carolina, and Texas) with missing “age in days” variable, discharge weights were rescaled to match the national estimate of discharges
bAfter excluding the states (Connecticut, Florida, Massachusetts, Maine, New Hampshire, South Carolina, and Texas) with missing “age in days” variable, discharge weights were rescaled to match the national estimate of discharges
cQuartile ranges change by year for NIS and KID (http://www.hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp). For Anderson et al. [17]: quartile 1 = $1–39,999; quartile 2 = $40,000–50,999; quartile 3 = $51,000–65,999; quartile 4 = $66,000+
Table 3.
Proportion of RSV hospitalizations by age in months in the National Inpatient Sample Databasea, overall and by RSV season from 2006 through 2011, and the Kids Inpatient Database in 2006 and 2009
| Age in months | NIS | KID | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Across all years (n = 361,685) | November 2006–March 2007 (n = 58,958) | November 2007–March 2008 (n = 58,872) | November 2008–March 2009 (n = 50,893) | November 2009–March 2010 (n = 58,560) | November 2010–March 2011 (n = 52,265) | 2006 and 2009 (n = 136,344) | ||||||||
| Weighted n | % (95% CI) | Weighted n | % (95% CI) | Weighted n | % (95% CI) | Weighted n | % (95% CI) | Weighted n | % (95% CI) | Weighted n | % (95% CI) | Weighted n | % (95% CI) | |
| <1 | 52,310 | 14.5% (13.9–15.0) | 8543 | 14.5% (13.5–15.5) | 8464 | 14.4% (13.5–15.3) | 7648 | 15.0% (13.7–16.3) | 8220 | 14% (13.0–15.1) | 7089 | 13.6% (12.5–14.6) | 20,119 | 14.8% (14.3–15.3) |
| 1 to <2 | 76,545 | 21.2% (20.6–21.7) | 12,357 | 21.0% (19.9–22.0) | 12,858 | 21.8% (20.7–23.0) | 10,431 | 20.5% (19.5–21.5) | 11,969 | 20.4% (19.5–21.4) | 11,369 | 21.8% (20.2–23.3) | 29,067 | 21.3% (20.9–21.8) |
| 2 to <3 | 50,606 | 14.0% (13.7–14.3) | 8315 | 14.1% (13.4–14.8) | 8311 | 14.1% (13.3–14.9) | 6947 | 13.6% (12.9–14.4) | 8120 | 13.9% (13.1–14.7) | 7317 | 14% (13.3–14.7) | 19,444 | 14.3% (13.9–14.6) |
| 3 to <4 | 35,934 | 9.9% (9.7–10.2) | 6076 | 10.3% (9.7–10.9) | 5921 | 10.1% (9.5–10.7) | 5065 | 10% (9.2–10.7) | 5636 | 9.6% (9.1–10.2) | 5436 | 10.4% (9.6–11.2) | 13,110 | 9.6% (9.4–9.9) |
| 4 to <5 | 30,123 | 8.3% (8.1–8.6) | 5332 | 9.0% (8.4–9.7) | 4876 | 8.3% (7.6–9.0) | 4273 | 8.4% (7.7–9.1) | 4561 | 7.8% (7.3–8.3) | 4207 | 8.1% (7.4–8.7) | 11,176 | 8.2% (8.0–8.4) |
| 5 to <6 | 25,036 | 6.9% (6.7–7.2) | 4051 | 6.9% (6.2–7.5) | 4062 | 6.9% (6.3–7.5) | 3464 | 6.8% (6.1–7.5) | 4323 | 7.4% (6.8–8.0) | 3664 | 7.0% (6.3–7.7) | 9145 | 6.7% (6.5–6.9) |
| 6 to <7 | 21,280 | 5.9% (5.6–6.1) | 3282 | 5.6% (5.0–6.1) | 3318 | 5.6% (5.1–6.2) | 3147 | 6.2% (5.6–6.8) | 3503 | 6.0% (5.5–6.4) | 3058 | 5.9% (5.3–6.4) | 7991 | 5.9% (5.7–6.1) |
| 7 to <8 | 18,068 | 5.0% (4.8–5.2) | 3098 | 5.3% (4.8–5.7) | 2851 | 4.8% (4.4–5.3) | 2486 | 4.9% (4.4–5.3) | 3057 | 5.2% (4.8–5.6) | 2376 | 4.5% (4.1–5.0) | 6866 | 5.0% (4.8–5.2) |
| 8 to <9 | 15,171 | 4.2% (4.0–4.4) | 2163 | 3.7% (3.3–4.1) | 2535 | 4.3% (3.8–4.8) | 2121 | 4.2% (3.7–4.7) | 2679 | 4.6% (4.2–5.0) | 2253 | 4.3% (3.8–4.8) | 5583 | 4.1% (3.9–4.3) |
| 9 to <10 | 13,063 | 3.6% (3.4–3.8) | 2101 | 3.6% (3.2–4.0) | 2081 | 3.5% (3.1–4.0) | 1894 | 3.7% (3.3–4.1) | 2152 | 3.7% (3.3–4.1) | 1827 | 3.5% (3.0–3.9) | 5024 | 3.7% (3.5–3.9) |
| 10 to <11 | 12,297 | 3.4% (3.2–3.6) | 1888 | 3.2% (2.8–3.6) | 1880 | 3.2% (2.8–3.6) | 1742 | 3.4% (3.0–3.9) | 2258 | 3.9% (3.5–4.3) | 1901 | 3.6% (3.2–4.1) | 4775 | 3.5% (3.3–3.7) |
| 11–12 | 11,252 | 3.1% (3.0–3.3) | 1751 | 3.0% (2.6–3.3) | 1715 | 2.9% (2.5–3.3) | 1676 | 3.3% (2.9–3.7) | 2082 | 3.6% (3.2–3.9) | 1768 | 3.4% (3.0–3.8) | 4044 | 3.0% (2.8–3.1) |
CI confidence interval, KID Kids Inpatient Database, NIS National Inpatient Sample, RSV respiratory syncytial virus, wGA weeks gestational age
aAfter excluding the states (Florida, Massachusetts, Maine, New Hampshire, South Carolina, and Texas) with missing “age in days” variable, discharge weights were rescaled to match the national estimate of discharges
Discussion
The overall burden of RSV hospitalizations among infants is high, as the weighted results from the NIS and KID analyses estimated an average of more than 60,000 RSV-related hospitalizations each year during the first year of life, excluding birth hospitalizations. Moreover, all data sources showed that the peak age for RSV hospitalization was during the second month of life, with 20–30% of all RSV hospitalizations in the first year of life occurring during the second month of life. Also, consistent across all data sources, 50% of all infant RSV hospitalizations were observed in the first 3 months of life and more than 75% in the first 6 months of life. These results demonstrate that the risk of RSV hospitalization is greatest during the first 6 months of an infant’s life, and the risk declines with older chronologic age.
In our study, we showed that the peak incidence of hospitalization occurred in the second month for both preterm and term infants. However, this similar pattern may be driven by different mechanisms in preterm and term infants. In both, physiologic risk related to an infant’s small airways is greatest when infants are young; however, the greatest risk occurs at the second month of life rather than the first month. Chu et al. [20], based on a randomized control trial, and Glenzen et al. [21], based on a prospective cohort study, found that, in term infants, placentally-transferred maternal antibodies against RSV reduce incidence in the initial months of life, with the greatest effect in the first month of life. In contrast, preterm infants, particularly those <32 wGA, have less maternal antibody transfer before birth. However, as observed by La Gamma and colleagues [22] in a retrospective cohort study, these infants are frequently not discharged from the hospital for several weeks following birth, delaying exposure and the resulting peak incidence of RSV-related hospitalization. This is most evident in the Anderson et al. data for 29–31 wGA infants, in whom the relative incidence in the first month of life was much lower than that observed with all other populations studied [17].
In addition to the studies included in this analysis, other studies have highlighted the importance of chronologic age for RSV-associated hospitalizations in the United States. Using Florida and Texas Medicaid data for preterm (32–34 wGA) and term (37–41 wGA) infants, and using a different outcome measure (i.e., rate per 100 patient-years) for each month of age, Winterstein and colleagues [23] found that the rate per 100 patient-years for both states was greatest among infants aged 1 to <2 months. RSV hospitalization rates in the third month of life were 21–29% lower than rates in the second month. The Winterstein study did not examine rates in the first month of life.
Dougherty and Meissner [24], using data from 1994 to 1997 from a pediatric hospital, found that the greatest number of infants were admitted for RSV during the second and third months of life. Studies by Boyce et al. [25] and Fryzek et al. [26] did not present RSV hospitalizations by each month of chronologic age, but RSV hospitalizations were reported to be greatest among infants aged <3 months. A prospective study by Ambrose and coauthors observed that the risk of RSV hospitalization for infants 32–35 wGA was highest for infants in the first 6 months of life [4]. In a study by Simoes and colleagues published after our analysis was completed, it was demonstrated that RSV hospitalization was highest at young chronologic age and declined steadily with each additional month of age, similar to the results observed in the current analysis [27].
The findings presented here should be viewed in the context of certain methodological limitations. In Helfrich et al. [16], the number of infants (denominator in the proportions of hospitalizations per month of age) was not provided in the text and was therefore extracted from the figures, potentially leading to minor inaccuracies in the calculated proportions. RSV-related hospitalizations in the NIS and KID data were identified using diagnosis codes; as a result, coding inaccuracies may underestimate or overestimate the true prevalence of RSV hospitalizations. In the NIS and KID data, RSV hospitalizations from states for which the “age in days” variable was missing were excluded, and, although sampling weights were rescaled to report a national estimate (following recommendations from the data custodians), it may not accurately represent the age distribution of RSV hospitalizations in the missing states. In addition, because KID data were only available in 3-year intervals (e.g., 2003, 2006, 2009) rather than annually, hospitalizations during complete RSV seasons (November–March) could not be studied. Finally, the results of the present analyses are only generalizable to term and preterm infants without other underlying medical conditions. The results are not applicable to infants with chronic lung disease, congenital heart disease, or other underlying medical conditions that place children at significantly elevated risk of severe RSV disease, as no specific data were available for these populations.
Conclusion
Overall, in this study, data from various sources and diverse regions of the USA showed that a considerable number of preterm and term infants are hospitalized each year with RSV infection and that the risk of being hospitalized due to RSV is greatest during the first 6 months of life. As a result, strategies to prevent RSV hospitalization among infants in the United States should be targeted to the first months of life.
Acknowledgements
Funding for this study and the article processing charges was provided by AstraZeneca, Gaithersburg, MD, USA. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. The authors acknowledge Kelsey Tsipis of RTI Health Solutions for medical writing support. Editorial support in the preparation of this manuscript was provided by Rebecca McCracken, MSPH, CMPP, of The Lockwood Group, which was in accordance with Good Publication Practice (GPP3) guidelines and funded by AstraZeneca. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval to the version to be published.
Disclosures
Kimmie McLaurin is an employee of AstraZeneca. Christopher S. Ambrose is an employee of AstraZeneca. Melissa Pavilack is an employee of AstraZeneca. Rohan C. Parikh is an employee of RTI Health Solutions. Andrea V. Margulis is an employee of RTI Health Solutions. Josephine Mauskopf is an employee of RTI Health Solutions. Sean D. Candrilli is an employee of RTI Health Solutions.
Compliance with Ethics Guidelines
This article is based on previously available data, and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
The datasets analyzed during the current study are available from published literature (Hall et al. [15] and Helfrich et al. [16]), from the authors of the Anderson et al. study [17], or from the National Inpatient Sample database (https://www.hcup-us.ahrq.gov/nisoverview.jsp) and the Kids’ Inpatient Database (https://www.hcup-us.ahrq.gov/kidoverview.jsp), which have been developed and maintained by the Healthcare Cost and Utilization Project and are sponsored by the Agency for Healthcare Research and Quality, US Department of Health and Human Services.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/21FBF0605446F8F2.
References
- 1.Zhou H, Thompson WW, Viboud CG, et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis. 2012;54:1427–1436. doi: 10.1093/cid/cis211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among US children. N Engl J Med. 2015;372:835–845. doi: 10.1056/NEJMoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ambrose CS, Anderson EJ, Simões EAF, et al. Respiratory syncytial virus disease in preterm infants in the US born at 32–35 weeks gestation not receiving immunoprophylaxis. Pediatr Infect Dis J. 2014;33:576–582. doi: 10.1097/INF.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanken MO, Koffijberg H, Nibbelke EE, Rovers MM, Bont L, Dutch RSV Neonatal Network Prospective validation of a prognostic model for respiratory syncytial virus bronchiolitis in late preterm infants: a multicenter birth cohort study. PLoS ONE. 2013;8:e59161. doi: 10.1371/journal.pone.0059161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carbonell X, Fullarton JR, Gooch KL, Figueras-Aloy J. The evolution of risk factors for respiratory syncytial virus-related hospitalization in infants born at 32–35 weeks’ gestational age: time-based analysis using data from the FLIP-2 study. J Perinat Med. 2012;40:685–691. doi: 10.1515/jpm-2011-0248. [DOI] [PubMed] [Google Scholar]
- 7.Figueras-Aloy J, Carbonell-Estrany X, Quero J, IRIS Study Group Case-control study of the risk factors linked to respiratory syncytial virus infection requiring hospitalization in premature infants born at a gestational age of 33–35 weeks in Spain. Pediatr Infect Dis J. 2004;23:815–820. doi: 10.1097/01.inf.0000136869.21397.6b. [DOI] [PubMed] [Google Scholar]
- 8.Figueras-Aloy J, Quero-Jiménez J, Fernández-Colomer B, et al. Usefulness of different risk factor associations in predicting admissions due to respiratory syncytial virus in premature newborns of 32 to 35 weeks gestation in Spain [in Spanish] Ann Pediatr (Barc). 2009;71:47–53. doi: 10.1016/j.anpedi.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Law BL, Langley JM, Allen U, et al. The Pediatric Investigators Collaborative Network on Infections in Canada study of predictors of hospitalization for respiratory syncytial virus infection for infants born at 33 through 35 completed weeks of gestation. Pediatr Infect Dis J. 2004;23:806–814. doi: 10.1097/01.inf.0000137568.71589.bd. [DOI] [PubMed] [Google Scholar]
- 10.Resch B, Bramreiter VS, Kurath-Koller S, Freidl T, Urlesberger B. Respiratory syncytial virus associated hospitalizations in preterm infants of 29 to 32 weeks gestational age using a risk score tool for palivizumab prophylaxis. Eur J Clin Microbiol Infect Dis. 2017;36(6):1057. doi: 10.1007/s10096-016-2891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sommer C, Resch B, Simões EA. Risk factors for severe respiratory syncytial virus lower respiratory tract infection. Open Microbiol J. 2011;5:144–154. doi: 10.2174/1874285801105010144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simoes EA. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr. 2003;143(5):118–126. doi: 10.1067/S0022-3476(03)00511-0. [DOI] [PubMed] [Google Scholar]
- 13.Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360:588–598. doi: 10.1056/NEJMoa0804877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mauskopf J, Margulis A, Samuel M, Lohr KN. Respiratory syncytial virus hospitalizations in healthy preterm infants: systematic review. Pediatr Infect Dis J. 2016;35:e229–e238. doi: 10.1097/INF.0000000000001163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall CB, Weinberg GA, Blumkin AK, et al. Respiratory syncytial virus-associated hospitalizations among children less than 24 months of age. Pediatrics. 2013;132:e341–e348. doi: 10.1542/peds.2013-0303. [DOI] [PubMed] [Google Scholar]
- 16.Helfrich AM, Nylund CM, Eberly MD, Eide MB, Stagliano DR. Healthy late-preterm infants born 33–36 + 6 weeks gestational age have higher risk for respiratory syncytial virus hospitalization. Early Hum Dev. 2015;91:541–546. doi: 10.1016/j.earlhumdev.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Anderson EJ, Krilov LR, DeVincenzo JR, et al. SENTINEL1: an observational study of respiratory syncytial virus hospitalizations among US infants born at 29 to 35 weeks’ gestational age not receiving immunoprophylaxis. Am J Perinatol. 2017;34:51–61. doi: 10.1055/s-0036-1584147. [DOI] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality. HCUP NIS Database Documentation. Healthcare Cost and Utilization Project (HCUP). 2016. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed 25 Aug 2016.
- 19.Agency for Healthcare Research and Quality. KID Database Documentation. Healthcare Cost and Utilization Project (HCUP). 2016. https://www.hcup-us.ahrq.gov/db/nation/kid/kiddbdocumentation.jsp. Accessed 25 Aug 2016.
- 20.Chu HY, Steinhoff MC, Magaret A, et al. Respiratory syncytial virus transplacental antibody transfer and kinetics in mother-infant pairs in Bangladesh. J Infect Dis. 2014;210:1582–1589. doi: 10.1093/infdis/jiu316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glezen WP, Paredes A, Allison JE, Taber LH, Frank AL. Risk of respiratory syncytial virus infection for infants from low-income families in relationship to age, sex, ethnic group, and maternal antibody level. J Pediatr. 1981;98:708–715. doi: 10.1016/S0022-3476(81)80829-3. [DOI] [PubMed] [Google Scholar]
- 22.La Gamma EF, Kumar VR, Wadhawan R, et al. Receipt of palivizumab before birth hospitalization discharge among preterm infants in the United States. Am J Perinatol. 2015;32:1017–1023. doi: 10.1055/s-0034-1543951. [DOI] [PubMed] [Google Scholar]
- 23.Winterstein A, Knox CA, Kubilis P, Hampp C. Appropriateness of age thresholds for respiratory syncytial virus immunoprophylaxis in moderate-preterm infants: a cohort study. JAMA Pediatr. 2013;167:1118–1124. doi: 10.1001/jamapediatrics.2013.2636. [DOI] [PubMed] [Google Scholar]
- 24.Dougherty NN, Meissner HC. Respiratory syncytial virus immunoprophylaxis. PediatrDrugs. 2000;1:127–132. doi: 10.2165/00148581-200002020-00005. [DOI] [PubMed] [Google Scholar]
- 25.Boyce TG, Mellen BG, Mitchel EF, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid. J Pediatr. 2000;31:865–870. doi: 10.1067/mpd.2000.110531. [DOI] [PubMed] [Google Scholar]
- 26.Fryzek JP, Martone WJ, Groothuis JR. Trends in chronologic age and infant respiratory syncytial virus hospitalization: an 8-year cohort study. Adv Ther. 2011;28:195–201. doi: 10.1007/s12325-010-0106-6. [DOI] [PubMed] [Google Scholar]
- 27.Simoes EA, Anderson EJ, Wu X, Ambrose CS. Effects of chronologic age and young child exposure on respiratory syncytial virus disease among US preterm infants born at 32 to 35 weeks gestation. PLoS ONE. 2016;11:e0166226. doi: 10.1371/journal.pone.0166226. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from published literature (Hall et al. [15] and Helfrich et al. [16]), from the authors of the Anderson et al. study [17], or from the National Inpatient Sample database (https://www.hcup-us.ahrq.gov/nisoverview.jsp) and the Kids’ Inpatient Database (https://www.hcup-us.ahrq.gov/kidoverview.jsp), which have been developed and maintained by the Healthcare Cost and Utilization Project and are sponsored by the Agency for Healthcare Research and Quality, US Department of Health and Human Services.