Abstract
Access to reliable transportation is important for people with chronic diseases considering the need for frequent medical visits and for medications from the pharmacy. Understanding of the extent to which transportation barriers, including lack of transportation, contribute to poor health outcomes has been hindered by a lack of consistency in measuring or operationally defining “transportation barriers.” The current study uses the Rasch measurement model to examine the psychometric properties of a new measure designed to capture types of transportation and associated barriers within an urban context. Two hundred forty-four adults with Type 2 diabetes were recruited from within an academic medical center in Chicago and completed the newly developed transportation questions as part of a larger National Institute of Health funded study (ClinicalTrials.gov identifier: NCT01498159). Results suggested two subscale structure that reflected 1) general transportation barriers and 2) public transportation barriers.
Approximately half of all adults in the United States - over 100 million people - are diagnosed with a chronic disease such as hypertension, diabetes, or cancer (Ward, Schiller, and Goodman, 2014). Medical management of these diseases typically involves long-term use of medication prescriptions and frequent healthcare visits. For individuals with limited economic resources, transportation to provider visits and pharmacies may be a significant barrier to care that can alter health outcomes (Syed, Gerber, and Sharp, 2013; Ramirez, Perez-Stable, Penedo, Talavera, Carrillo, Fernandez, Holden, Munoz, San Miguel, Gallion, 2014; Tejeda, Darnell, Cho, Stolley, Markossian, Calhoun, 2013). Within the context of chronic disease management, timely visits to providers are needed to assess treatment response, evaluate for medication side effects, and renew or change medication prescriptions. Additional transportation may be required to access pharmacies where prescriptions are filled. As a result, missed provider appointments and delays in filling medications may adversely affect chronic disease control.
A recent review of empirical research addressing the relationship between transportation barriers and health care access in patients with chronic disease highlighted a critical methodological problem related to the operational definition of transportation barriers (Syed et al., 2013). Much of the research conducted to date has failed to conceptualize and operationalize transportation barriers in a comprehensive and systematic manner. In fact, most studies have relied on individual item indicators or a few items that simply ask if the person experienced problems with transportation (Syed et al., 2013). Other studies include focus groups where participants cite transportation as a barrier to chronic disease self-management in addition to others (Jerant, von Friederich-Fitzwater, and Moore, 2005). Few, if any, studies report on the psychometric properties of the selected transportation question(s). This is problematic for several reasons. First, transportation barriers may be context specific. For example, transportation issues in urban populations may need to consider access to public transportation, neighborhood safety, or traffic. Conversely, distance may be more important for rural populations. Time taken for transportation has relative importance and often is not fully reflected in distance traveled. The use of public transportation, vehicle ownership, access to a driver, transportation benefits through insurance, and mobility disabilities are issues that potentially contribute to difficulties in travel. Additionally, a metric of travel difficulty may be useful in relating to various elements of chronic disease care. This may include missed or delayed appointments, medication adherence and persistence, receipt of outpatient therapies, and overall outpatient access and utilization. While potentially most relevant among low-income, urban people, this metric may be applied across other populations as well.
With this in mind, the current study was designed to evaluate the psychometric properties of a new measure of transportation barriers in urban populations specific to healthcare matters. We elected to use Rasch measurement to model our data. Rasch is a prescriptive, rather than descriptive model, meaning it provides properties a measure should have to be useful (Linacre, 2000). The Rasch model (Rasch, 1960/1993) provides an advantage over other psychometric models, such as true score test theory or multi-parameter item response theory models, by focusing on item function and dimensionality, eliminating the impact of confounding factors, and maximizing the potential for objective measurement of the latent construct (Fisher, 1994). Ultimately, this analysis would allow for further refinement of the scale. This is particularly important in measuring transportation barriers because the type of transportation barriers may vary with the characteristics of the individual or population under study. Rasch measurement theory allows for the development of a measure that is non-sample dependent (Smith, 2001), meaning the structure of item difficulties is applicable beyond the sample used in development.
Methods
Participants
Two hundred forty-four participants were recruited from within four primary care outpatient clinics affiliated with an academic medical center in Chicago to participate in a larger National Institute of Health funded study (ClinicalTrials.gov identifier: NCT01498159). The larger study aimed to evaluate the role of clinical pharmacists and community health workers in supporting diabetes self-management- (Gerber et al., 2012). Inclusion criteria for the larger study included: (1) self-identifying as African American/Black or Latino/Hispanic; (2) having verbal fluency in English or Spanish; (3) being 21 years old or above; (4) physician diagnosed Type 2 diabetes with a documented history of poor glycemic control (hemoglobin A1C≥ 8%) within 12 months prior to recruitment; (5) seen by a primary care provider within the healthcare system for at least the past 12 months; and (6) currently prescribed one or more oral medications to treat diabetes or hypertension. By virtue of having at least one chronic disease, patients needed to make multiple visits to the healthcare setting each year. During the baseline data collection for the study, all participants completed a series of questionnaires that included the measure assessing transportation barriers. The study was approved by the Institutional Review Board at the University of Illinois at Chicago.
Measure
The transportation measure was comprised of items developed after conducting a review of the existing literature on transportation barriers associated with seeking healthcare (Syed, 2013). The review failed to identify any consensus on measurement of transportation barriers. Therefore, we generated items based upon prior studies and knowledge of urban transportation barriers experienced by patients. The final draft survey was reviewed for clarity and content by two team members independently. Modifications were made prior to administering it verbally to participants.
As shown in Appendix 1, the first question on the survey identifies the respondent’s usual transportation method to attend health care appointments: bus, drive self, someone else drives, “L” train, taxi, walk, or other. Questions 2–7 assess transportation barriers in general, including difficulty getting transportation (item 2), delaying scheduling an appointment (item 3), travel time (item 4), being 20 or more minutes late to an appointment (item 5), and missing appointments (item 6). Open-ended questions were used to gather more information about these experiences, including what transportation issues caused them to be late for (item 5a) or miss an appointment (item 6a), and a recent experience with transportation barriers (item 7). All participants responded to questions 2-6, with additional questions (5a, 6a, and 7) depending on responses to 5 and/or 6.
Item 8 was a multi-part question specific to the kind of transportation the respondent reported using (as indicated in item 1). Respondents who were driven by someone were asked if not having a ride ever prevented them from seeing their primary care doctor (8a). Respondents who drove themselves were asked about cost of gasoline as a barrier (8b). Bus, “L” train, and taxi were separate options in question 1, but were combined for question 8c, which addresses cost of public transit/taxi as a barrier, and 8d, which asks for an estimate of the roundtrip cost. Individuals taking the bus or “L” train also responded to questions 8e-h, which asked if any of the following were barriers to utilizing public transit to attend primary care appointments: distance to transit stop (8e), number of transfers (8f), safety issues (8g), and presence of physical disabilities (8h). Individuals who reported walking or using another transportation method did not respond to any parts of question 8.
All participants responded to question 9, which assessed whether the respondent had ever run out of medication due to transportation barriers. Participants responded to additional questions, including an open-ended question about the specific transportation barriers to refilling medications (9) and a close-ended question on how frequently this occurs (9b). Question 10 was an open-ended question about what would help ameliorate transportation barriers.
Analysis
Psychometric analyses were conducted using the Rasch grouped-items rating scale model. The Rasch model (Rasch, 1960/1980) is a logarithmic model that transforms qualitatively ordered (ordinal) scales to interval scales of measurement (Wright and Mok, 2004). Rasch provides a model for ordering persons according to their ability (or amount of trait they possess) and ordering items according to their difficulty (or the amount of trait needed to respond in a certain way to an item) (Bond and Fox, 2007). Because both person ability and item difficulty are calibrated on the same scale (expressed as logits), the probability of a specific response pattern can be estimated based on the difference between person ability and item difficulty:
where loge is the natural log, Pni1 is the probability that person n of ability Bn selects response option 1 (e.g., Yes) for item i of difficulty Di, and Pni0 is 1 – Pni1, or the probability of selecting response option 0 (e.g., No). For questions with more than two response options, the probability is expressed as:
where Fj is the threshold difficulty, or the additional amount of trait needed to respond to category j versus j-1. A grouped-items model allows items using the same rating scale to have the same response structure, while allowing other items to have a unique structure (e.g., partial credit) (Linacre, 2000).
While rating scales allow researchers to understand the extent to which a trait is present, use of rating scales introduces complexity to measurement, particularly when multiple rating scales are used within the same measure. Pivot anchoring is used to define transition points within the rating scales, particularly when multiple rating scales are used, to ensure comparability across items (Bode, 2004). For the present measure, pivot anchors were placed where the individual moved from having none of the trait (lowest category) to some of the trait, following the procedure identified by Bode (2004).
Analysis was performed using Stata 13.1 (StataCorp LP, College Station, TX) for descriptive analysis and Winsteps® 3.74.0 (Linacre, 2012) for Rasch analyses. The psychometric analysis approach was multi-stage and iterative; results from a stage indicating poor fit to the Rasch model led to changes to the dataset (e.g., drop or recode items, drop persons, etc.), and previously conducted analyses were repeated with the modified data. Analyses progressed as follows.
Dimensionality
Data were assessed for potential violations to the Rasch assumption of unidimensionality (i.e., that the items measure only one latent construct) (Smith, 2004). Principal components analysis (PCA) was used to determine the number of latent variables present in the data. Two criteria were used to understand PCA results: (1) the variance explained by the first dimension (the latent variable, i.e., transportation barriers) should be at least 40% and (2) the eigenvalue of the unexplained variance in the first contrast should be less than 2.
Item point-measure correlations are the Pearson’s correlation coefficient between each individual item and the total score of all other items. These values should be non-zero and positive, and should be similar to (or greater than) expected correlations based on the Rasch model. Items with low point-measure correlations were dropped. Item- and person-level fit indices were also examined, which compare observed to expected (based on the Rasch model) responses; these values are based on chi-square fit statistics (Smith, 2004) and should be less than 2.0 and greater than −2.0 (Linacre, 2002). OUTFIT (or Outlier sensitive) statistics are sensitive to responses that fall outside of the targeted ability level, such as a person with a low ability level responding correctly to a difficult item (Wright and Mok, 2004). INFIT (Information weighted) statistics are sensitive to responses that are too predictable, and provide little information (Wright and Mok, 2004). Misfitting items may need to be dropped from the dataset before analysis can proceed to the next step. For person misfit, Linacre (2010) recommends removing persons with very high OUTFIT mean-squares and cross-plotting estimates from the smaller sample against the full sample. If removal of these persons has little effect on the final estimates, these persons can be retained. If there is a difference, he recommends next examining persons with smaller (but still greater than 2.0) OUTFIT mean-squares in a similar manner. For the purposes of this project, an OUTFIT mean-square of 3.0 was deemed ‘very high’ and 2.0 was deemed ‘high.’
Rating scale function
Difficulty thresholds for response options were also examined to ensure categories progressed monotonically, meaning that selecting a higher response option on an ordinal scale was associated with higher person ability. Overall model fit was also examined through log-likelihood chi-square, person and item reliability, and person and item separation. Chi-square provides a measure of goodness of fit between the observed data and the Rasch model; though a significant chi-square indicates the observed data differ from the Rasch model, this figure is biased to be significant when sample sizes are large. To minimize the effect of sample size on chi-square, the normed chi-square will be computed (χ2/df) (Wheaton, 1977); the critical value for chi-square with df = 1 (3.841) was used to determine statistical significance.
Reliability is measured separately for persons and items. Person reliability is similar to the classical test theory notion of reliability, referring to replicability of the test results (Linacre, 1997). Item reliability refers to the replicability of the item hierarchy (difficulty levels). Separation indices are also provided for both persons and items. Person separation indicates the number of performance groups the measure is able to differentiate among in the sample (Wright and Stone, 1979). Item separation represents the number of distinguishable difficulty levels for the measure items; for example an item separation of 3 indicates the presence of distinguishable low, medium, and high difficulty items. (Wright and Stone, 1979).
Finally, the distributions of item difficulties and person abilities were also examined. Because item difficulties and person abilities are on the same scale, these values can be directly compared to determine whether the items align well with the ability levels of the present sample. A variable map was generated, placing participants or groups of participants on one side of the continuum, and items on the other side, allowing for identification of gaps in item difficulties, such as a lack of easy or difficult items. For rating scales with 3 or more options, difficulty thresholds are also included on the map.
Differential item function
Differential item function (DIF) analyses were conducted using Winsteps® to determine if items function in the same way among different participant groups, specifically sex, race (African-American, Latino/Hispanic), education (less than high school (HS), HS diploma, any college), employment (unemployed, employed), marital status (unmarried, married), and health status (poor/fair, good/very good/excellent). (Linacre, 2012) The assumption in Rasch analysis is that item function is uniform across various groups. Differences by group mean that certain groups require more or less of the underlying trait to respond in a specific way compared to other groups (Lai, Teresi, and Gershon, 2005). Item difficulties were examined by these target subgroups, as well as for the overall sample, and resulting difficulties were compared using Welch’s t-test. Unlike Student’s t, Welch’s t does not assume equal variances across groups and calculates degrees of freedom differently, minimizing potential inflation of the type I error rate (Ruxton, 2006). Items found to have significant DIF were examined to determine their potential impact on scores.
Because only a small proportion of respondents participated in the interview in Spanish (n = 28, 11.5%), traditional DIF analysis could not be conducted between these groups. Therefore, analyses were conducted with the whole sample, and again with only respondents who participated in English, and the resulting item difficulties and person abilities were cross-plotted in Winsteps®. This form of sensitivity analysis can provide indirect evidence of the impact of language of interview.
Results
Sample Characteristics
Participants were predominantly women (67.2%), African-American/Black (73.4%), and unmarried (71.3%) with an average age of 48.8 years (SD=13.0). Nearly half of the sample (47.5%) reported their health status as fair, and over half (56.6%) reported insurance as Public Aid/Medicaid. The majority had completed high school (70.5%), and approximately one-fourth of the sample was currently employed (21.8%).
A third of the sample reported taking a bus or “L” train as their usual form of transportation; only 2.5% reported taking a taxi. Approximately 27% stated they drove themselves, and 21.4% stated that someone else drove them. Finally, a small number of respondents reported using transportation provided through Medicaid or another service (13.5%) or walking (2.0%).
Dimensionality
Principal components analysis
Principal components analysis (PCA) of the 14 items (highlighted in Appendix 1) demonstrated that 58.4% of the variance was explained by the measure; this resulted in 41.6% unexplained variance. The first contrast had an eigenvalue of 5.5 (16.4% of the total variance), suggesting the existence of subscales. Standardized residual loadings by item suggested that items 8c and 8e–8h loaded onto a single scale (factor loadings ranged from 0.79 to 0.95). These represent the items responded to by individuals who reported using public transit (bus or L train); 8c was also responded to by individuals who reported taking a taxi to their appointments. The remaining items loaded on another factor.
The second contrast has an eigenvalue of 1.9 (5.6% of the total variance), less than the cut-off of 2 and substantially smaller than the eigenvalue of the first contrast. Standardized residual loadings suggested that items 9 and 9b may load onto a single scale (factor loadings were 0.87 and 0.88, respectively). However, for the present analyses, these items were retained in subscale 1. Items 8c and 8e-h were retained as subscale 2, with these analyses performed only on the public transportation group (n=81). When dimensionality analyses were performed by subscale, it was found that 50.1% of the variance was explained by the measure for subscale 1, and 60.8% of the variance was explained by the measure for subscale 2.
Item point-measure correlations
Item correlations with the overall measure were examined by subscale. In subscale 1, two items had correlations that were much smaller than expected values, item 8a (r = 0.27, expected r = 0.46) and 8b (r = 0.14, expected r = 0.49). These two items were responded to by individuals who reported someone else drove them or that they drove themselves, respectively. Analysis of these groups separately confirmed that these questions did not correlate with total score of the remaining items: item 8a (lack of ride results in missed appointment) in someone else drives dataset, r = 0.00, expected r = 0.31; item 8b (cost of gas for car) dataset, r = 0.00, expected r = 0.44. These items were removed from the full dataset. All remaining subscale 1 items had positive correlations, ranging from 0.55 to 0.71. In subscale 2, item correlations were strong and positive, ranging from 0.56 to 0.75. No items were removed from subscale 2 as a result of item point-measure correlations.
Item and person fit
All item fit statistics were less than +2 and greater than −2 for both subscales, indicating that these items fit on their respective subscales. No items were removed.
Several respondents had high INFIT and OUTFIT statistics for both subscales. Following guidance from Linacre (2010), the 6 respondents who had OUTFIT values greater than 3 were removed from subscale 1, and person measures were cross-plotted to compare the full sample (no deletions) with the N-6 sample. As demonstrated in the cross-plot (see Figure 1), the removal of these 6 respondents had little effect on the distribution of scores and all values fall within the confidence bands. This process was repeated with the 8 respondents who had OUTFIT values greater than 3 for subscale 2. Once again, the removal of 8 misfitting persons had little effect on the distribution of scores (see Figure 2). Therefore, all participants were retained for subsequent analyses.
Figure 1.
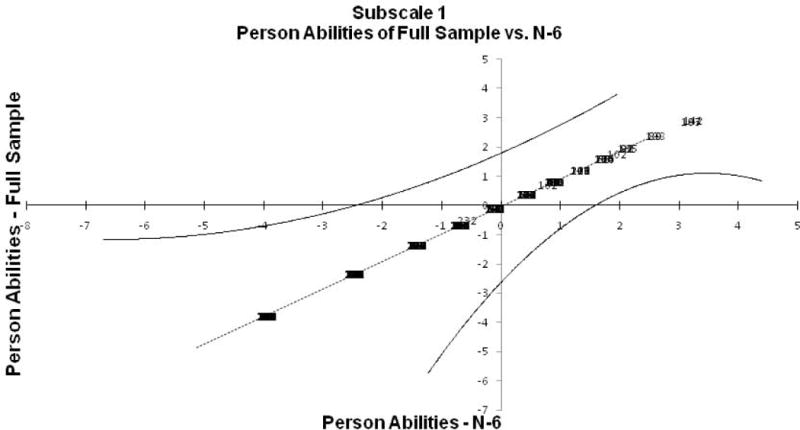
Figure 2.
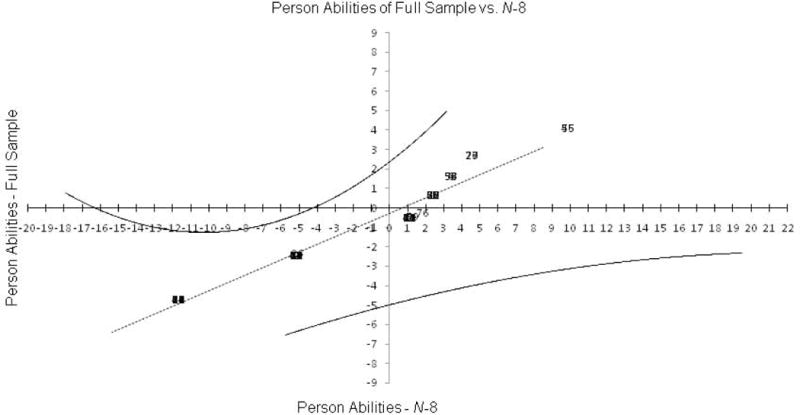
Cross-plot full sample without missfitting persons subscale 2
Rating Scale Function
Category function
Category function analysis of subscale 1 showed that the response options for item 2 did not progress monotonically; the response option 4 ‘A Lot of Trouble’ had a lower difficulty threshold (−2.60) than option 3 ‘Some Trouble’ (−2.54). This suggests that option 3 should be combined with another category. (See Table 1 for distribution of scores). Though the distribution is positively skewed, combining categories 2 and 3 would keep the distribution relatively similar in shape. These categories were combined. Additionally, response options for 9b demonstrated poor rating scale function; two categories did not progress monotonically (option 1 ‘Rarely’, 1.17; option 2 ‘Sometimes’, 1.08), and the first three response options differed by less than 0.5 logits. Because combining categories would make this question too similar to question 9, this item was dropped. Once these changes were made, and analyses rerun, no additional issues were noted with category function. Response options for subscale 2 items all progressed monotonically. No additional changes were made to the response structure.
Table 1.
Distribution of Scores for Item 2 (Difficulty Getting Transportation).
| Response Option | Frequency (Percent) |
|---|---|
| 1 – No Trouble | 146 (59.8%) |
| 2 – A Little Trouble | 37 (15.2%) |
| 3 – Some Trouble | 36 (14.8%) |
| 4 – A Lot of Trouble | 24 (3.8%) |
Overall model fit
For subscale 1, the log-likelihood chi-square is significant, χ2 (df = 942) = 1329.33, p < 0.001, indicating a departure from the Rasch model; however, the normed chi-square is not significant, χ2 (df = 1) = 1.41, p = 0.17, suggesting this chi-square may be inflated due to large sample size. Item difficulties ranged from −1.95 to 1.58. Person abilities ranged from −3.50 to 4.87. These ranges suggest that most items are more difficult than participants’ ability levels. The scale shows low-moderate person reliability, 0.51, and person separation, 1.03, and excellent item reliability, 0.97, and item separation, 5.94.
For subscale 2, the log-likelihood chi-square is not significant, χ2 (df = 240) = 238.52, p = 0.51. Item difficulties ranged from −3.74 to 2.42. Person abilities ranged from −4.69 to 4.12. These ranges demonstrate that items on this subscale lack high difficulty for the small group with more public transit transportation barriers. Additionally, the scale shows poor person reliability, 0.36, and person separation, 0.75, but excellent item reliability, 0.96, and item separation, 5.15.
Differential Item Function
Two questions from subscale 1 showed differences. Item 4 showed differences by education, employment status, gender, and race. Individuals with less than a high school diploma needed 0.57 more logits of the trait than individuals with a high school diploma, t (df = 161) = 2.07, p = 0.04, and 1.20 more logits than individuals with any college, t (df = 121) = 3.72, p = 0.0003. Additionally, individuals with a high school diploma needed 0.63 more logits of the trait than individuals with any college, t (df = 126) = 2.20, p = 0.03. Individuals who were unemployed needed 0.59 logits more of the trait than individuals who were employed, t (df = 114) = 2.12, p = 0.04. Additionally, men needed 0.49 logits more of the trait than women, t (df = 185) = 2.00, p = 0.05. Finally, African-American participants needed 0.59 more logits of the trait than participants who Latino/Hispanic, t (df = 147) = −2.16, p = 0.03.
Finally, item 5 showed differences only by employment status; unemployed participants needed 0.83 more logits of the trait than employed participants, t (df = 112) = 2.30, p = 0.02.
Though these differences are statistically significant, they would likely have little practical impact on scores. For instance, an individual who was unemployed would have only 0.23 logit difference in their estimated trait level for subscale 1 because of these differences. Differences by education level would only range from 0.10 to 0.20 logits.
No items from subscale 2 showed any differences.
Language of interview
Analyses conducted with individuals who completed the interview in English were similar to the overall analyses with one exception. Item difficulties and person abilities were generally unchanged.
Discussion
Within the clinical setting, missing appointments due to a lack of transportation is common. The empirical literature suggests that between 10% – 51% of patients report transportation as a barrier to obtaining healthcare (Syed et al., 2013). However, the accuracy of these reports is questionable because of the lack of any validated approach to measuring transportation barriers relevant to accessing healthcare visits. These numbers vary in part because the approach to measurement was inconsistent across studies. The current study fills a gap by providing a psychometric description of a new tool to assess transportation barriers that urban populations might face in traveling to their healthcare setting. Rasch measurement was selected because of the ability to assess dimensionality, item difficulty and fit, and item and person reliability and separation.
These results suggest the existence of two subscales in this measure, one assessing transportation barriers in general (subscale 1: general transportation barriers), and another assessing transportation barriers specific to use of public transit (subscale 2: public transit barriers). This measure may be useful in identifying potential transportation barriers among patients and in understanding social factors impacting disease and medication management. In particular, items 2 (how much trouble is it for you to get transportation to your primary care doctor) and 4 (how long does it usually take you to get to your primary care doctor) in the general transportation barriers subscale may be more useful in screening individuals for transportation problems, as they represent the two items with the lowest difficulty levels and can be used regardless of the specific transportation method utilized. There was less variability for questions that address being late to or missing appointments (items 5 and 6, respectively), and delaying scheduling appointments (item 3). These latter items may reflect different, more extreme transportation barriers. The public transit barriers subscale could then also be used to explore barriers in this at-risk group among respondents who report using public transportation. Because all but one item on this subscale uses a yes/no format, the addition of this subscale should not impact respondent burden.
In general, both subscales functioned similarly across multiple participant groups; differences, when present, were minor and would have little practical impact on scores. This preliminary study also suggests the measure functions similarly regardless of whether it is given in English or Spanish, although more research is needed with a larger group of Spanish-speaking participants to determine if there are reliable language effects.
Currently, there are no items directly relevant to individuals who drive or receive a ride, as these items had very low correlations with other items from the general transportation barriers subscale. There are also no items relevant to individuals who walk or utilize subsidized medical transportation services. One possibility is to construct a general question about cost of transportation as a barrier (which was the subject of 8b, and 8c in Subscale 2). This item may fit best in the general transportation barriers subscale. However, the present results suggest that public transit poses unique barriers, necessitating a separate subscale. This subscale demonstrated excellent person reliability and separation, excellent item reliability and separation, and high item point-measure correlations.
The transportation barriers scale incorporates a number of personal, social, and environmental issues that influence transportation availability and impact on health care in more complex ways. A number of enabling factors include ability to walk, vehicle ownership, income, insurance (particularly for subsidized travel), and geographic location. Other factors that may contribute to variance in travel impact include disability, lack of social support, and limited organizational skills. There is likely a greater experience of transportation barriers among those who are dependent on others for travel and have fewer resources. For those individuals, the relationship between barriers and healthcare access or pharmacy use may be more pronounced.
The relationship between transportation barriers to access pharmacy services is largely unexplored in the literature. From a clinical standpoint, separating items related to pharmacy access may be desirable because they would not be applicable to everyone. Many patients with chronic diseases receive their medications through mail-order pharmacies limiting the need for pharmacy visits. For those who do fill their medications in a community pharmacy, transportation issues may be less of a problem because they may have more options for selecting a pharmacy than they do for selecting a healthcare provider. They may be able to select a pharmacy with operational hours that work with their access to transportation or the distance to the pharmacy may be significantly less. There is evidence suggesting that neighborhoods with higher concentrations of ethnic minorities have fewer pharmacies (Qato, Daviglus, Wilder, Lee, Qato, Lambert, 2014) however, the impact on actual possession of medication may not be impacted.(Syed, Sharp, Kim, Jentleson, Lora, Touchette, Berbaum, Suda, Gerber 2016) At this time, additional research is needed to fully understand the role of transportation barriers to accessing medications that are filled in pharmacies.
It is important to highlight that if transportation barriers are identified within the healthcare setting or with pharmacy access, there is an opportunity for intervention. Evidence from patient navigation interventions within the context of cancer treatment show that vouchers, arranged transportation, or assistance with rescheduling appointments during times when transportation is available are effective solutions (Ramirez et al., 2014; Tejeda et al., 2013). Although addressing the lack of transportation to healthcare visits on a larger scale would require policy changes or individual practice-level changes, in certain situations this may be cost effective.
Limitations
All participants were either adult African-American or Hispanic with poorly controlled type 2 diabetes. They were recruited from within different clinics that were part of one healthcare system. The healthcare system cared for predominantly lower income, ethnic minority patients who resided in a large urban city. As such, they had access to a large public transit system. Only 40% of the sample reported experiencing any transportation problems. These characteristics of our sample likely limit the generalizability of the results. The transportation barriers faced by those residing outside of a large urban area certainly differ. Our analyses rely upon self-report data which is vulnerable to recall bias. Additionally, certain types of validity could not be assessed in the present study. Additional assessment of the items in other populations with different characteristics is needed to refine the measure.
Validity is a complicated issue, related not to the test itself but rather to the context in which the test is administered and scored, and the persons responding (Messick, 1995). Though other types of validity (e.g., internal, external) are often maximized through research design, examining construct validity is an iterative process (Cherryholmes, 1988). However, in contrast to the classical test theory approach, the Rasch approach establishes a situation that allows the items to be evaluated by the respondents as much as respondents are evaluated by the items (Fisher, 1991), and various statistics provided through Rasch analysis (e.g., item fit) allow for the identification and removal of poor-performing items that damage construct validity. Rasch measurement theory allows researchers to address many of the validity issues outlined in Smith (2001), including content validity, substantive validity, structural validity, and interpretability.
Future research on this topic should assess external validity of the measure. For instance, items must be tested among different individuals and/or at different time points to assess the generalizability of the item difficulties. External criteria related to transportation barriers, such as frequencies of missed appointments or arriving late for appointments, and other relevant red flags, could be used in future research to assess consequential validity, or the degree to which person measures are valid reflections of person ability (Smith, 2001).
Conclusions
The final measure contains two subscales, one measuring general transportation barriers (6 items), and another measuring barriers specific to utilizing public transportation (5 items). In general, both subscales functioned similarly across multiple participant groups; differences, when present, were minor and would have little practical impact on scores. This preliminary study also suggests that this measure functions similarly regardless of whether it is given in English or Spanish, although more research is needed with a larger group of Spanish-speaking participants to determine if there are reliable language effects.
To date, this is among the most scientifically rigorous published research on the measurement of health-related transportation barriers. This work fills a gap in the literature which has relied largely upon individual items or group of items that have been adopted with little or no psychometric understanding. Assuming the psychometric properties of this measure are supported in future studies, this measure could provide a standardized tool for accurately comparing the impact of transportation barriers on health care outcomes as well as potentially targeting interventions to support patients’ needs.
Table 2.
Demographic Characteristic of the Sample (N=244)
| N (%) | |
|---|---|
| Sex | |
| Female | 164 (67.2) |
| Male | 80 (32.8) |
| Race/Ethnicity | |
| African American/Black | 179 (73.4) |
| Hispanic/Latino | 65 (26.6) |
| Marital Status | |
| Single, never married | 104 (42.6) |
| Married or living with partner | 70 (28.7) |
| Widowed/Separated/Divorced | 70 (28.7) |
| Income Level | |
| < $10,000 | 86 (41.4) |
| $10,000-$19,999 | 56 (26.9) |
| $20,000-$29,999 | 16 (7.7) |
| $30,000+ | 50 (20.5) |
| Highest Education Level | |
| Less than high school | 72 (29.5) |
| High school Diploma/GED | 117 (48.0) |
| Any College | 55 (22.6) |
| Employment Status | |
| Employed | 53 (21.8) |
| Unemployed | 190 (78.2) |
| Health Insurance | |
| None | 13 (5.4) |
| Public Aid/Medicaid | 138 (57.3) |
| Medicare | 47 (19.5) |
| HMO/PPO | 43 (17.8) |
| Health Status | |
| Excellent, Very Good, Good | 96 (39.3) |
| Fair/Poor | 148 (60.6) |
| Age | |
| <40 | 29 (11.9) |
| 40–49 | 48 (19.7) |
| 50–59 | 91 (37.3) |
| 60–69 | 60 (24.6) |
| >=70 | 16 (6.6) |
| Mean (SD) | 48.8 (13.0) |
Acknowledgments
Funding. This project was supported by the University of Illinois at Chicago (UIC) Center for Clinical and Translational Science (CCTS), Award Number UL1RR029879 from the National Center For Research Resources and by the National Institute of Diabetes and Digestive and Kidney Diseases grant number R01DK091347. The views expressed in this manuscript are the authors’ and do not necessarily represent the views of the Department of Veterans Affairs or United States Government.
Appendix 1. Items on the Transportation Barriers Measure (Items in BOLD were included in the Rasch analyses)
TS1. When you visit your primary care doctor at (UIC/Mile Square), how do you usually get there?
| Bus | ……………………………0 |
| Drive – myself | ……………………………1 |
| Drive – someone else drives me | ……………………………2 |
| L train | ……………………………3 |
| Taxi | ……………………………4 |
| Walk | ……………………………5 |
| Other (specify) _____________ | ……………………………6 |
TS2. On a scale of 1-4, how much trouble is it for you to get transportation to your primary care doctor at (UIC/Mile Square)?
1= No trouble; 2= A little trouble; 3= Some trouble; 4=A lot of trouble
TS3. Do you ever delay scheduling a primary care doctor’s appointment because transportation is too much trouble?
0 = No; 1 = Yes
TS4. How long does it usually take you to get from where you live to your primary care doctor at (UIC/Mile Square)?
0 = More than 120 minutes (more than 2 hours)
1 = Between 60 and 120 minutes (between 1 and 2 hours)
2 = Between 30 and 59 minutes
3 = Less than 30 minutes
TS5. Have you ever been more than 20 minutes late to a doctor’s appointment because of transportation problems?
0 = No; 1 = Yes
(If yes) What were the transportation problems? ________________________________________________________________________
TS6. Have you ever missed a doctor’s appointment because of transportation problems?
0 = No; 1 = Yes
(If yes) What were the transportation problems? ________________________________________________________________________
TS7. (If patient has transportation problems continue with question, otherwise skip to number 8)
Think of the last time when a transportation problem made it hard to get to your primary care doctor at (UIC/Mile Square). What happened? ________________________________________________________________________
TS8. (If patient walks, skip to number 9)
You said you usually get to your primary care doctor by (fill in with answer from question number 1).
(If patient has someone else drive them)
a. Does not having a ride to the doctor ever prevent you from seeing your primary care doctor?
0 = No; 1 = Yes
Recode:
Never (all who did not select someone else drives in 1)
No (same as original question)
Yes (same as original question)
(If patient drives him/herself)
b. Does the cost of gasoline for your car ever prevent you from seeing your primary care doctor?
0 = No; 1 = Yes
Recode:
Never (all who did not select drives self in 1)
No (same as original question)
Yes (same as original question)
(If patient takes public transportation/taxi)
c. Does the cost of public transportation/taxi ever prevent you from seeing your primary care doctor?
0 = No; 1 = Yes
Recode:
Never (all who did not select bus/L or taxi in 1)
No (same as original question)
Yes (same as original question)
d. How much does it cost you to get to your primary care doctor at (UIC/Mile Square) and then back to your house (round trip cost)?
__________________________________________________
(If patient takes public transportation, continue on to next question. If patient only takes a taxi, skip to number 9).
e. Think about the distance from your house to the transit stop. Does this distance ever prevent you from going to your primary care doctor because it is too far to walk?
0 = No; 1 = Yes
Recode:
Never (all who did not select bus/L in 1)
No (same as original question)
Yes (same as original question)
f. Do too many transfers on public transportation ever prevent you from going to your primary care doctor?
0 = No; 1 = Yes
Recode:
Never (all who did not select bus/L in 1)
No (same as original question)
Yes (same as original question)
g. How safe do you usually feel when using public transit to get to the doctor?
0 Very safe 1 Somewhat safe 2 Not safe
Recode:
No safety issues (all who did not select bus/L in 1)
Very safe (same as original question)
Somewhat safe (same as original question)
Not safe (same as original question)
h. Do you feel you have any physical disabilities that make it difficult for you to use public transportation to get to the doctor?
0 = No; 1 = Yes
Recode:
Never (all who did not select bus/L in 1)
No (same as original question)
Yes (same as original question)
The following questions are about the pharmacy you use to get your medications.
TS9. People often run out of medicine before they get their prescription refilled. There are many reasons for this. One reason is that they do not have a way to get to the pharmacy. Have you ever run out of medicines because you could not find a way to get to the pharmacy to pick up your refill of medicines?
0 = No; 1 = Yes
a. (If yes)What were the transportation problems? ________________________________________________________________________
b. (If yes) How often does this happen?
| Rarely | ……………………………0 |
| Sometimes | ……………………………1 |
| Often | ……………………………2 |
| All the time | ……………………………3 |
Recode (for new Q9):
Never (all who said no to TS9)
Rarely (same as original question)
Sometimes (same as original question)
Often (same as original question)
All the time (same as original question)
TS10. If you have any transportation problems, what would help fix them? ________________________________________________________________________
Contributor Information
Sara M. Locatelli, Department of Veterans Affairs, Hines VA Hospital, Health Services Research & Development, 5000 S. 5th Avenue (Mailcode 151H), Hines, IL USA 60141, Phone: 708-202-4558.
Lisa K. Sharp, Pharmacy Systems, Outcomes, & Policy, College of Pharmacy, University of Illinois at Chicago, 833 S. Wood Street M/C 871, Chicago, IL 60612, Phone: 312-355-3569.
Samina T. Syed, Section of Endocrinology, Diabetes and Metabolism, University of Illinois at Chicago, 1819 W. Polk Street, M/C 640, Chicago, IL 60612.
Shikhi Bhansari, Institute for Health Research and Policy M/C 275, University of Illinois at Chicago, 1747 West Roosevelt Road, Chicago, IL 60608.
Ben S. Gerber, Division of Academic Internal Medicine and Geriatrics, Institute for Health Research and Policy M/C 275, University of Illinois at Chicago, 1747 West Roosevelt Road, Chicago, IL 60608, Phone: 312-996-8872.
References
- Andrich D. A rating formulation for ordered response categories. Psychometrika. 1978;43:357–374. doi: 0.1007/BF02293814. [Google Scholar]
- Bode RK. Partial credit model and pivot anchoring. In: Smith EV Jr, Smith RM, editors. Introduction to Rasch measurement. Maple Grove, MN: JAM Press; 2004. pp. 279–295. [PubMed] [Google Scholar]
- Bond TG, Fox CM. Applying the Rasch model: Fundamental measurement in the human sciences. 2nd. New York, NY: Routledge; 2007. [Google Scholar]
- Fischer GH. On the existence and uniqueness of maximum-likelihood estimates in the Rasch model. Psychometrika. 1981;46:59–77. doi: 10.1007/BF02293919. [DOI] [Google Scholar]
- Fisher WP., Jr . The Rasch debate: Validity and revolution in educational measurement. In: Wilson M, editor. Objective measurement: Theory into practice. Vol. 2. Norwood: Ablex Publishing Corporation; 1994. pp. 36–72. [Google Scholar]
- Gerber BS, Rapacki L, Castillo A, Tilton J, Touchette DR, Milhailescu D, Berbaum ML, Sharp LK. Design of a trial to evaluate the impact of clinical pharmacists and community health promotors working with African-Americans and Latinos with Diabetes. BMC Public Health. 2012;12:891. doi: 10.1186/1471-2458-12-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Education and Counseling. 2005;57:300–307. doi: 10.1016/j.pec.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Lai JS, Teresi J, Gershon R. Procedures for the analysis of Differential Item Function (DIF) for small sample sizes. Evaluation and the Health Professions. 2005;28:283–294. doi: 10.1177/0163278705278276. [DOI] [PubMed] [Google Scholar]
- Linacre JM. Comparing “partial credit models” (PCM) and “rating scale models” (RSM) Rasch Measurement Transactions. 2000;14:768. [Google Scholar]
- Linacre JM. Data variance explained by Rasch measures. Rasch Measurement Transactions. 2006;20:1045. [Google Scholar]
- Linacre JM. KR-20/Cronbach alpha or Rasch person reliability: Which tells the “truth”? Rasch Measurement Transactions. 1997;11:580–581. [Google Scholar]
- Linacre JM. Optimizing rating scale category effectiveness. Journal of Applied Measurement. 2002;3:85–106. [PubMed] [Google Scholar]
- Linacre JM. When to stop removing items and persons in Rasch misfit analysis? Rasch Measurement Transactions. 2010;23:1241. [Google Scholar]
- Linacre JM. Winsteps ® (Version 3.74.0) [Computer Software] Beaverton, OR: 2012. Winsteps.com. [Google Scholar]
- Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B. ‘Pharmacy deserts’ are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Aff (Millwood) 2014 Nov;33(11):1958–65. doi: 10.1377/hlthaff.2013.1397. 2014. [DOI] [PubMed] [Google Scholar]
- Ramirez A, Perez-Stable E, Penedo F, Talavera G, Carrillo JE, Fernandez M, Holden A, Munoz E, San Miguel S, Gallion K. Reducing time-to-treat in underserved Latinas with breast cancer. Cancer. 2014;120(5):752–60. doi: 10.1002/cncr.28450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasch G. Probabilistic models for some intelligence and attainment tests. Chicago, IL: MESA Press; 1993. (Original work published 1960) [Google Scholar]
- Ruxton GD. The unequal variance t-test is an under used alternative to Student’s t-test and the Mann-Whitney U test. Behavior Ecology. 2006;17:688–690. doi: 10.1093/beheco/ark016. [DOI] [Google Scholar]
- Smith EV., Jr Evidence for the reliability of measures and validity of measure interpretation: A Rasch measurement perspective. Journal of Applied Measurement. 2001;2:281–311. [PubMed] [Google Scholar]
- Smith EV., Jr . Detecting and evaluating the impact of multidimensionality using item fit statistics and principal components analysis of residuals. In: Smith EV, Smith RM, editors. Introduction to Rasch measurement: Theory, models, and applications. Maple Grove, MN: JAM Press; 2004. pp. 575–600. [PubMed] [Google Scholar]
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. Journal of Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed ST, Sharp LK, Kim Y, Jentleson A, Lora CM, Touchette DR, Berbaum ML, Suda KJ, Gerber BS. Relationship Between Medication Adherence and Distance to Dispensing Pharmacies and Prescribers Among an Urban Medicaid Population with Diabetes Mellitus. Pharmacotherapy. 2016 Jun;36(6):590–7. doi: 10.1002/phar.1757. 2016. Epub 2016 May 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejeda S, Darnell JS, Cho YI, Stolley MR, Markossian TW, Calhoun EA. Patient barriers to follow-up care for breast and cervical cancer abnormalities. Journal of Women’s Health. 2013;22(6):507–17. doi: 10.1089/jwh.2012.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Preventing Chronic Disease. 2014;11:130389. doi: 10.5888/pcd11.130389. http://dx.doi.org/10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner SJ, Schwartz A, Yudkowsky R, Schiff GD, Weaver FM, Goldberg J, Weiss KB. Evaluating physician performance at individualizing care: A pilot study tracking conceptual errors in medical decision making. Medical Decision Making. 2007;27:726–734. doi: 10.1177/0272989X07306113. [DOI] [PubMed] [Google Scholar]
- Wheaton B, Muthen B, Alwin DF, Summers G. Assessing reliability and stability in panel models. Sociological Methodology. 1977;8:84–136. [Google Scholar]
- Wright BD. Reliability and separation. Rasch Measurement Transactions. 1996;9:472. [Google Scholar]
- Wright BD, Mok MMC. An overview of the family of Rasch measurement models. In: Smith EV, Smith RM, editors. Introduction to Rasch measurement: Theory, models, and applications. Maple Grove, MN: JAM Press; 2004. pp. 1–24. [Google Scholar]
- Wright BD, Panchapakesan N. A procedure for sample-free item analysis. Educational Psychology Measurement. 1969;29:23–48. [Google Scholar]
- Wright BD, Stone MH. Best test design. Chicago: MESA Press; 1979. [Google Scholar]


