Abstract
We describe a surgical technique for arthroscopic posterior cruciate ligament (PCL) reconstruction with remnant preservation of the original PCL fibers using a posterior trans-septal portal approach. Using the transtibial technique and the posterior trans-septal portal approach allows good visualization of the tibial tunnel preparation, easy access to the tibial tunnel without neurovascular injury, and preservation of remnant PCL fibers. In the preparation of the tibial tunnel, we expose the PCL tibial attachment site completely, detach the posterior capsule from the PCL, and preserve the distal stump of the PCL without neurovascular injury. PCL reconstruction is performed in a way that preserves the remnant PCL fibers. We report on our surgical technique for arthroscopic PCL reconstruction preserving the original PCL fibers.
No consensus has been reached on the optimal posterior cruciate ligament (PCL) reconstruction technique, including transtibial versus tibial inlay, single bundle versus double bundle, or 1 versus 2 incisions.1, 2 The advantages of arthroscopic transtibial single-bundle reconstruction over the tibial inlay technique or double-bundle reconstruction are that it is a relatively simple procedure with a short operation time and low morbidity.2
Conventional arthroscopic PCL reconstruction is technically difficult when creating an accurate tibial tunnel under good visualization without removing the remnant PCL fibers.3 Poor visualization of the tibial attachment site could lead to malpositioning of the tibial tunnel, which seems to be one of the most important causes of failure.4 In addition, it causes posterior-compartment neurovascular injury.4, 5, 6
PCL reconstruction using a posterior trans-septal portal could make tibial tunnel preparation easier without neurovascular injury by providing excellent visualization of the tibial attachment site of the original PCL fibers and could preserve the remnant fibers of the PCL as much as possible.2, 3, 7 If the remnant PCL fibers are well preserved, this could contribute to knee stability, restoration of proprioception by saving mechanoreceptors, and prevention of the killer-turn effect.2, 3, 7, 8, 9, 10, 11
We describe a surgical technique for arthroscopic PCL reconstruction with remnant preservation of the original PCL fibers using a posterior trans-septal portal, which could allow good visualization of the tibial attachment site and easy access to the tibial tunnel without neurovascular injury (Video 1).
Surgical Technique
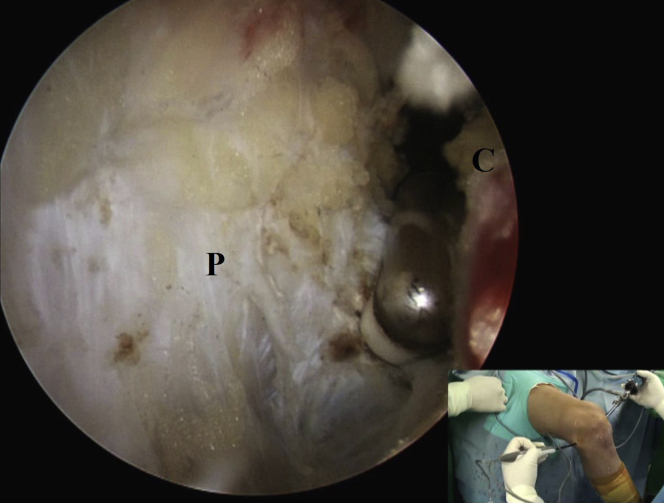
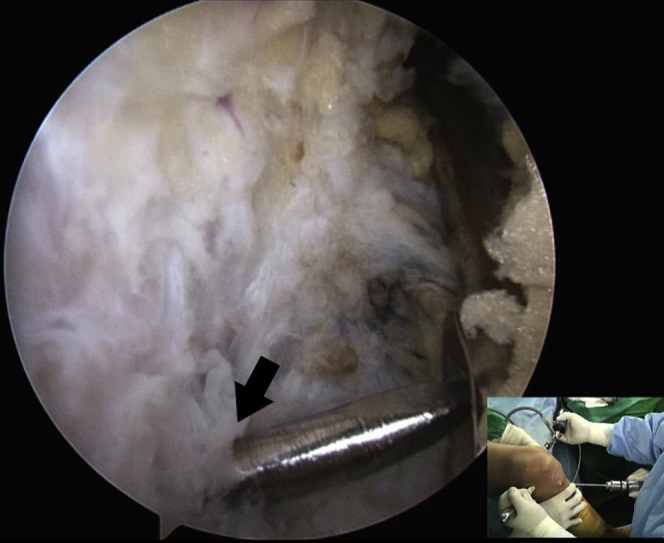
Creation of Posterior Trans-septal Portal
A routine arthroscopic examination is performed through standard anterolateral and anteromedial portals. We create additional posteromedial, posterolateral, and posterior trans-septal portals. A small hole is created at the posterior septum with a shaver behind the PCL without iatrogenic injury through the posteromedial portal. We pass the arthroscope into the posterolateral compartment through the posterior trans-septal portal. This portal is made at the central part of the posterior septum behind the PCL without disrupting the remnant PCL (Fig 1). After the posterolateral portal is created under direct visualization, the shaver and radiofrequency device are engaged through this portal to expose the PCL tibial attachment site completely.
Fig 1.
An arthroscopic view from the posteromedial portal in the right knee shows the posterior trans-septal portal (arrow) made at the central part of the posterior septum.
Preparation of Tibial Tunnel
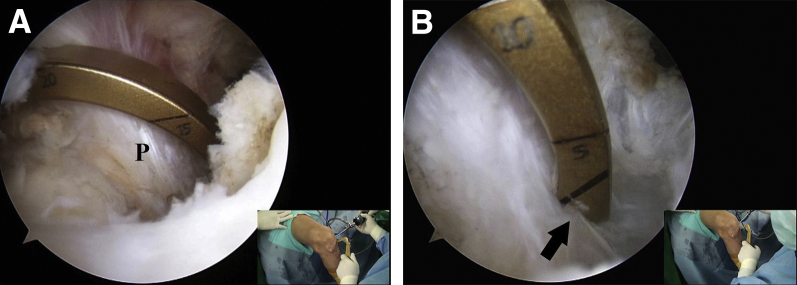
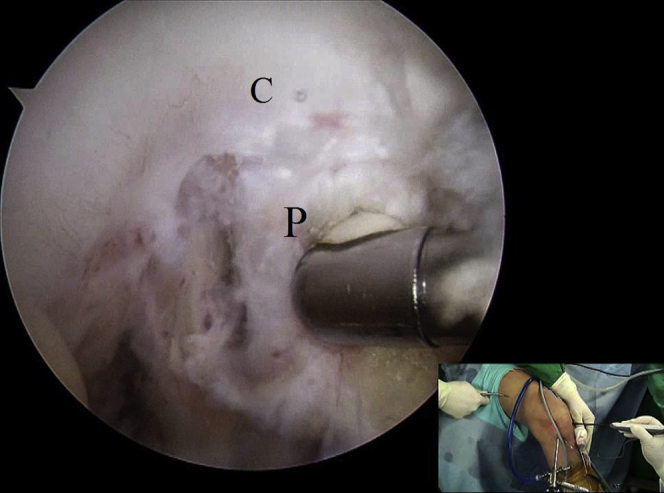
We detach the posterior capsule from the PCL more than 15 mm downward from the articular margin and preserve the distal stump of the PCL (Fig 2). The PCL tibial guide is inserted into the PCL tibial attachment site through the anteromedial portal under visualization through the posteromedial portal and advanced to approximately 15 mm below the joint line (Fig 3).
Fig 2.
Viewing from the posteromedial portal in the right knee at 90° of flexion, the radiofrequency device is engaged through the posterolateral portal to detach the posterior capsule (C) from the posterior cruciate ligament (P) more than 15 mm downward from the articular margin without disrupting the remnant posterior cruciate ligament.
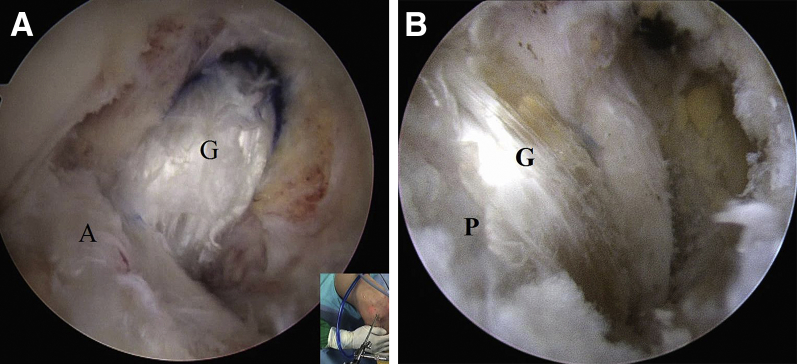
Fig 3.
The hook of the posterior cruciate ligament (PCL) tibial guide is introduced over the remnant PCL bundles (A) and is advanced into the PCL tibial attachment site (arrow) through the anteromedial portal in the right knee (B), viewing from the posteromedial portal. (P, PCL bundles.)
A guide pin is inserted from anterior to the superficial medial collateral ligament by placing the PCL guide at a 45° to 55° angle. The guide pin is drilled to penetrate the posterior cortex of the tibia at the distal and slightly lateral portion of the PCL tibial attachment site at 90° of flexion (Fig 4). With accumulated experience, the anatomic position on the tibia can be obtained under direct visualization through the posteromedial portal without intraoperative radiographs. A transtibial tunnel for the PCL graft—which is usually between 7 and 9 mm in diameter—is made, matching the diameter of the graft following the guide pin, and care using a curette should be taken to protect any neurovascular structures during the process of drilling and reaming. A fresh-frozen allograft (usually tibialis anterior or posterior), irradiated with 1.5 to 2.0 Mrad, is prepared simultaneously at a diameter of 7 to 9 mm.
Fig 4.
Viewing from the posteromedial portal in the right knee, the guide pin is drilled to penetrate the posterior cortex of the tibia at the distal and slightly lateral portion of the tibial attachment site (arrow) with minimal damage to the posterior cruciate ligament fibers.
Preparation of Femoral Tunnel
The remaining anterolateral bundle of the PCL femoral attachment is dissected, and the footprint is exposed with the shaver and radiofrequency device. The femoral tunnel location is about 7 mm and 11 mm from the trochlear point and the medial arch point of the medial femoral condyle, respectively, which is at the 1-o'clock position on the right side or 11-o'clock position on the left side (Fig 5). After insertion of the guide pin into the femoral footprint through an accessory anterolateral portal, which is 30 mm deep, 7 to 9 mm in diameter, and matched with the graft, the femoral tunnel is created.
Fig 5.
Viewing from the anterolateral portal in the right knee, the femoral tunnel location is marked about 7 to 8 mm posteriorly to the distal border of the articular cartilage (C) of the medial femoral condyle, which is at the 1-o'clock position through the anteromedial portal.
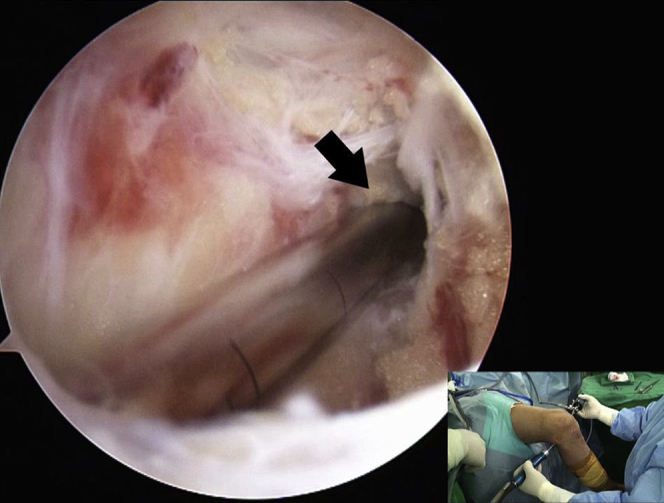
Graft Passage and Fixation
A wire loop is inserted from the exit of the tibial tunnel, passed through the posterior compartment, and taken out through the accessory anterolateral portal to pass the graft. First, the graft, attached to the wire loop, is pulled into the femoral tunnel by inside-out and press-fit methods; fixed with 2 cross pins (Rigidfix system; DePuy Mitek, Raynham, MA); and pulled out through the tibial tunnel. The graft is then fixed to the tibial tunnel with 2 bioabsorbable interference screws (Smith & Nephew, London, England) while the knee is kept in a reduced position at 90° of flexion (Fig 6).
Fig 6.
(A) An arthroscopic view from the anterolateral portal in the right knee shows that the posterior cruciate ligament (PCL) graft (G) and the remnant PCL on the femoral side have good tension after fixation. (A, anterior cruciate ligament.) (B) An arthroscopic view from the posteromedial portal in the right knee shows that the PCL graft (G) and the remnant PCL (P) on the tibial side have good tension after fixation.
Discussion
In conventional transtibial PCL reconstructions, it is difficult to visualize the original PCL fibers at the tibial attachment site, and poor visualization of the tibial attachment site could lead to malpositioning of the tibial tunnel.3, 12 This malpositioning could cause impingement of the graft, which is medially directed with the medial femoral condyle, and result in graft loosening or failure. In our technique, we detach the posterior capsule from the PCL more than 15 mm downward from the articular margin, preserve the distal stump of the PCL, and expose the PCL tibial attachment site completely without neurovascular injury. This procedure allows the surgeon to make an accurate transtibial tunnel with minimal damage to the remaining distal stump of the PCL.
Ahn et al.3, 6 described the posterior trans-septal portal and suggested that it provides excellent visualization of the tibial insertion site and has a lower risk of neurovascular injury when dissecting soft tissue between the posterior capsule and the remnant PCL fibers. This remnant preservation is advantageous to gain postoperative stability, restore proprioception by saving mechanoreceptors, and avoid the killer-turn effect by acting like a cushion.2, 7, 8, 9, 10, 11 If the remnant fibers of the PCL are removed to expose the bony landmark, we have to use at least a 10-mm-diameter graft for PCL reconstruction. However, in the remnant-preservation technique, we have tried to preserve the remnant fibers of the PCL as much as possible, and when performing this technique, we have been able to use a graft and tibial tunnel with an 8-mm diameter, on average, to augment and reinforce the remnant PCL bundles, especially for the anterolateral bundle. Regarding the better healing potential of the PCL versus the anterior cruciate ligament, Ahn et al.7 showed that the remnant PCL fibers and the graft healed together and formed a broad cross-sectional area, and the graft was revascularized and healed with the remnant PCL fibers.
Lee et al.2 reported that clinical outcomes and posterior instability improved significantly, postoperative proprioception recovered to a level similar to that of the uninvolved side, and magnetic resonance imaging (MRI) and second-look arthroscopy showed a high rate of complete healing and synovialization in patients who underwent either isolated transtibial PCL reconstruction with the posterior trans-septal portal or combined posterolateral corner and PCL reconstruction. They showed normal integrity in 100% of patients as well as complete synovialization in 86% at the tibial attachment site on second-look arthroscopy at a minimum of 2 years after surgery. They assumed that remnant PCL fibers would heal with the graft and provide less loosening of the graft induced by the killer turn, as well as restoration of sensation for joint motion and position. Ahn et al.7 performed follow-up MRI and second-look arthroscopy at a mean of 11 months after remnant-preserving PCL reconstruction and found no tearing of the graft on the tibial side. Kim et al.12 reported that remnant-preserving PCL reconstruction with posterolateral corner reconstruction showed better activity-related outcomes than techniques without remnant preservation.
It is theoretically reasonable to perform a double-bundle reconstruction to achieve better stability, given that the PCL consists of 2 main bundles. However, recent studies have shown no difference in clinical results between single- and double-bundle reconstruction.13, 14 Lee et al.2 reported that postoperative clinical scores and posterior displacement measured by a KT-2000 (MEDmetric) or Telos device were similar or superior to those of double- or single-bundle reconstruction.13, 15 Recent studies have proved that the graft was healed together with the remnant PCL bundles at the femoral and tibial attachment sites and formed a broad cross-sectional area, similar to a normal double-bundle PCL technique after remnant preservation, on follow-up MRI and second-look arthroscopy.2, 7
In summary, arthroscopic PCL reconstruction using the posterior trans-septal portal is anticipated to provide a single-bundle reconstruction with remnant preservation and without complications. Table 1 describes advantages and disadvantages of our technique, and Table 2 presents pitfalls and tips.
Table 1.
Advantages and Disadvantages
| Advantages |
| Improved exposure of PCL tibial attachment site, which lies >10 mm below articular surface |
| Preservation of maximal amount of remnant PCL fibers |
| Minimal neurovascular injury |
| Minimal killer-turn effect |
| Disadvantages |
| Difficulty in determining exact tibial footprint of PCL during learning curve |
| Creation of additional portals: posteromedial, posterolateral, and trans-septal portals |
| Difficulty in passage of graft between remnant PCL bundles and surrounding soft tissues |
PCL, posterior cruciate ligament.
Table 2.
Pitfalls and Tips
| Pitfalls |
| When the surgeon is creating the trans-septal portal directly, moving the rod posteriorly while breaking the septum can result in neurovascular injury. |
| Sometimes, it is a struggle to pass the graft between the remnant PCL bundles and surrounding soft tissues. |
| The killer-turn effect is still a possibility. |
| Tips |
| When creating the trans-septal portal directly, the surgeon should keep the rod anterior and close to the bone as much as possible to prevent posterior neurovascular injury. |
| Performing sufficient soft-tissue debridement and PCL shrinkage with an electrocautery device is helpful in achieving easier graft passage. |
| Rasping the acute entrance of the tibial tunnel after reaming is a way to reduce the killer-turn effect. |
PCL, posterior cruciate ligament.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique of arthroscopic posterior cruciate ligament (PCL) reconstruction with remnant preservation of the original PCL fibers using a posterior trans-septal portal approach in the right knee. After creation of additional posteromedial (mainly the viewing portal), posterolateral (mainly the working portal), and posterior trans-septal portals, a small hole is created at the posterior septum with a shaver behind the PCL. We pass the arthroscope into the posterolateral compartment through the posterior trans-septal portal. This portal is made at the central part of the posterior septum behind the PCL without disrupting the remnant PCL. After the posterolateral portal is created, the shaver and radiofrequency device are engaged through this portal to expose the PCL tibial attachment site completely while viewing from the posteromedial portal. We detach the posterior capsule from the PCL more than 15 mm downward from the articular margin and preserve the distal stump of the PCL. The PCL tibial guide is inserted into the PCL tibial attachment site through an anteromedial portal under visualization through the posteromedial portal and advanced to approximately 15 mm below the joint line. A guide pin is inserted from anterior to the superficial medial collateral ligament by placing the PCL guide at a 45° to 55° angle. The guide pin is drilled to penetrate the posterior cortex of the tibia at the distal and slightly lateral portion of the PCL tibial attachment site. A transtibial tunnel for the PCL graft—which is usually between 7 and 9 mm in diameter—is made, matching the diameter of the graft following the guide pin, and care using a curette should be taken to protect any neurovascular structures during the process of drilling and reaming. A fresh-frozen allograft (usually tibialis anterior or posterior), irradiated with 1.5 to 2.0 Mrad, is prepared simultaneously at a diameter of 7 to 9 mm. The remaining anterolateral bundle of the PCL femoral attachment is dissected, and the footprint is exposed with the shaver and radiofrequency device through an anterolateral portal while viewing from the anteromedial portal. The femoral tunnel location is about 7 mm and 11 mm from the trochlear point and the medial arch point of the medial femoral condyle, respectively, which is at the 1-o'clock position on the right side or 11-o'clock position on the left side. After insertion of the guide pin into the femoral footprint through an accessory anterolateral portal, which is 30 mm deep, 7 to 9 mm in diameter, and matched with the graft, the femoral tunnel is created. A wire loop is inserted from the exit of the tibial tunnel, passes through the posterior compartment, and is taken out through the accessory anterolateral portal to pass the graft. First, the graft, attached to the wire loop, is pulled into the femoral tunnel by inside-out and press-fit methods; fixed with 2 cross pins (Rigidfix system); and pulled out through the tibial tunnel. The graft is then fixed to the tibial tunnel with 2 bioabsorbable interference screws (Smith & Nephew) while the knee is kept in a reduced position at 90° of flexion. This surgical technique could provide an effective transtibial single-bundle reconstruction with remnant preservation and without neurovascular injury.
References
- 1.LaPrade C.M., Civitarese D.M., Rasmussen M.T., LaPrade R.F. Emerging updates on the posterior cruciate ligament: A review of the current literature. Am J Sports Med. 2015;43:3077–3092. doi: 10.1177/0363546515572770. [DOI] [PubMed] [Google Scholar]
- 2.Lee D.W., Jang H.W., Lee Y.S. Clinical, functional, and morphological evaluations of posterior cruciate ligament reconstruction with remnant preservation minimum 2-year follow-up. Am J Sports Med. 2014;42:1822–1831. doi: 10.1177/0363546514536680. [DOI] [PubMed] [Google Scholar]
- 3.Ahn J.H., Chung Y.S., Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003;19:101–107. doi: 10.1053/jars.2003.50017. [DOI] [PubMed] [Google Scholar]
- 4.Nicodeme J.D., Locherbach C., Jolles B.M. Tibial tunnel placement in posterior cruciate ligament reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:1556–1562. doi: 10.1007/s00167-013-2563-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee Y.S., Ra H.J., Ahn J.H., Ha J.K., Kim J.G. Posterior cruciate ligament tibial insertion anatomy and implications for tibial tunnel placement. Arthroscopy. 2011;27:182–187. doi: 10.1016/j.arthro.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 6.Ahn J.H., Wang J.H., Lee S.H., Yoo J.C., Jeon W.J. Increasing the distance between the posterior cruciate ligament and the popliteal neurovascular bundle by a limited posterior capsular release during arthroscopic transtibial posterior cruciate ligament reconstruction—A cadaveric angiographic study. Am J Sports Med. 2007;35:787–792. doi: 10.1177/0363546506297908. [DOI] [PubMed] [Google Scholar]
- 7.Ahn J.H., Yang H.S., Jeong W.K., Koh K.H. Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: Clinical results of minimum 2-year follow-up. Am J Sports Med. 2006;34:194–204. doi: 10.1177/0363546505279915. [DOI] [PubMed] [Google Scholar]
- 8.Lee D.C., Shon O.J., Kwack B.H., Lee S.J. Proprioception and clinical results of anterolateral single-bundle posterior cruciate ligament reconstruction with remnant preservation. Knee Surg Relat Res. 2013;25:126–132. doi: 10.5792/ksrr.2013.25.3.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song J.G., Kim H.J., Han J.H. Clinical outcome of posterior cruciate ligament reconstruction with and without remnant preservation. Arthroscopy. 2015;31:1796–1806. doi: 10.1016/j.arthro.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Lee S.H., Jung Y.B., Lee H.J., Jung H.J., Kim S.H. Remnant preservation is helpful to obtain good clinical results in posterior cruciate ligament reconstruction: Comparison of clinical results of three techniques. Clin Orthop Surg. 2013;5:278–286. doi: 10.4055/cios.2013.5.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eguchi A., Adachi N., Nakamae A., Usman M.A., Deie M., Ochi M. Proprioceptive function after isolated single-bundle posterior cruciate ligament reconstruction with remnant preservation for chronic posterior cruciate ligament injuries. Orthop Traumatol Surg Res. 2014;100:303–308. doi: 10.1016/j.otsr.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Kim S.J., Kim S.H., Chun Y.M., Hwang B.Y., Choi D.H., Yoon J.Y. Clinical comparison of conventional and remnant-preserving transtibial single-bundle posterior cruciate ligament reconstruction combined with posterolateral corner reconstruction. Am J Sports Med. 2012;40:640–649. doi: 10.1177/0363546511428068. [DOI] [PubMed] [Google Scholar]
- 13.Kim S.J., Jung M., Moon H.K., Kim S.G., Chun Y.M. Anterolateral transtibial posterior cruciate ligament reconstruction combined with anatomical reconstruction of posterolateral corner insufficiency: Comparison of single-bundle versus double-bundle posterior cruciate ligament reconstruction over a 2- to 6-year follow-up. Am J Sports Med. 2011;39:481–489. doi: 10.1177/0363546510385398. [DOI] [PubMed] [Google Scholar]
- 14.Apsingi S., Nguyen T., Bull A.M., Unwin A., Deehan D.J., Amis A.A. Control of laxity in knees with combined posterior cruciate ligament and posterolateral corner deficiency: Comparison of single-bundle versus double-bundle posterior cruciate ligament reconstruction combined with modified Larson posterolateral corner reconstruction. Am J Sports Med. 2008;36:487–494. doi: 10.1177/0363546508314415. [DOI] [PubMed] [Google Scholar]
- 15.Min B.H., Lee Y.S., Jin C.Z., Son K.H. Evaluation of transtibial double-bundle posterior cruciate ligament reconstruction using a single-sling method with a tibialis anterior allograft. Am J Sports Med. 2011;39:374–379. doi: 10.1177/0363546510382207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique of arthroscopic posterior cruciate ligament (PCL) reconstruction with remnant preservation of the original PCL fibers using a posterior trans-septal portal approach in the right knee. After creation of additional posteromedial (mainly the viewing portal), posterolateral (mainly the working portal), and posterior trans-septal portals, a small hole is created at the posterior septum with a shaver behind the PCL. We pass the arthroscope into the posterolateral compartment through the posterior trans-septal portal. This portal is made at the central part of the posterior septum behind the PCL without disrupting the remnant PCL. After the posterolateral portal is created, the shaver and radiofrequency device are engaged through this portal to expose the PCL tibial attachment site completely while viewing from the posteromedial portal. We detach the posterior capsule from the PCL more than 15 mm downward from the articular margin and preserve the distal stump of the PCL. The PCL tibial guide is inserted into the PCL tibial attachment site through an anteromedial portal under visualization through the posteromedial portal and advanced to approximately 15 mm below the joint line. A guide pin is inserted from anterior to the superficial medial collateral ligament by placing the PCL guide at a 45° to 55° angle. The guide pin is drilled to penetrate the posterior cortex of the tibia at the distal and slightly lateral portion of the PCL tibial attachment site. A transtibial tunnel for the PCL graft—which is usually between 7 and 9 mm in diameter—is made, matching the diameter of the graft following the guide pin, and care using a curette should be taken to protect any neurovascular structures during the process of drilling and reaming. A fresh-frozen allograft (usually tibialis anterior or posterior), irradiated with 1.5 to 2.0 Mrad, is prepared simultaneously at a diameter of 7 to 9 mm. The remaining anterolateral bundle of the PCL femoral attachment is dissected, and the footprint is exposed with the shaver and radiofrequency device through an anterolateral portal while viewing from the anteromedial portal. The femoral tunnel location is about 7 mm and 11 mm from the trochlear point and the medial arch point of the medial femoral condyle, respectively, which is at the 1-o'clock position on the right side or 11-o'clock position on the left side. After insertion of the guide pin into the femoral footprint through an accessory anterolateral portal, which is 30 mm deep, 7 to 9 mm in diameter, and matched with the graft, the femoral tunnel is created. A wire loop is inserted from the exit of the tibial tunnel, passes through the posterior compartment, and is taken out through the accessory anterolateral portal to pass the graft. First, the graft, attached to the wire loop, is pulled into the femoral tunnel by inside-out and press-fit methods; fixed with 2 cross pins (Rigidfix system); and pulled out through the tibial tunnel. The graft is then fixed to the tibial tunnel with 2 bioabsorbable interference screws (Smith & Nephew) while the knee is kept in a reduced position at 90° of flexion. This surgical technique could provide an effective transtibial single-bundle reconstruction with remnant preservation and without neurovascular injury.