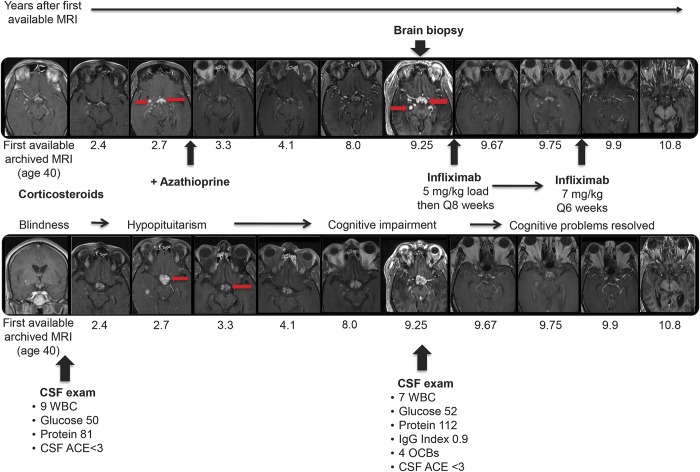
Figure 1. Progression of CNS sarcoidosis over 10 years despite conventional immunosuppressive therapy with complete remission on infliximab.
At age 37, this previously healthy African American man developed bilateral sequential optic neuropathy. Over the next 3 years, he progressed to blindness with no light perception bilaterally, despite aggressive glucocorticoid therapy. Chest CT at age 39 showed mild bilateral hilar lymphadenopathy, and biopsy of nasal mucosa at age 42 was consistent with sarcoidosis. Over the next decade, he went on to develop hypopituitarism, cognitive impairment (correlating with further subcortical involvement on neuroimaging), and intractable hiccups despite treatment with oral glucocorticoids and azathioprine. At age 50, brain biopsy of an enhancing lesion in the right thalamus showed non-necrotizing granulomatous inflammation consistent with CNS sarcoidosis. The top and bottom rows show serial T1 postgadolinium MRIs from 2 different anatomic levels with the x-axis aligned by time. The MRIs show that there is persistent waxing and waning abnormal nodular enhancement (arrows show some examples) in the same neuroanatomic distribution over 10 years, which finally remitted following treatment with infliximab, initially at an escalated dose of 7 mg/kg IV every 6 weeks and since maintained on infliximab 5 mg/kg Q8 weeks together with azathioprine 50 mg/d and replacement doses of glucocorticoids. Remission of the CNS process has been maintained for over 4 years. The patient had breakthrough sarcoidal granulomatous dermatitis on this maintenance regimen 2.5 years into his CNS remission, and the facial lesions subsequently resolved. His hiccups resolved and cognition returned to baseline; as expected, there has been no improvement in visual function. ACE = angiotensin-converting enzyme; IgG = immunoglobulin G; OCB = oligoclonal band; WBC = white blood cell.