Figure 2.
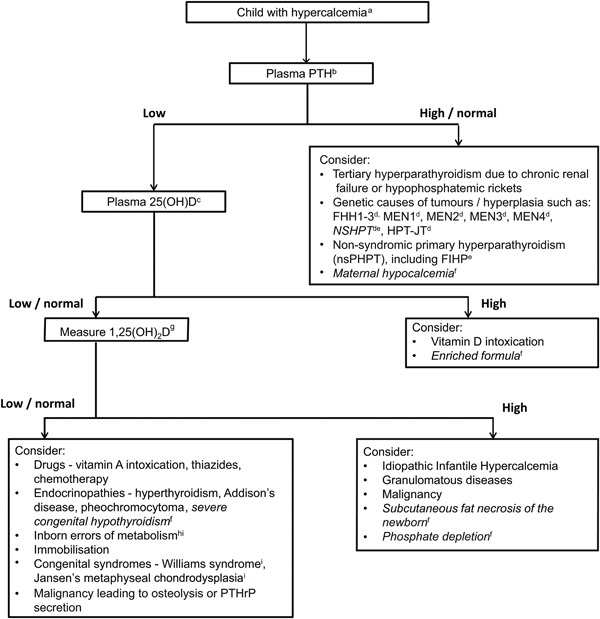
Clinical approach to investigation of causes of hypercalcemia in a child. aConfirm hypercalcemia, defined as plasma (or serum) adjusted calcium > 10.5 mg/dL (2.60 mmol/L) or ionized calcium > 5.25 mg/dL (1.32 mmol/L) (see Table 2). bPTH–parathyroid hormone. c25(OH)D–25‐hydroxyvitamin D. dFHH1‐3– Familial Hypocalciuric Hypercalcemia types 1‐3; MEN1–Multiple Endocrine Neoplasia type 1; MEN2–Multiple Endocrine Neoplasia type 2; MEN3–Multiple Endocrine Neoplasia type 3; MEN4–Multiple Endocrine Neoplasia type 4; NSHPT–Neonatal Severe Primary Hyperparathyroidism; HPT‐JT–Hyperparathyroid‐Jaw Tumour syndrome. eFamilial Isolated Hyperparathyroidism. fConditions affecting neonates (shown in italics). g1,25(OH)2D–1,25‐dihydroxyvitamin D. hInborn errors of metabolism, e.g. Hypophosphatasia, Congenital Lactase Deficiency (CLD) and blue diaper syndrome. iThese syndromes may be associated with dysmorphic features, e.g. Williams syndrome, Jansen's metaphyseal chondrodysplasia, Hypophosphatasia.
