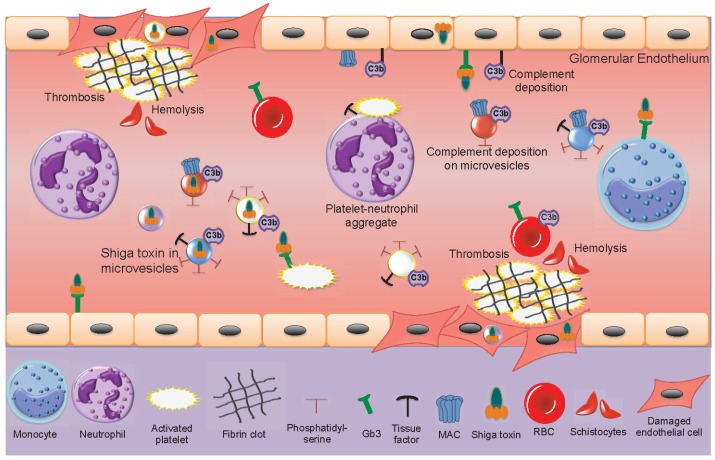
Figure 3.
Shiga toxin-induced activation of blood cells and damage to the glomerular endothelium. Within the bloodstream Shiga toxin can bind to monocytes, neutrophils, activated platelets and red blood cells. Aggregates are formed between platelets and leukocytes (depicted in the figure between a neutrophil and a platelet). Microvesicles are shed from blood cells (neutrophils, monocytes, platelets and red blood cells). Some of these contain the toxin. All these microvesicles may expose phosphatidylserine. Microvesicles from platelets and monocytes expose tissue factor. Complement may deposit on platelet, monocyte and red blood cell-derived microvesicles, as well as on the glomerular endothelium. Shiga toxin binds to glomerular endothelial cells via the Gb3 glycolipid receptor or undergoes endocytosis within blood cell-derived microvesicles. Shiga toxin-induced cytotoxicity and complement deposition lead to glomerular endothelial cell damage. Thrombosis is induced by toxin-mediated endothelial cell damage, platelet activation and the pro-thrombotic effects of microvesicles. Hemolysis is induced by mechanical breakdown of red blood cells in occluded capillaries as well as by complement deposition on red blood cells. Fragmented red blood cells are termed schistocytes. Gb3: globotriaosylceramide, MAC: membrane attack complex (C5b-9), RBC: red blood cell.