Abstract
Objectives
To determine whether the Child Opportunity Index (COI), a nationally-available measure of relative educational, health/environmental, and social/economic opportunity across census tracts within metropolitan areas, was associated with population- and patient-level asthma morbidity.
Study design
This population-based retrospective cohort study was conducted between 2011–2013 in 1 Southwest Ohio county. Participants included all children, 1–16 years, with hospitalizations or emergency department visits for asthma or wheezing at a major pediatric hospital. Patients were identified using discharge diagnosis codes and geocoded to their home census tract. The primary population-level outcome was census tract asthma hospitalization rate. The primary patient-level outcome was re-hospitalization within 12 months of index hospitalization. Census tract opportunity was characterized using the COI and its educational, health/environmental, and social/economic domains.
Results
Across 222 in-county census tracts, there were 2,539 geocoded hospitalizations. The median asthma-related hospitalization rate was 5.0 per 1,000 children per year (interquartile range: 1.9–8.9). Median hospitalization rates in very low, low, moderate, high, and very high opportunity tracts were 9.1, 7.6, 4.6, 2.1, and 1.8 per 1,000, respectively (P < .0001). The social/economic domain had the most variables significantly associated with the outcome at the population level.
The adjusted patient-level analyses showed that the COI was not significantly associated with a patient’s risk of re-hospitalization within 12 months.
Conclusions
The Child Opportunity Index was associated with population-level asthma morbidity. The detail provided by the COI may inform interventions aimed at increasing opportunity and reducing morbidity across regions.
Keywords: Asthma, Pediatrics, Social Determinants of Health
Asthma affects ~7 million American children and is among the most common reasons children are hospitalized.(1) Asthma-related morbidity disproportionately affects racial minorities and the socioeconomically disadvantaged.(1–3) Marked disparities exist across regions with considerable neighborhood-to-neighborhood variability.(4) At the population level, areas with high rates of poverty, substandard housing, and crime have high rates of asthma morbidity.(5–9) At the patient level, influential factors may include socioeconomic status, culture, ethnicity, health beliefs, and gene-environment interactions.(3, 5, 10–12) Factors related to these social determinants of health (SDH) play an undeniable role at both levels.(5)
Current research in population health has been limited by existing measures and the lack of an organizing framework. Certain area-level measures of the SDH, including the percentage of individuals below the federal poverty level, are widely available and have shown value in characterizing inequities;(9, 13) however, such measures are crude and may not be amenable to immediate action. Other measures related to housing or crime(7, 8) provide nuanced, potentially-actionable detail but are typically local. There is a need for more generalizable measures with which to examine root causes and the broader context of inequities.(5) Analyses could benefit from the organizing framework introduced by Wise et al, which assesses differential presence of risk (negative factors) and access (positive factors) across populations.(14) Identification of generalizable, actionable measures, and combinations of measures, within this framework would be a major step forward in understanding, tracking, and responding to the inequitable distribution of many disease outcomes, including asthma.
The Child Opportunity Index (COI) may reflect needed progress. The COI, crafted by diversitydatakids.org in collaboration with the Kirwan Institute, defines “opportunity” as “neighborhood-based conditions and resources conducive to healthy child development.”(15) This publically-available and easily-accessible index includes a range of measures, enumerating relative opportunity in educational, health and environmental, and social and economic domains across all census tracts within metropolitan areas.(16, 17) Though the index has been previously linked to life expectancy, low birth weight, and preterm birth,(15) it has not yet been linked to asthma morbidity. Establishing such a link could provide a more informed approach to identifying and addressing potentially-correctable inequities across or within metropolitan areas. Here, we hypothesize that those tracts with less “opportunity” would be more likely to experience excess morbidity. In testing this hypothesis, we sought, first, to determine whether census tract opportunity would be associated with census tract rates of acute asthma morbidity, defined using hospital data on all asthma-related emergency department (ED) visits and hospitalizations. Our second objective was to determine whether COI measures for the tract where a hospitalized child lives would be associated with that child’s risk of asthma-related re-hospitalization. For both population- and patient-level analyses, we also sought to evaluate individual measures comprising the COI and their associations with asthma-related morbidity.
METHODS
We pursued an ecological study using a retrospective cohort of 5,462 children, aged 1–16 years, living within Hamilton County, Ohio. Children were eligible for inclusion if they were hospitalized or visited the emergency department (ED) for asthma or wheezing at Cincinnati Children’s Hospital Medical Center (CCHMC) between January 2011 and December 2013. We excluded those children >16 years as they are more likely to visit other area EDs and hospitals. We opted to include children aged 1–2 years given their high rates of emergency and hospital utilization; however, given diagnostic uncertainty around this age group, we pursued sensitivity analyses after their exclusion. All patients were identified using an asthma-specific encounter diagnosis (International Classification of Diseases, 9th Revision, Clinical Modification, 493.XX) within hospital billing data. The street address for each patient’s utilization event was geocoded and mapped to an in-county census tract. Children (and utilization events) were excluded from our analyses if the associated address was unable to be geocoded.
Population-level analyses focused on the utilization events these children contributed. Patient-level analyses focused on unique, geocoded patients who were hospitalized during the study period. Each patient had ≥12 months of follow up time available to determine if they experienced an asthma-related re-hospitalization.
Hamilton County, the location of metropolitan Cincinnati, contains 222 census tracts and 167,659 children aged 1–16 years.(18) Although the COI provides data for an area larger than Hamilton County,(16) we used just in-county utilization data because CCHMC manages ~95% of all in-county asthma-related hospitalizations and fewer outside the county.(2)
Outcomes and predictors
Our primary population-level outcome was an annualized asthma-related hospitalization rate calculated for each census tract by dividing all hospitalizations occurring within a specific tract by the total number of children, aged 1–16 years, living within that tract.(7, 8) The calculation yielded an annual hospitalization rate measured per 1,000 children per year. We calculated a total utilization rate (all hospitalizations plus all ED visits) in the same manner.
Patient-level outcomes were determined for children who had an index hospitalization at any point between 2011 and 2013. Each child was then followed for at least 12 months to establish whether or not they had an asthma-related re-hospitalization. Re-hospitalizations were captured the same way as the index hospitalization.
The COI provided predictors for both population- and patient-level analyses. The Index includes 19 variables across three domains specific to educational, health and environmental, and social and economic opportunities, conditions, and resources.(15) Z-scores are calculated and standardized for the metropolitan area based on the distribution of the variables within that area – these Z-scores enumerate the number of standard deviations that census tract’s variable (or domain) is from the region’s mean tract. The Z-scores allow for analyses of within-region variation with respect to each variable, each domain, and for the COI as a whole. To categorize opportunity measures, census tracts are placed into quintiles (very low, low, moderate, high, and very high opportunity) based on their overall scores and their three domain scores. Distributions for each individual variable can also be assessed on a continuous scale. As ~20% of our included tracts were within each quintile, we did not alter the Z-scores that had been calculated for all the entire metropolitan area that included some tracts outside of Hamilton County.
For population-level analyses, our primary predictor was the composite opportunity measure, here termed Overall COI (OCOI). We also assessed the categorized domain-specific measures: educational (EOI), health and environmental (HEOI), and social and economic opportunity (SEOI). The continuous distributions for each individual variable were also assessed.
For patient-level analyses, we used the categorized measures of opportunity; however, we narrowed the OCOI, EOI, HEOI, and SEOI categories considering how they could be more clinically useful. Here, opportunity categories were defined as very low-low, moderate, and high-very high. We again examined each individual variable on a continuous scale.
Covariates
Given the breadth of area-level variables included in the COI, we did not use additional area-level covariates. At the patient-level, we extracted child age at the index admission, sex, race/ethnicity, and insurance from the health record. We treated age as a continuous variable. We categorized race/ethnicity as white/non-Hispanic, African American/non-Hispanic, Hispanic, or other. We defined insurance as private or public. Unknown data were treated as missing.
Statistical Analyses
We first mapped all utilization events and linked each to the composite opportunity measure (OCOI) by census tract. We then used descriptive statistics to characterize key population- and patient-level variables using frequencies for categorical variables and distributions (including medians and interquartile ranges [IQR]) for continuous variables.
We used the Kruskal-Wallis test to assess for bivariate associations between each categorized opportunity measure and population-level asthma outcomes. Next, we assessed the association between each of the continuous Z-scores for the 19 COI variables and our asthma outcomes using LOESS regression. Parameter estimates >1.96 or <−1.96 were considered statistically significant at the p<0.05 level. We used this method because it is robust to extreme, skewed outcome values – here, asthma hospitalization rates that were not normally distributed. It also yields a visual display of potential non-linear relationships between outcome and predictor.
We assessed patient-level associations between categorized opportunity (overall and within domains) and both covariates and outcomes using the Chi square test for categorical variables and the Wilcoxon Rank Sum test for continuous variables. We used the Mantel-Haenszel Chi square test of trend in the bivariate assessment of opportunity and patient-level re-hospitalization. We then built multivariable logistic regression models to adjust for patient age, race/ethnicity, and insurance. The race/ethnicity and insurance covariates were added in a step-wise fashion so as ensure that models were not over-fit. Given the low numbers of reutilization events within certain tracts, we did not pursue hierarchical regression; instead, we assigned census tract data to individuals based on their home street address. Finally, we explored bivariate relationships between each individual COI variable and a patient’s risk of re-hospitalization within 12 months.
Geocoding and mapping were pursued using ArcGIS (version 10.1, Redlands, California). Statistical analyses were performed using SAS (version 9.3, Cary, North Carolina). This study was approved by the CCHMC Institutional Review Board.
RESULTS
Between January 1, 2011 and December 31, 2013, the 222 Hamilton County census tracts contained a total of 9,425 successfully geocoded utilization events; 2,539 were hospitalizations (geocode rate of ~95%). The median asthma hospitalization rate across the tracts was 5.0 hospitalization events per 1,000 children per year (IQR 1.9–8.9) (Table I). The median utilization rate was 19.0 hospitalizations and ED visits per 1,000 children per year (IQR 8.6–29.8). Approximately 20% of tracts were within each COI category.
A total of 1,932 unique patients had ≥1 hospitalization during the study period; 1,845 were successfully geocoded (>95%). These patients had a median age, at their index visit, of 4.7 years (IQR 2.5–8.3). They were predominantly male, African American/non-Hispanic, and publicly-insured (Table 1). More than 60% lived in very low or low overall opportunity tracts.
Table 1.
Population-level characteristics for included census tracts (n=222 census tracts) and patient-level characteristics for those patients contributing hospitalization events (n=1,932 patients)
| N (or median) | % (or IQR) | |
|---|---|---|
| Population-level characteristics (n=222 census tracts) | ||
| Asthma hospitalization rate (events per 1,000 children per year) | 5.0 | 1.9, 8.9 |
| Asthma hospitalization + emergency department utilization rate (events per 1,000 children per year) | 19.0 | 8.6, 29.8 |
| Overall Child Opportunity Index Categories (OCOI) | ||
| Very low | 53 | 23.9 |
| Low | 39 | 17.6 |
| Moderate | 42 | 18.9 |
| High | 41 | 18.5 |
| Very high | 47 | 21.2 |
| Educational Opportunity Index Categories (EOI) | ||
| Very low | 55 | 24.8 |
| Low | 49 | 22.1 |
| Moderate | 42 | 18.9 |
| High | 39 | 17.6 |
| Very high | 37 | 16.7 |
| Health & Environmental Opportunity Index Categories (HEOI) | ||
| Very low | 40 | 18.0 |
| Low | 44 | 19.8 |
| Moderate | 40 | 18.0 |
| High | 40 | 18.0 |
| Very high | 58 | 26.1 |
| Social & Economic Opportunity Index Categories (SEOI) | ||
| Very low | 56 | 25.2 |
| Low | 34 | 15.3 |
| Moderate | 41 | 18.5 |
| High | 44 | 19.8 |
| Very high | 47 | 21.2 |
| Patient-level characteristics (n=1,932 patients with index hospitalization)* | ||
| Age | 4.7 | 2.5, 8.3 |
| Male sex | 1,209 | 62.6 |
| Race/Ethnicity | ||
| White/Non-Hispanic | 490 | 25.8 |
| African American/Non-Hispanic | 1,278 | 67.4 |
| Hispanic | 77 | 4.1 |
| Other | 52 | 2.7 |
| Insurance | ||
| Private | 473 | 24.9 |
| Public | 1,428 | 75.1 |
| Child Opportunity Index (COI) | ||
| Overall Child Opportunity Index Categories (OCOI) | ||
| Very low or Low | 1,174 | 63.6 |
| Moderate | 307 | 16.6 |
| High or Very High | 364 | 19.7 |
| Educational Opportunity Index Categories (EOI) | ||
| Very low or Low | 1,208 | 65.5 |
| Moderate | 276 | 15.0 |
| High or Very High | 361 | 19.6 |
| Health & Environmental Opportunity Index Categories (HEOI) | ||
| Very low or Low | 980 | 53.1 |
| Moderate | 296 | 16.0 |
| High or Very High | 569 | 30.8 |
| Social & Economic Opportunity Index Categories (SEOI) | ||
| Very low or Low | 1,153 | 62.5 |
| Moderate | 285 | 15.5 |
| High or Very High | 407 | 22.1 |
| Re-hospitalization experienced within 12 months of index visit | 411 | 21.3 |
Abbreviations: COI – Child Opportunity Index; OCOI – Overall Child Opportunity Index Categories; EOI – Educational Opportunity Index Categories; HEOI – Health & Environmental Opportunity Index Categories; SEOI – Social & Economic Opportunity Index Categories
Missing data: 35 patients did not have available race/ethnicity information; 31 patients did not have available insurance information; 87 patients were not able to be successfully geocoded and were therefore unable to be grouped into opportunity categories.
Population-level analyses
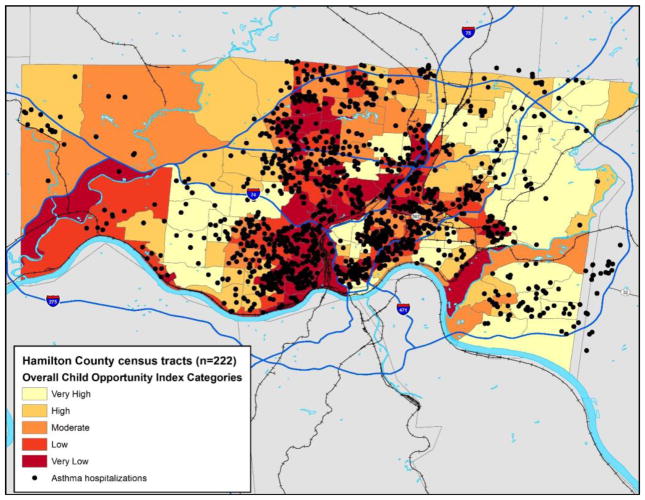
The mapped hospitalization events were well-distributed across Hamilton County but appeared to cluster in tracts with very low and low OCOI (Figure 1; available at www.jpeds.com). This finding was confirmed quantitatively. Both hospitalization and utilization rates varied in a graded fashion across OCOI categories and within each domain (Table 2). For example, the median hospitalization rate in very low overall opportunity tracts was 9.12 hospitalizations per 1,000 children per year. This rate was compared to 7.61 per 1,000 children per year in the low, 4.60 in the moderate, 2.09 in the high, and 1.77 in the very high opportunity tracts (p<0.0001). While 21% of the entire child population lived in very low opportunity tracts, they contributed 41% of all hospitalizations; 26% of the population lived in very high opportunity tracts but contributed just 10% of hospitalizations. These same gradations were seen within each of the EOI, HEOI, and SEOI domains (all p<0.0001) and for our utilization rate measure (overall and each domain, all p<0.0001).
Figure 1.
online only: Map of Hamilton County, Ohio including the Overall Child Opportunity Index Categories for each of the 222 included census tracts. The map also depicts all in-county hospitalizations occurring during the 2011–2013 study period.
Table 2.
Distribution of asthma-related hospitalizations and utilization events across the Child Opportunity Index (COI) Categories*
| Median hospitalization rate (events per 1,000 children per year) (IQR) | Median utilization rate (events per 1,000 children per year) (IQR) | |
|---|---|---|
| Overall Child Opportunity Index Categories (OCOI) | ||
| Very low | 9.12 (6.84, 11.72) | 31.82 (24.89, 46.07) |
| Low | 7.61 (4.88, 10.03) | 26.97 (14.91, 34.18) |
| Moderate | 4.60 (2.55, 6.39) | 18.31 (11.73, 23.07) |
| High | 2.09 (0.94, 3.65) | 10.19 (5.47, 15.59) |
| Very high | 1.77 (0.80, 2.82) | 6.36 (3.31, 12.92) |
| Educational Opportunity Index Categories (EOI) | ||
| Very low | 8.14 (6.50, 10.43) | 29.30 (23.15, 35.55) |
| Low | 6.84 (4.88, 11.67) | 24.64 (19.05, 36.32) |
| Moderate | 3.70 (1.87, 6.64) | 15.98 (10.03, 21.13) |
| High | 2.24 (0.97, 3.30) | 8.46 (4.26, 14.46) |
| Very high | 1.79 (0.87, 3.37) | 6.26 (3.50, 12.92) |
| Health & Environmental Opportunity Index Categories (HEOI) | ||
| Very low | 9.10 (6.35, 11.71) | 30.63 (20.15, 44.41) |
| Low | 7.55 (3.71, 9.54) | 27.01 (17.15, 35.25) |
| Moderate | 4.00 (1.93, 6.58) | 14.68 (9.23, 24.13) |
| High | 3.90 (0.91, 6.53) | 15.54 (5.55, 22.71) |
| Very high | 2.55 (1.18, 5.90) | 10.52 (5.67, 19.77) |
| Social & Economic Opportunity Index Categories (SEOI) | ||
| Very low | 9.10 (6.62, 11.25) | 30.73 (24.37, 43.00) |
| Low | 6.67 (4.49, 9.96) | 25.85 (16.78, 32.80) |
| Moderate | 3.61 (1.89, 7.50) | 15.48 (8.23, 26.12) |
| High | 2.80 (1.65, 5.37) | 11.10 (8.10, 19.89) |
| Very high | 1.32 (0.63, 3.30) | 6.26 (3.08, 13.66) |
P-value < 0.0001 as measured by Kruskal Wallis test statistic across tested associations between categorized opportunity measure and both the hospitalization and utilization rate
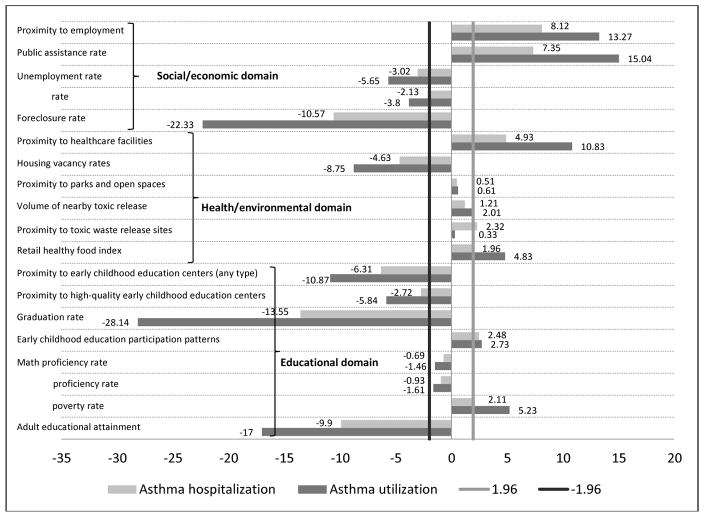
Next, we assessed the 19 individual variables, measured on a continuous scale, and our population-level outcomes. Figure 2 visually depicts parameter estimates for each individual variable and the associations with both the population-level hospitalization rate and the utilization rate. In the educational domain, high school graduation rate was the most strongly associated with both the population-level hospitalization rate (parameter estimate −13.6) and utilization rate (parameter estimate −28.1). In the health and environmental domain, housing vacancy rates were most strongly associated with both outcomes (parameter estimates of −4.6 for the hospitalization rate and −8.8 for the utilization rate). The social and economic domain had the most variables significantly related to our outcomes including rates of foreclosures, poverty, unemployment, and public assistance, and a measure of proximity to employment. Of all variables assessed, high school graduation rate showed the strongest association with both population-level outcomes.
Figure 2.
Parameter estimates for each of the individual elements composing the Child Opportunity Index measured on a continuous scale in association with asthma hospitalization and utilization rates. Parameter estimates above 1.96 or below −1.96 correspond to a p-value of <0.05
The direction and magnitude of all assessed relationships remained the same after sensitivity analyses were pursued excluding those children aged <2 years.
Patient-level analyses
A total of 21.3% patients with an index hospitalization between 2011 and 2013 were re-hospitalized within 12 months; 22.7% of those with very low-low overall opportunity tracts were re-hospitalized compared to 16.5% of those tracts with high-very high opportunity (Mantel-Haenszel p=0.01). Similar relationships were seen with EOI (p=0.02) and SEOI (p<0.05) but not for HEOI (p=0.2). Re-hospitalization at 12 months was also significantly associated with patient age, race/ethnicity, and insurance. Adjustment for these covariates eliminated the significance of associations between opportunity and re-hospitalization (Table 3).
Table 3.
Unadjusted and adjusted* associations between categorizes of child opportunity and measures of asthma-related re-hospitalization among those patients with an index hospitalization event
| Re-hospitalization within 12 months of index hospitalization | ||
|---|---|---|
| OR (95% CI) | AOR (95% CI) | |
| Overall Child Opportunity Index Categories (OCOI) | ||
| Very low or Low | 1.49 (1.10, 2.03) | 1.16 (0.81, 1.65) |
| Moderate | 1.36 (0.92, 2.00) | 1.23 (0.82, 1.84) |
| High or Very High | Ref | Ref |
| Educational Opportunity Index Categories (EOI) | ||
| Very low or Low | 1.49 (1.10, 2.04) | 1.18 (0.84, 1.66) |
| Moderate | 1.42 (0.95, 2.12) | 1.24 (0.82, 1.89) |
| High or Very High | Ref | Ref |
| Health & Environmental Opportunity Index Categories (HEOI) | ||
| Very low or Low | 1.16 (0.90, 1.50) | 0.98 (0.75, 1.29) |
| Moderate | 1.03 (0.72, 1.46) | 1.01 (0.71, 1.44) |
| High or Very High | Ref | Ref |
| Social & Economic Opportunity Index Categories (SEOI) | ||
| Very low or Low | 1.30 (0.98, 1.73) | 1.01 (0.73, 1.39) |
| Moderate | 1.06 (0.72, 1.56) | 0.98 (0.66, 1.46) |
| High or Very High | Ref | Ref |
Abbreviations: OR – odds ratio; AOR – adjusted odds ratio; 95% CI – 95% confidence intervals; OCOI – Overall Child Opportunity Index Categories; EOI – Educational Opportunity Index Categories; HEOI – Health & Environmental Opportunity Index Categories; SEOI – Social & Economic Opportunity Index Categories
Adjusted for age, race/ethnicity, and insurance
Finally, we looked at bivariate relationships between each of the 19 COI variables and patient-level re-hospitalization within 12 months. Six variables were significantly related to this patient-level outcome at the p<0.05 level: three within the EOI (adult educational attainment, math proficiency rate, high school graduation rate), two within the HEOI (proximity to parks and open spaces, housing vacancy rates), and one within the SEOI (poverty rate) (data not shown).
As for the population-level analyses, relationships were essentially unchanged when those children <2 years were excluded.
DISCUSSION
The Child Opportunity Index was independently associated with population-level asthma hospitalization and utilization rates. Very low opportunity census tracts experienced more asthma morbidity compared to very high opportunity tracts. Similar, though non-significant relationships, were noted for individual patients and their risk of re-hospitalization within 12 months. Though previous studies have supported the association between area-level measures of the SDH and both population- and patient-level outcomes, the breadth, generalizability, and potential actionability of the COI could have implications for national use in population health efforts.
The associations between a census tract’s degree of opportunity and its rate of asthma-related morbidity help to further characterize disparities previously recognized in our community.(4) Our findings align with Acevedo-Garcia et al.’s suggestion that the COI could have important applications in guiding community development and monitoring health equity.(15) It could also be applied to the evaluation of disparities in ways that facilitate movement from risk characterization to action.(19–21) Tools such as the COI could be key to “moving upstream,” identifying health-relevant, contextual factors that may be modifiable through interventions and polices.(22, 23) For example, with its association with population-level asthma morbidity, the COI may inform the design of census-tract level, asthma-specific interventions (e.g., medication delivery programs, school-based asthma symptom monitoring).(5, 24) The COI could similarly motivate opportunity-enhancing interventions that promote health and well-being in ways that are not directly clinical or condition-specific (e.g., community development programs, connections to community resources like job training programs).(25, 26) Moreover, bringing indices like the COI together with health outcomes could highlight populations and patients at risk for “double jeopardy” – limited opportunity and heightened risk for morbidity.(27)
Communities are complex entities, and the multiple measures and domains of the COI enhance our ability to understand the distribution of risk and access(14) across a region. Previous studies of asthma, including our own, have looked at individual variables in isolation or relatively narrow clusters of variables available nationally (eg, poverty).(9, 28) We have also looked at other locally-available variables, “geomarkers” pertaining to housing code violations and exposure to crime.(7, 8) These data are potentially less useful in other locations while the COI is currently easily accessible and available for census tracts across 100 metropolitan areas.(17) Identifying whether our findings generalize to other municipalities could further support its use across population health efforts.
The COI also shifts attention to opportunity, providing a positive frame through which population health efforts could be designed. If all census tracts in our county had the same asthma hospitalization rate as observed in very high opportunity tracts, nearly 1,600 hospitalizations, >60% of all, would have been prevented during the three-year study period. This potential for reduction in morbidity (and cost) could illuminate ways in which interventions relevant to a census tract’s opportunity deficits could reduce risk and expand access to medical and social services across our region; the COI may inform what interventions are most appropriate in one tract (or neighborhood) compared to another.(14) In our data, there were strong associations between many variables within each of the COI’s domains and asthma outcomes. That being said, there were some variables that seemed less relevant, at least for asthma. Such findings may help to target condition-specific activities. Alternatively, it may be worthwhile to study each individual census tract in more depth, assessing whether certain variables, positive or negative, are of particular relevance to that particular tract. Such a tactic could inform population-based, tract-specific assessments, interventions, or policy changes relevant to expanding opportunity.
Although we found no significant associations between the COI and a patient’s risk of asthma-related re-hospitalization, we suspect that there could still be clinical, patient-level utility for indices such as the COI.(29) This possibility warrants further investigation, especially considering the growing emphasis on identifying and responding to the SDH during patient care.(30) While social risk assessment is increasingly upheld as a critical component of preventive patient care, no singular “right” way to assess (or intervene) has been established.(31, 32) Given these challenges, it is possible that area-based measures or indices could help frame or inform patient-level social histories. We previously showed significant correlations between area-level and family-reported measures of socioeconomic status within a cohort of children hospitalized with asthma.(33) Such area-level data, or “geomarkers,”(8, 29) could inform assessments and target interventions (eg, medication delivery, legal advocacy, care navigation, connection to community resources or agencies) in ways that warrant further evaluation.(20) The domains of the COI could also support the development and ongoing evaluation of cross-sector partnerships.
There were limitations to this study. First, the COI is constructed using Z-scores calculated for specific metropolitan areas. It is not possible to directly compare a census tract within our metropolitan area to one elsewhere.(15) For within-area population health initiatives, or patient-level projects focusing on morbidity reduction, such a limitation is of less importance. Additionally, relative opportunity may be just as, if not more, important than absolute opportunity.(34) Second, our findings illustrate association and not causation; unmeasured confounding may obscure our findings. Third, our asthma utilization data were obtained using billing codes. It is possible that certain utilization events were missed (or included mistakenly) as a result – this may be particularly true for younger patients with a less-certain asthma diagnosis. Still, we expect this to be non-differential across tracts (and patients), and our sensitivity analyses excluding those children <2 years did not meaningfully change our results. Fourth, we acknowledge that asthma-related utilization rates, when divided by all residents, capture both asthma prevalence and severity. It is possible that prevalence differs across census tracts, a reality that could account, in part, for the identified disparities in morbidity.(35) Unfortunately, we are not able, within our data, to examine whether opportunity influences asthma prevalence. Fifth, our patient-level analyses assigned census tract opportunity data to individuals. We expect that census tract sociodemographic homogeneity supports such an assumption. We also used the area-level measure as a predictor of morbidity and not whether that individual does or does not have certain risks or access. Finally, our sample was drawn from a single health system so we cannot account for children seeking care elsewhere. We expect this to be a more relevant limitation to our utilization analyses that included ED visits as these may be more sensitive to differential access to other care locations (e.g., private physician offices). However, local data suggest that our system captures the vast majority of in-county utilization events, including ~95% of all hospitalizations.(2) Relatedly, the demographic characteristics of our region may limit the degree to which our findings generalize to other communities.
Pediatric asthma morbidity is largely driven by contextual factors rooted in the social and environmental determinants of health. We found that the Child Opportunity Index, a multi-dimensional tool using publically-available national datasets, was significantly associated with population-level asthma hospitalization rates. The detail provided by the COI may inform assessments and interventions aimed at increasing opportunity and reducing morbidity in ways that promote equitable outcomes across regions.
Acknowledgments
Supported, in part, through the National Institutes of Health (NIH 1K23AI112916). The authors declare no conflicts of interest.
Abbreviations
- CCHMC
Cincinnati Children’s Hospital Medical Center
- COI
Child Opportunity Index
- ED
emergency department
- EOI
Educational domain of the COI
- HEOI
Health and Environmental domain of the COI
- IQR
interquartile range
- OCOI
Overall COI categories
- SDH
social determinants of health
- SEOI
Social and Economic domain of the COI
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat. 2012;3(35):1–58. [PubMed] [Google Scholar]
- 2.Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133(3):431–9. doi: 10.1542/peds.2013-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck AF, Huang B, Auger KA, Ryan PH, Chen C, Kahn RS. Explaining Racial Disparities in Child Asthma Readmission Using a Causal Inference Approach. JAMA Pediatr. 2016;170(7):695–703. doi: 10.1001/jamapediatrics.2016.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beck AF, Moncrief T, Huang B, Simmons JM, Sauers H, Chen C, et al. Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163(2):574–80. doi: 10.1016/j.jpeds.2013.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(Suppl 3):S174–84. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. The protective effect of community factors on childhood asthma. J Allergy Clin Immunol. 2009;123(6):1297–304. e2. doi: 10.1016/j.jaci.2009.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AF, Huang B, Ryan PH, Sandel MT, Chen C, Kahn RS. Areas with High Rates of Police-Reported Violent Crime Have Higher Rates of Childhood Asthma Morbidity. J Pediatr. 2016;173:175–82. e1. doi: 10.1016/j.jpeds.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beck AF, Huang B, Chundur R, Kahn RS. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Aff (Millwood) 2014;33(11):1993–2002. doi: 10.1377/hlthaff.2014.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102(12):2308–14. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 Suppl):757S–69S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 11.Hill TD, Graham LM, Divgi V. Racial disparities in pediatric asthma: a review of the literature. Curr Allergy Asthma Rep. 2011;11(1):85–90. doi: 10.1007/s11882-010-0159-2. [DOI] [PubMed] [Google Scholar]
- 12.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: parent perspectives. Pediatrics. 2000;106(3):512–9. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 13.Chen JT, Rehkopf DH, Waterman PD, Subramanian SV, Coull BA, Cohen B, et al. Mapping and measuring social disparities in premature mortality: the impact of census tract poverty within and across Boston neighborhoods, 1999–2001. J Urban Health. 2006;83(6):1063–84. doi: 10.1007/s11524-006-9089-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wise PH. The anatomy of a disparity in infant mortality. Annu Rev Public Health. 2003;24:341–62. doi: 10.1146/annurev.publhealth.24.100901.140816. [DOI] [PubMed] [Google Scholar]
- 15.Acevedo-Garcia D, McArdle N, Hardy EF, Crisan UI, Romano B, Norris D, et al. The child opportunity index: improving collaboration between community development and public health. Health Aff (Millwood) 2014;33(11):1948–57. doi: 10.1377/hlthaff.2014.0679. [DOI] [PubMed] [Google Scholar]
- 16.Beck AF, Klein MD, Schaffzin JK, Tallent V, Gillam M, Kahn RS. Identifying and treating a substandard housing cluster using a medical-legal partnership. Pediatrics. 2012;130(5):831–8. doi: 10.1542/peds.2012-0769. [DOI] [PubMed] [Google Scholar]
- 17.Child Opportunity Maps: The Heller School for Social Policy and Management. Brandeis University; [Accessed May 25, 2017]. updated 2016. Available from: http://www.diversitydatakids.org/data/childopportunitymap. [Google Scholar]
- 18. [Accessed January 29, 2017];American FactFinder. 2016 Available from: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
- 19.Thornton RL, Glover CM, Cene CW, Glik DC, Henderson JA, Williams DR. Evaluating Strategies For Reducing Health Disparities By Addressing The Social Determinants Of Health. Health Aff (Millwood) 2016;35(8):1416–23. doi: 10.1377/hlthaff.2015.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woolf SH, Purnell JQ. The Good Life: Working Together to Promote Opportunity and Improve Population Health and Well-being. JAMA. 2016;315(16):1706–8. doi: 10.1001/jama.2016.4263. [DOI] [PubMed] [Google Scholar]
- 21.Beck AF, Klein MD. Moving From Social Risk Assessment and Identification to Intervention and Treatment. Acad Pediatr. 2016;16(2):97–8. doi: 10.1016/j.acap.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 24.Clark NM. Community-based approaches to controlling childhood asthma. Annu Rev Public Health. 2012;33:193–208. doi: 10.1146/annurev-publhealth-031811-124532. [DOI] [PubMed] [Google Scholar]
- 25.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff (Millwood) 2008;27(2):321–33. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- 26.Pastor M, Morello-Frosch R. Integrating public health and community development to tackle neighborhood distress and promote well-being. Health Aff (Millwood) 2014;33(11):1890–6. doi: 10.1377/hlthaff.2014.0640. [DOI] [PubMed] [Google Scholar]
- 27.Stein RE, Siegel MJ, Bauman LJ. Double jeopardy: what social risk adds to biomedical risk in understanding child health and health care utilization. Acad Pediatr. 2010;10(3):165–71. doi: 10.1016/j.acap.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. J Allergy Clin Immunol. 2015;135(3):655–62. doi: 10.1016/j.jaci.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping Neighborhood Health Geomarkers To Clinical Care Decisions To Promote Equity In Child Health. Health Aff (Millwood) 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Council On Community Pediatrics. Poverty and Child Health in the United States. Pediatrics. 2016;137(4) doi: 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- 31.Chung EK, Siegel BS, Garg A, Conroy K, Gross RS, Long DA, et al. Screening for Social Determinants of Health Among Children and Families Living in Poverty: A Guide for Clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46(5):135–53. doi: 10.1016/j.cppeds.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fierman AH, Beck AF, Chung EK, Tschudy MM, Coker TR, Mistry KB, et al. Redesigning Health Care Practices to Address Childhood Poverty. Acad Pediatr. 2016;16(3 Suppl):S136–46. doi: 10.1016/j.acap.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Auger KA, Kahn RS, Simmons JM, Huang B, Shah AN, Timmons K, et al. Using Address Information to Identify Hardships Reported by Families of Children Hospitalized With Asthma. Acad Pediatr. 2017;17(1):79–87. doi: 10.1016/j.acap.2016.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Subramanyam M, Kawachi I, Berkman L, Subramanian SV. Relative deprivation in income and self-rated health in the United States. Soc Sci Med. 2009;69(3):327–34. doi: 10.1016/j.socscimed.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 35.Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001–2010. J Allergy Clin Immunol. 2014;134(3):547–53. e5. doi: 10.1016/j.jaci.2014.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]