Figure 1.
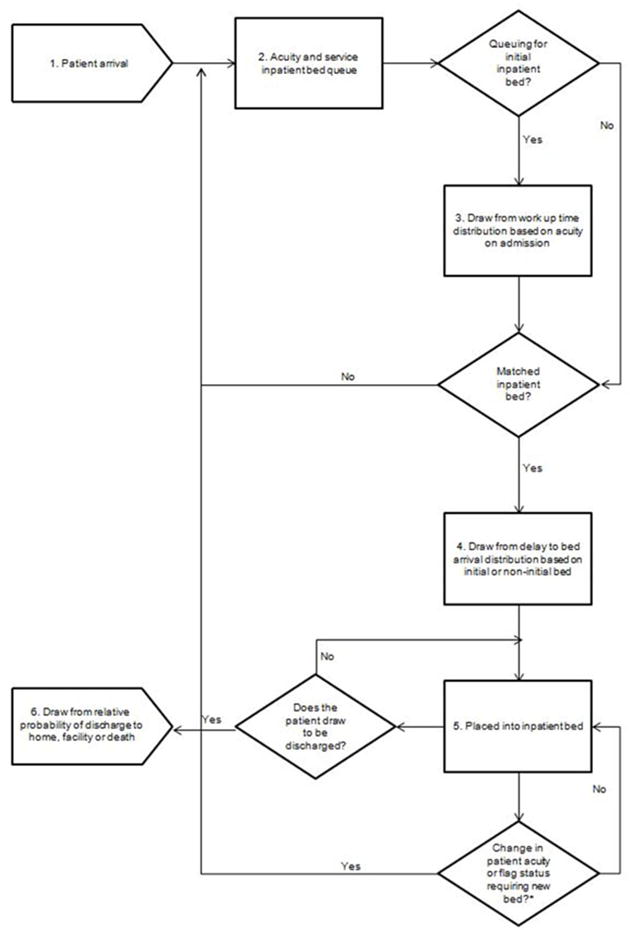
Model schematic. Patients experience six different events as they progress through the model: First, patients arrive in the hospital on an hourly basis (1). Each patient has four inherent characteristics that are relevant for bed allocation: acuity on arrival, service required (medical or surgical), gender, and MRSA and VRE flag status. The source of patient arrival is not modeled, nor is their physical location as they await initial bed placement. Next, on the basis of the combination of their four characteristics upon arrival, patients awaiting admission are instantly assigned to an acuity/service queue (2). The model does not begin to look for available beds immediately upon entrance to the queue. Instead, the model approximates work up time (i.e., an approximation of the time required by clinicians to evaluate and begin initial management of the patient) (3). During the time patients are being worked up, they may experience changes in acuity at each time step (i.e., if their condition improves their acuity will decrease, if their condition worsens, their acuity level will increase). If this change occurs, a patient’s acuity is updated and informs the bed match. Once a bed match is made, patients do not instantly arrive in the assigned bed. In order to account for delays in clinician-to-clinician pass-offs, as well as transport and other non-clinical administrative delays, the model draws from a relative distribution of delay in bed arrival in hours (4). At the completion of the delay to bed arrival, patients are placed in an inpatient bed within their required service and acuity level (5).Finally, at each hour the model draws from a discharge distribution to determine if each patient is ready to be discharged (6).
*Not all patients experience a change in patient acuity or flag status requiring a new bed. These patients will remain in their initial inpatient bed until discharge.
