Abstract
[Purpose] To determine the validity of knee extension muscle strength measurements using belt-stabilized hand-held dynamometry with and without body stabilization compared with the gold standard isokinetic dynamometry in healthy adults. [Subjects and Methods] Twenty-nine healthy adults (mean age, 21.3 years) were included. Study parameters involved right side measurements of maximal isometric knee extension strength obtained using belt-stabilized hand-held dynamometry with and without body stabilization and the gold standard. Measurements were performed in all subjects. [Results] A moderate correlation and fixed bias were found between measurements obtained using belt-stabilized hand-held dynamometry with body stabilization and the gold standard. No significant correlation and proportional bias were found between measurements obtained using belt-stabilized hand-held dynamometry without body stabilization and the gold standard. The strength identified using belt-stabilized hand-held dynamometry with body stabilization may not be commensurate with the maximum strength individuals can generate; however, it reflects such strength. In contrast, the strength identified using belt-stabilized hand-held dynamometry without body stabilization does not reflect the maximum strength. Therefore, a chair should be used to stabilize the body when performing measurements of maximal isometric knee extension strength using belt-stabilized hand-held dynamometry in healthy adults. [Conclusion] Belt-stabilized hand-held dynamometry with body stabilization is more convenient than the gold standard in clinical settings.
Keywords: Systematic bias, Body stabilization, Muscle strength
INTRODUCTION
Lower limb muscle strength is related to the ability to perform ambulatory activities, such as rising from a chair, walking at an appropriate speed, and ascending and descending stairs1,2,3,4,5). Current evidence suggests that loss of muscle strength is an important predictor of mobility limitation, physical disability, and mortality. Several studies have reported that knee extensor strength is important for activities of daily living (ADL) and have indicated the threshold value of knee extensor strength necessary to perform ADL6,7,8,9,10,11,12). It has been suggested that strength tests could be used to identify people who independently perform ADL but are at an increased risk of becoming dependent because of poor muscle strength.
In clinical settings, manual muscle testing is often used to measure muscle strength. However, objective data is required to generate standard values, such as the threshold of muscle strength necessary to perform ADL in an independent manner. Various types of dynamometry have been used to obtain objective data, and the gold standard is isokinetic dynamometry (GS) using an isometric dynamometer or hand-held dynamometer (HHD). In clinical settings, the HHD method is one of the most commonly used methods because of its convenience, portability, and ease of performance for both the examiner and subject, when compared with other dynamometry methods. However, HHD test results are influenced by factors, such as the examiner’s strength13,14,15,16,17) and the level of body stabilization of the subject18, 19). It has been reported that the strength values obtained using the HHD method are inaccurate13,14,15,16,17, 20,21,22).
Strength values obtained using the HHD method are dependent on the tester having adequate strength to hold the device against the effort of the individual being tested. Therefore, the dependence of the range of measurements on the strength of the tester reflects a limitation, and the inter-tester reliability of this method is low13,14,15,16,17). Belt-stabilized hand-held dynamometry (BSHHD) has been suggested to eliminate the need of the tester to apply force against a subject’s knee extension strength, and high intra- and inter-tester reliabilities of this method have been demonstrated in previous studies13, 23,24,25).
When using the HHD method, the extent of a subject’s stabilization may not be sufficient compared with that using GS and stationary isometric dynamometry. A few previous studies reported that a subject’s stabilization affects the maximum muscle strength, and if ample stabilization cannot be achieved, the maximum strength cannot be ascertained18, 19, 26, 27). Studies have reported that measurements obtained using HHD method were significantly lower than those obtained using GS and stationary isometric dynamometry20,21,22). In studies using BSHHD, subjects were sometimes seated on a chair with their bodies stabilized by belts23, 28), while in other studies, subjects were seated on the edge of a bed without body stabilization13, 24). Thus, there is no standardized approach with regard to BSHHD. If stabilization is lacking, the maximum knee extension strength might not be measured as good as when using GS, particularly in subjects with high muscle strength. Therefore, it is necessary to know the difference in strength identified using BSHHD with and without body stabilization compared with GS in order to determine a standard approach for BSHHD.
Bohannon et al.28) performed a BSHHD validation study and compared BSHHD with GS. In their study, participants were seated on a chair, and stabilizing straps were applied to the thighs and waist, indicating that body stabilization was not entirely comparable with that of GS. The authors found that measurements were significantly lower with the BSHHD method than with the GS method; however, a high correlation was found between the two methods. Meanwhile, this study did not evaluate systematic bias. Although a good correlation was found between the two methods, if systematic bias, such as fixed or proportional bias, were found, the two methods would not necessarily be in agreement. Therefore, it is necessary to completely examine the validity of the methods, and thus, not only the relationship between two types of measurements, but also the systematic bias should be assessed.
The aim of the present study was to determine the validity of maximal knee extension strength measurements using BSHHD with and without body stabilization compared with GS in healthy adults.
SUBJECTS AND METHODS
Healthy young adults were recruited among students from Shinshu University. Participants were excluded if they had a history of knee injury, cardiovascular symptoms, and neuromuscular, musculoskeletal, or other systematic diseases, or if they felt pain when performing leg muscle contraction. The study included data from 29 participants (20 male and 9 female participants). The study protocol was approved by the Medical Ethics Committee of Shinshu University School of Medicine (No. 2160). Prior to enrollment in the study, all participants were fully informed of the study’s purpose, procedures, and risks. Written informed consent was obtained from all participants.
Basic demographic and anthropometric data were obtained. Before the day of the test trial (2–7 days), instructions for positioning and testing were provided to each participant, and understanding was confirmed prior to the test. Additionally, maximum isometric contraction was practiced. Before each test, three submaximal contractions were performed as a warm-up. The maximum isometric knee extension strength of the right lower extremity was measured using the following three methods: 1) BSHHD with body stabilization, 2) BSHHD without body stabilization, and 3) GS. All measurements were performed by the same examiner. Subjects were seated with their hips and knees at approximately 90° of flexion for all methods.
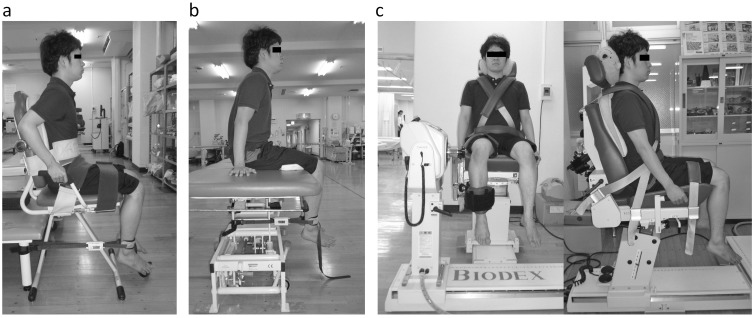
In BSHHD testing, a calibrated Mobie HHD (Sakai Med., Tokyo, Japan) was used for measurements. The Mobie HHD can be used in push and pull modes. In this study, the dynamometer was set to the pull mode and was placed between two belts, as in strain gauge methods. One belt was wrapped around the distal shank at the level of three fingers above the malleoli. Another belt was wrapped around the backward-fixed poll vertically (Fig. 1a, b). The distance from the estimated knee axis of rotation to the midpoint of the belt (width, 7 cm) was measured in meters as the lever length for torque calculation. During BSHHD with body stabilization, subjects were seated on a chair, and stabilizing straps were applied across the abdomen, waist, and both thighs. The subjects were instructed to hold on to the chair handles throughout the test (Fig. 1a). During BSHHD without body stabilization, subjects were seated on the edge of a table with their hands placed on the table (Fig. 1b). GS testing was performed using a Biodex isokinetic dynamometer (Biodex 4.0 system, Shirley, NY, USA). Subjects were seated on a Biodex chair, and stabilizing straps were applied across the chest, waist, and one of the thighs. The subjects were instructed to hold on to the chair handles throughout the test (Fig. 1c).
Fig. 1.
The three conditions used in the study to measure isometric knee extension strength. (a) Belt-stabilized hand-held dynamometry (BSHHD) with body stabilization, (b) BSHHD without body stabilization, (c) gold standard isokinetic dynamometry (GS) view from the front and side. Subjects were seated with their hips and knees at approximately 90° of flexion. (a)(b): The belt-stabilized hand-held dynamometry (BSHHD) sensor-fixing belt was located at a level of three fingers above the malleoli. (a): Subject’s stabilizing straps were applied across the abdomen and pelvis to suppress the anterior superior iliac spines on both sides and on both thighs. Hands held on to the chair handles. (b): No stabilizing strap was used. Subjects placed their hands on the table. (c): Subject’s stabilizing straps were applied across the chest, pelvis to push the bilateral anterior iliac spines, and one of the thighs. Hands held on to the chair handles.
Two maximum contractions of 5 s each were performed for each method with a 60-s rest period between contractions. Three test trials were performed randomly with a 10-min rest period before switching to a new method. Subjects were instructed to hold the position and to exert as much force as possible against the pad and stop if they felt pain during contraction. To encourage the subject, the words “push, push; more, more; relax” were used. No feedback on strength was provided until after completion of testing with all three methods.
For BSHHD testing, the peak force of each trial was recorded in Newton and was later converted according to lever length into torque (Nm) in order to compare the results with those of GS. For tests carried out with Biodex, the peak torque of each trial was recorded in Nm. The best torque from the two trials of each method was standardized by body weight (Nm/kg) and used for the analysis.
Standard descriptive statistics were calculated, and then, Spearman’s rank correlation coefficient and scatter plots were used to examine the relationships between measurements obtained using BSHHD with body stabilization and GS, and between measurements obtained using BSHHD without body stabilization and GS. Systematic biases, such as fixed and proportional bias, were assessed using Bland–Altman analyses29, 30). Bland–Altman plots provided a visual interpretation, in which the difference in torque between the two methods (GS and BSHHD) was plotted against the mean of the torque by the two methods for each subject. All data analyses were performed using the Statistical Package for Social Sciences (SPSS v18.0) software (IBM Corp., Armonk, NY, USA). The α level was set at 0.05.
RESULTS
The study included 29 participants. Their ages ranged from 20 to 35 years (21.3 ± 2.3 years), heights ranged from 155 to 186 cm (169.7 ± 7.5 cm), and body weights ranged from 47.0 to 100.2 kg (62.1 ± 12.2 kg). Additionally, their body mass index values ranged from 15.2 to 34.2 kg/m2 (21.6 ± 4.2 kg/m2).
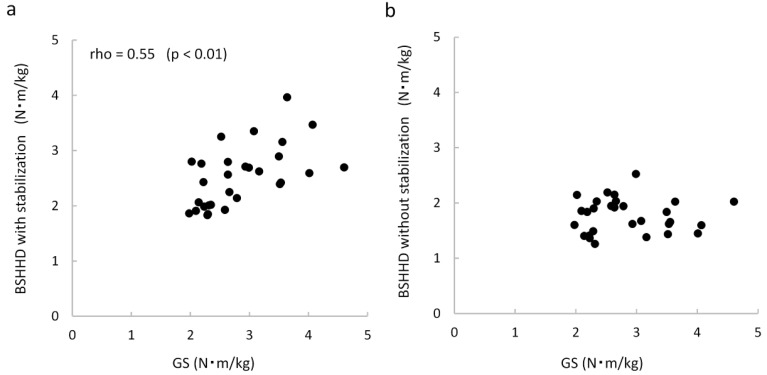
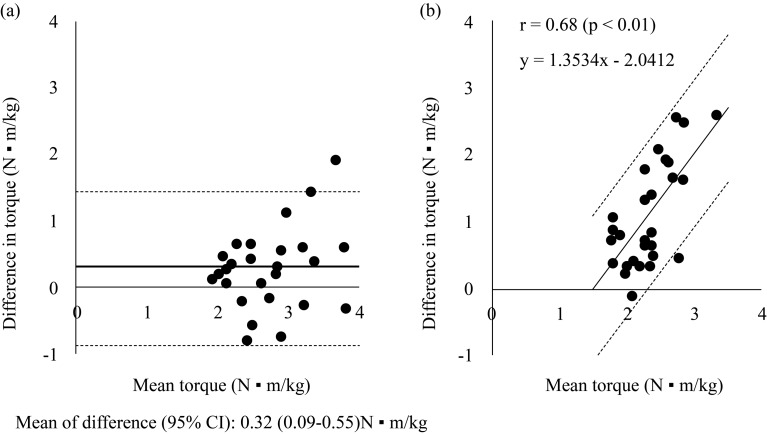
The knee extension strength of all participants could be assessed under the three conditions. Table 1 shows the maximum knee extension torque values obtained under each condition. Figure 2 shows the scatter plots of values obtained using BSHHD with or without body stabilization and GS. A moderate correlation was found between the values obtained using BSHHD with body stabilization and GS (rho=0.55, p<0.01); however, there was no significant correlation between the values obtained using BSHHD without body stabilization and GS. Figure 3a shows Bland-Altman plots of values obtained using BSHHD with body stabilization and GS. Fixed bias was found between the two types of measurements, suggesting that BSHHD tended to underestimate quadriceps strength by an average of 0.32 (95% confidence interval: 0.09, 0.55) Nm/kg, when compared with GS. Figure 3b shows Bland-Altman plots of values obtained using BSHHD without body stabilization and GS. Proportional bias was found between the two types of measurements, as indicated by the relationship between the mean torque value and difference in torque values (r=0.68, p<0.01). The difference between the values obtained using the two methods for each subject became increasingly more apparent among stronger subjects.
Table 1. Knee extension torque values obtained using each method.
| Method | Median (first quartile, third quartile) (Nm/kg) | Range (Nm/kg) |
|---|---|---|
| BSHHD with body stabilization | 2.56 (2.01, 2.79) | 1.83–3.96 |
| BSHHD without body stabilization | 1.84 (1.47, 2.02) | 1.26–2.52 |
| GS | 2.64 (2.26, 3.51) | 1.98–4.61 |
BSHHD: belt-stabilized hand-held dynamometry; GS: gold standard isokinetic dynamometry
Fig. 2.
Scatterplots illustrating the relationship between knee extension torque values obtained using BSHHD with body stabilization and GS (a) and BSHHD without body stabilization and GS (b). Moderate correlation is noted between BSHHD with body stabilization and GS; however, no correlation is noted between BSHHD without body stabilization and GS. GS: gold standard isokinetic dynamometry (Biodex 4); BSHHD: belt-stabilized hand-held dynamometry (Mobie)
Fig. 3.
Bland-Altman plots of the differences in torque values between BSHHD and GS against the mean torque value of both measurements for knee extension torque obtained using (a) BSHHD with body stabilization and GS, and (b) BSHHD without body stabilization and GS
Fixed bias is noted between BSHHD with body stabilization and GS, and the mean difference is 0.32 Nm/kg (a). Proportional bias is noted between BSHHD without body stabilization and GS (b). 95% CI: 95% confidence interval; GS: gold standard isokinetic dynamometry (Biodex 4); BSHHD: belt-stabilized hand-held dynamometry (Mobie). The solid line indicates the mean difference in torque values. Dashed lines show the 95% limit of value agreements
DISCUSSION
In this study, two conditions of BSHHD (with and without body stabilization) were compared with GS. The strength identified using BSHHD with body stabilization may not be commensurate with the maximum strength that can be generated by an individual, but it can reflect such strength. On comparing BSHHD with body stabilization and GS, fixed bias was observed. The strength measured using BSHHD with body stabilization was lower than that measured using GS (mean difference=0.32 Nm/kg). Bohannon et al.28) reported that values obtained using BSHHD were significantly lower than those obtained using the gold standard Biodex. The differences in torque values obtained using the two methods were 33.7 Nm for the right side and 35.6 Nm for the left side. For comparison, when converted to the torque weight ratio using the subject’s average body weight of 73.3 kg, it was 0.46 Nm/kg on the right side and 0.49 Nm/kg on the left side. These torque values were greater than the torque values obtained in our study. In the study by Bohannon et al., subjects only used stabilizing straps for the proximal part of the thigh and waist when tested with BSHHD. On the other hand, our subjects used stabilizing straps for the abdomen, waist, and thigh, and they held on to the chair handles during BSHHD with body stabilization. Therefore, the difference was associated with the extent of subject stabilization, and our BSHHD method with body stabilization was almost equivalent to the GS method. However, fixed bias occurred in our study. We speculated that there were two reasons for the difference between values obtained using BSHHD with body stabilization and those obtained using GS. The major reason for the difference could be the difference in calculation of torque values. In this study, lever length determined the distance from the estimated knee axis to the midpoint of the belt. Because the width of the belt was 7 cm, when measured at the distal end, the length increased by 3.5 cm. As a result, the obtained torque values were higher, and the fixed bias was reversed. Another reason for the difference could be the difference in stabilizing the subject’s upper body. In BSHHD, stabilizing straps were applied only across the abdomen, whereas in GS, these were applied across the chest as well.
Because proportional bias affected by subject strength did not exist between values obtained using BSHHD with body stabilization and those obtained using GS, we thought that the fixed bias was an instrumental error related exclusively to the calculation of the lever length. Therefore, BSHHD with subject stabilization methods should be introduced as a substitute for GS methods to assess the knee extension strength.
We found that the strength identified using BSHHD without body stabilization did not reflect the maximum strength. In the current study, there was proportional bias, and the difference in measurements obtained using BSHHD without body stabilization and GS increased in association with increasing strength. In addition, the maximum torque value obtained using BSHHD without body stabilization was 2.52 Nm/kg, which was lower than the median torque value obtained using GS (2.64 Nm/kg). Mendlar19) reported that isometric knee extension force increased when an added stabilization of the body was provided. The subject demonstrated maximum force when the stabilization was provided using thigh cuffs, backboard, and the hand grip. On the other hand, approximately 70% of the maximum force was demonstrated in the case where the stabilization was provided by the weight of the body on the table surface. Therefore, it is clear that BSHHD without body stabilization cannot measure the maximum strength in healthy young subjects.
Suzuki25) reported that intra-examiner and inter-examiner reliabilities of isometric knee extension muscle strength measurements of healthy young adults obtained using BSHHD without body stabilization were acceptable. However, in this study, the mean values of the measurements were approximately 40 kgf, and these were lower that our values obtained using BSHHD with body stabilization. Therefore, this method could fail in the measurement of maximum strength.
Our findings may not be reflective of old people and patients who are weaker than the young adults assessed. Further research is needed to identify the range that can produce valid measurements using BSHHD without subject stabilization. If a subject’s knee extension torque exceeds the upper body weight torque, his/her hip will float on the seat and the maximum strength cannot be measured. As long as this hypothesis is valid, for subjects whose knee extension torque is less than the body weight torque, the maximum knee strength can be measured using BSHHD without subject stabilization. Thus, it is necessary to investigate the use of BSHHD without validation of subject’s stabilization method, aimed at weak-strength subjects.
A chair should be used to stabilize the body when performing measurements of maximum isometric knee extension strength using BSHHD in healthy adults. This approach is more convenient than GS in clinical settings.
Acknowledgments
This study was funded by the Shinshu University. The authors would like to thank the Fujimi Kogen Hospital staff for their support.
REFERENCES
- 1.Corrigan D, Bohannon RW: Relationship between knee extension force and stand-up performance in community-dwelling elderly women. Arch Phys Med Rehabil, 2001, 82: 1666–1672. [DOI] [PubMed] [Google Scholar]
- 2.Marsh AP, Miller ME, Saikin AM, et al. : Lower extremity strength and power are associated with 400-meter walk time in older adults: The InCHIANTI study. J Gerontol A Biol Sci Med Sci, 2006, 61: 1186–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakao H, Yoshikawa T, Mimura T, et al. : Influence of lower-extremity muscle force, muscle mass and asymmetry in knee extension force on gait ability in community-dwelling elderly women. J Phys Ther Sci, 2006, 18: 73–79. [Google Scholar]
- 4.Ringsberg K, Gerdhem P, Johansson J, et al. : Is there a relationship between balance, gait performance and muscular strength in 75-year-old women? Age Ageing, 1999, 28: 289–293. [DOI] [PubMed] [Google Scholar]
- 5.Samuel D, Rowe P, Hood V, et al. : The relationships between muscle strength, biomechanical functional moments and health-related quality of life in non-elite older adults. Age Ageing, 2012, 41: 224–230. [DOI] [PubMed] [Google Scholar]
- 6.Barbat-Artigas S, Rolland Y, Cesari M, et al. : Clinical relevance of different muscle strength indexes and functional impairment in women aged 75 years and older. J Gerontol A Biol Sci Med Sci, 2013, 68: 811–819. [DOI] [PubMed] [Google Scholar]
- 7.Eriksrud O, Bohannon RW: Relationship of knee extension force to independence in sit-to-stand performance in patients receiving acute rehabilitation. Phys Ther, 2003, 83: 544–551. [PubMed] [Google Scholar]
- 8.Hasegawa R, Islam MM, Lee SC, et al. : Threshold of lower body muscular strength necessary to perform ADL independently in community-dwelling older adults. Clin Rehabil, 2008, 22: 902–910. [DOI] [PubMed] [Google Scholar]
- 9.Manini TM, Visser M, Won-Park S, et al. : Knee extension strength cutpoints for maintaining mobility. J Am Geriatr Soc, 2007, 55: 451–457. [DOI] [PubMed] [Google Scholar]
- 10.Moreland JD, Richardson JA, Goldsmith CH, et al. : Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc, 2004, 52: 1121–1129. [DOI] [PubMed] [Google Scholar]
- 11.Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, et al. : Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci, 2002, 57: B144–B152. [DOI] [PubMed] [Google Scholar]
- 12.Rantanen T, Avlund K, Suominen H, et al. : Muscle strength as a predictor of onset of ADL dependence in people aged 75 years. Aging Clin Exp Res, 2002, 14: 10–15. [PubMed] [Google Scholar]
- 13.Katoh M, Yamasaki H: Comparison of reliability of isometric leg muscle strength measurements made using a hand-held dynamometer with and without a restraining belt. J Phys Ther Sci, 2009, 21: 37–42. [Google Scholar]
- 14.Lu TW, Hsu HC, Chang LY, et al. : Enhancing the examiner’s resisting force improves the reliability of manual muscle strength measurements: comparison of a new device with hand-held dynamometry. J Rehabil Med, 2007, 39: 679–684. [DOI] [PubMed] [Google Scholar]
- 15.Lu YM, Lin JH, Hsiao SF, et al. : The relative and absolute reliability of leg muscle strength testing by a handheld dynamometer. J Strength Cond Res, 2011, 25: 1065–1071. [DOI] [PubMed] [Google Scholar]
- 16.Mulroy SJ, Lassen KD, Chambers SH, et al. : The ability of male and female clinicians to effectively test knee extension strength using manual muscle testing. J Orthop Sports Phys Ther, 1997, 26: 192–199. [DOI] [PubMed] [Google Scholar]
- 17.Wikholm JB, Bohannon RW: Hand-held dynamometer measurements: tester strength makes a difference. J Orthop Sports Phys Ther, 1991, 13: 191–198. [DOI] [PubMed] [Google Scholar]
- 18.Hart DL, Stobbe TJ, Till CW, et al. : Effect of trunk stabilization on quadriceps femoris muscle torque. Phys Ther, 1984, 64: 1375–1380. [DOI] [PubMed] [Google Scholar]
- 19.Mendler HM: Effect of stabilization on maximum isometric knee extensor force. Phys Ther, 1967, 47: 375–379. [DOI] [PubMed] [Google Scholar]
- 20.Arnold CM, Warkentin KD, Chilibeck PD, et al. : The reliability and validity of handheld dynamometry for the measurement of lower-extremity muscle strength in older adults. J Strength Cond Res, 2010, 24: 815–824. [DOI] [PubMed] [Google Scholar]
- 21.Martin HJ, Yule V, Syddall HE, et al. : Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology, 2006, 52: 154–159. [DOI] [PubMed] [Google Scholar]
- 22.Nollet F, Beelen A: Strength assessment in postpolio syndrome: validity of a hand-held dynamometer in detecting change. Arch Phys Med Rehabil, 1999, 80: 1316–1323. [DOI] [PubMed] [Google Scholar]
- 23.Desrosiers J, Prince F, Rochette A, et al. : Reliability of lower extremity strength measurements using the belt-resisted method. J Aging Phys Act, 1998, 6: 317–326. [Google Scholar]
- 24.Katoh M, Yamasaki H: Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: Comparisons during and between sessions. J Phys Ther Sci, 2009, 21: 239–243. [Google Scholar]
- 25.Suzuki T: Reliability of measurements of knee extensor muscle strength using a pull-type hand-held dynamometer. J Phys Ther Sci, 2015, 27: 967–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magnusson SP, Geismar RA, Gleim GW, et al. : The effect of stabilization on isokinetic knee extension and flexion torque production. J Athl Train, 1993, 28: 221–225. [PMC free article] [PubMed] [Google Scholar]
- 27.Ricard G, Currier DP: Back stabilization during knee strengthening exercise. Phys Ther, 1977, 57: 1013–1015. [DOI] [PubMed] [Google Scholar]
- 28.Bohannon RW, Bubela DJ, Wang YC, et al. : Adequacy of belt-stabilized testing of knee extension strength. J Strength Cond Res, 2011, 25: 1963–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bland JM, Altman DG: Statistical methods for assessing agreement between two methods of clinical measurement. Lancet, 1986, 1: 307–310. [PubMed] [Google Scholar]
- 30.Bland JM, Altman DG: Measuring agreement in method comparison studies. Stat Methods Med Res, 1999, 8: 135–160. [DOI] [PubMed] [Google Scholar]