Abstract
Head and neck squamous cell carcinoma (HNSCC) has been treated for decades with cisplatin chemotherapy, and anti–PD-1 immunotherapy has recently been approved for the treatment of this disease. However, preclinical studies of how antitumor immunity in HNSCC is affected by cisplatin alone or in combination with immunotherapies are lacking. Here, we show that sublethal doses of cisplatin may enhance antigen presentation and T-cell killing in vitro, though cisplatin also upregulates tumor cell expression of PD-L1 and may impair T-cell function at higher doses. In a syngeneic mouse model of HNSCC, concurrent use of cisplatin and anti–PD-L1/PD-1 delayed tumor growth and enhanced survival without significantly reducing the number or function of tumor-infiltrating immune cells or increasing cisplatin-induced toxicities. These results suggest that moderate doses of cisplatin may enhance antitumor immunity by mechanisms other than direct tumor cell killing, which may be further enhanced by anti–PD-L1/PD-1 therapy.
Keywords: cisplatin chemotherapy, PD-1, PD-L1, head and neck cancer, squamous cell carcinoma
INTRODUCTION
Head and neck squamous cell carcinoma (HNSCC), the sixth most common cancer type worldwide, is an aggressive malignancy with little improvement in overall survival during the past few decades (1). Clinical trials have focused on improving survival for patients with HNSCC related to carcinogen exposure, who have a relatively poor prognosis, and reducing treatment-related toxicities in patients with human papillomavirus (HPV)-associated HSNCC, which portends a relatively favorable prognosis (2). Cisplatin chemotherapy has been the standard systemic therapy for HNSCC for decades, but it offers modest increases in survival and substantial toxicity when used at traditional high doses (3, 4). Antibodies targeting the programmed death 1 (PD-1) immune checkpoint pathway have recently been FDA approved based on clinical trials showing sustained responses in patients with recurrent or metastatic HNSCC that were refractory to multiple prior treatments (5, 6). However, not all HNSCC patients respond to anti–PD-1 monotherapy. Combinations of immunotherapy with standard therapies are, thus, an attractive option for head and neck cancer patients.
The combination of anti–PD-1 immunotherapy with cisplatin chemotherapy for HNSCC is currently under exploration in clinical trials. However, the impact of cisplatin alone or in combination with checkpoint inhibitors on antitumor immunity has not been explored in preclinical models of HNSCC. Prior preclinical and clinical studies in other cancer types suggest that cisplatin and other cytotoxic chemotherapy drugs may enhance antitumor immunity by enhancing immunogenic cell death, increasing expression of MHC class I and other components of the antigen processing machinery, enhancing numbers and function of immune effector cells, and decreasing numbers of immunosuppressive cells (7–10). However, other preclinical studies suggest that cytotoxic chemotherapy can upregulate tumor cell expression of PD-L1 (11, 12), potentially impairing antitumor immunity by inducing T-cell anergy.
In the current study, we used multiple human and mouse HNSCC cell lines and antigen-specific, engineered mouse T cells to explore the effects of cisplatin on antigen processing machinery, PD-L1 expression, and T-cell function. A syngeneic mouse model of oral cancer was used to mechanistically investigate the effects of cisplatin and PD-L1/PD-1 blockade on tumor growth in vivo. We show that in these preclinical models of HNSCC, cisplatin can have both immune-enhancing and immunosuppressive effects, which may be dose-dependent and partially reversible by combination with PD-L1/PD-1 blockade.
MATERIALS AND METHODS
Cell lines
UMSCC-1, UMSCC-46 and UMSCC-74A cell lines were obtained from Dr. T. Carey at the University of Michigan and were authenticated by PCR and maintained as previously described (13). UPCI SCC90 cells were obtained from Dr. Robert Ferris and Dr. Susanne Gollin at the University of Pittsburgh and were validated there by PCR, exome sequencing, and fluorescence in situ hybridization as described (14, 15). Human cell lines were maintained in MEM or DMEM with 1% penicillin/streptomycin, 1% glutamine, and 10% FBS. Mouse oral cancer (MOC) 1 and 2 cell lines were obtained from Dr. R. Uppaluri in 2014 and were authenticated by exome sequencing and maintained as previously described (16, 17). All cell lines were stored in liquid nitrogen and cultured for no longer than 6 months or 20 passages before use. All cell lines were tested monthly for mycoplasma.
Antibodies and reagents
Recombinant human interferon gamma (IFNγ; catalog no. 570206) and antibodies to human HLA-ABC (catalog no. 311404) and PD-L1 (catalog no. 329706) were obtained from Biolegend. The antibody for intracellular calreticulin was obtained from R&D Systems (catalog no. IC3898R), and the antibodies to TAP1, TAP2, LMP2, ERp57 were obtained from Abcam (catalog numbers ab83817, ab180611, ab190350, and ab13506, respectively). Pharmaceutical grade cisplatin was obtained from the veterinary pharmacy at NIH. Antibodies for in vivo mouse treatments specific for PD-L1 (clone 10F.9G2), PD-1 (clone RMP1-14), NK1.1 (clone PK136) and CD8 (clone YTS 169.4) were from BioXCell. Fluorescent-conjugated flow cytometry antibodies for mouse tumor experiments were obtained from eBioscience (CD137/41BB, catalog no. 46-1371-80) or Biolegend: CD8 (catalog no. 100712), CD45.2 (catalog no. 109806), CD80 (catalog no. 104721), CD11b (catalog no. 101211), CD11c (catalog no. 117307), CD107a (catalog no. 121619), Ly6G (catalog no. 127623), Ly6C (catalog no. 128017), and H-2Kb/H-2Db (catalog no. 114611).
In vitro drug treatments and cell death assays
Cells were plated at 5 × 104 to 1 × 105 cells per well in 6-well plates and allowed to adhere overnight prior to treatment with IFN-γ (10 ng/ml) or cisplatin (see doses in Supplementary Table 1). PE Annexin V/7AAD Apoptosis Detection Kit (BD Biosciences) and Cell Proliferation Kit I/XTT (Sigma) cell death assays were used according to the manufacturer instructions.
Flow cytometry
Cell lines were harvested with TrypLE Select (Thermofisher) prior to staining for flow cytometry. For intracellular staining, cells were fixed in 2% paraformaldehyde (PFA) and permeabilized with 100% methanol overnight at −20°C. Data were acquired using a BD FACS Canto I cytometer and BD FACS Diva software, and then analyzed using FlowJo software. Cell viability was verified using 7AAD staining. Median fluorescence intensity values for isotype controls were subtracted for each condition, and “fluorescence minus one” controls were tested for each multicolor flow panel.
In vivo mouse studies
Wildtype, female C57BL/6 mice at 6–8 weeks were obtained from Charles River Laboratories. Mice were injected in the right flank with MOC1 (5 × 106, in matrigel) or MOC2 (1 × 105) cells and allowed to grow for 11–14 days, and then randomized into treatment groups. Mice were then treated with cisplatin (cis-diamminedichloroplatinum(II): CDDP; 3 or 5 mg/kg/week) and/or antibodies to PD-1 or PD-L1 (200 μg, twice/week) or vehicle (saline/PBS) by intraperitoneal injection. Cisplatin-treated mice received additional saline supplementation (0.5 ml daily × 2 days following cisplatin by subcutaneous injection). The cisplatin dose chosen was the maximum tolerated weekly dose that did not cause excessive illness or weight loss in preliminary experiments, as we were unable to find pharmacokinetic data in the literature comparing murine doses to clinically relevant doses. Antibodies blocking PD-1 and PD-L1 were used at 200 mcg twice weekly by intraperitoneal injection as established in the literature (18–21). Because previous experiments in our laboratories have shown no effect of isotype controls for anti–PD-1 and anti–PD-L1 antibodies (rat IgG2a and IgG2b, respectively) on tumor growth, control animals were not treated with isotype control antibodies in these experiments.
CD8+ T cells and NK cells were depleted in a subset of mice by intraperitoneal injection of depleting antibodies (clones listed above) at 200 mcg twice weekly as previously described and validated (22).
In a subset of mice from each experiment, tumors were harvested prior to completion of treatment (day 20 or day 25 as indicated), digested into single cell suspensions with mechanical dissociation followed by enzymatic dissociation using Miltenyi’s mouse tumor dissociation kit and GentleMACS Dissociator as previously described (22), then analyzed by flow cytometry for tumor cell surface markers and immune cell phenotypes. Mouse hearing tests (auditory brainstem response thresholds and distortion product otoacoustic emission amplitudes) were performed as previously described (23, 24), and kidney histology (H&E staining of paraffin-embedded tissue) was performed using standard methods by Histoserv (Germantown, Maryland). All animal procedures were approved by the NIDCD Animal Care and Use Committee.
T-cell assays
To generate SIINFEKL-specific cytotoxic T lymphocytes (CTLs), splenocytes from OT-1 mice were cultured in the presence of SIINFEKL (2 μg/ml) with daily 2:1 splitting. For IFNγ capture assays, OT-1 splenocytes were cultured with cisplatin at indicated doses for 24 hours, then stimulated with SIINFEKL peptide. CD8+Vα2+ T cells were then labeled for IFNγ capture using a Mouse IFN-γ Secretion Assay – Detection Kit according to the manufacturer’s instructions (Miltenyi) and analyzed by flow cytometry.
For CTL killing assays, 1×104 target cells (ovalbumin-expressing MOC1 cells) were plated in a 96-well E-Plate (ACEA Biosciences) and cultured with or without cisplatin at indicated doses for 24 hours prior to adding OT-1 CTL effector cells. Alteration of impedance was acquired using the xCELLigence Real-Time Cell Analysis (RTCA) platform per manufacturer instructions. Triton X-100 (0.2%) was added to some wells to verify complete loss of cell index with total cell lysis, and CTLs alone were plated up to 1×106/well to verify that they do not contribute to gain of impedance. Percent loss of cell index for a given time point was calculated as: 1-(experimental cell index/control cell index).
Statistical analyses
Data from in vitro experiments were analyzed by one- or two-way ANOVA where appropriate. Tumor growth curves were compared by linear regression. Animal survival curves were made using the Kaplan-Meier method with comparison by using log-rank (Mantel-Cox) testing. GraphPad Prism software was used for statistical testing. P < 0.05 was used to determine statistical significance.
RESULTS
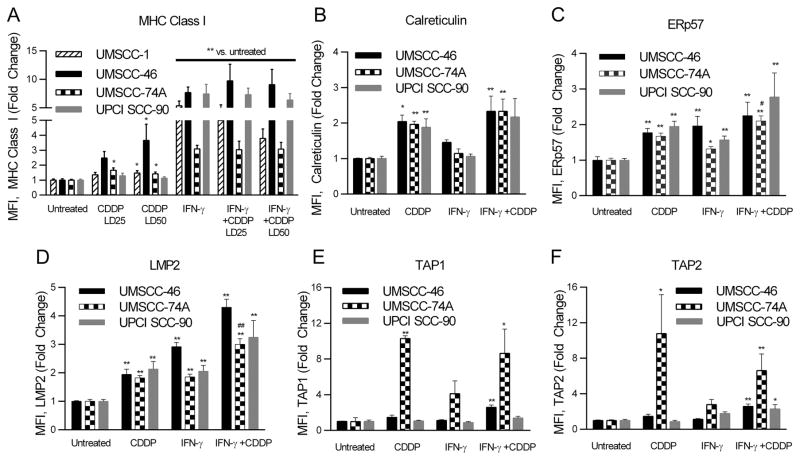
Cisplatin induces upregulation of antigen processing machinery (APM) components
To investigate whether cisplatin might enhance antigen presentation and adaptive immunity by mechanisms other than release of antigen from dying cells, several APM components were assessed in HNSCC cell lines treated with cisplatin. First, doses needed to kill 25% (LD25) or 50% (LD50) of cells in 72 hours were determined for each cell line (Supplementary Table S1). Treatment with these doses of cisplatin or IFNγ (positive control) alone or in combination increased cell surface MHC class I/HLA-ABC (Fig. 1A). Intracellular calreticulin, ERp57, and LMP2 also increased with cisplatin, with additive increases in ERp57 and LMP2 noted with combination cisplatin and IFNγ in UMSCC-74A cells (Fig. 1B–D). Cisplatin-induced increases in transporter of antigen proteins (TAP1 and TAP2) were noted only in the UMSCC-74A cells (Fig. 1E and F), which retain expression of wild type TP53 (25), an established inducer of TAP1 (26).
Figure 1. Cisplatin induces upregulation of APM components.
Cell lines were treated with IFNγ (10 ng/ml, positive control) or cisplatin (CDDP) for 48 hours, then assessed by flow cytometry. A, Surface MHC class I/HLA-ABC or B–F, intracellular levels of other APM components in cell lines. Data are mean + SEM from at least two independent experiments performed in triplicate, * p <0.05, ** p <0.01 vs. untreated, # p <0.05, ## p <0.01 vs. IFNγ or CDDP alone determined by one-way ANOVA with post-hoc Tukey’s multiple comparison test. “CDDP” in B–F refers to the LD50 for each cell line (see Supplementary Table S1 for doses). Cell lines: UMSCC-1 (striped), UMSCC-46 (solid black), UMSCC-74A (bricked), and UPCI SCC90 (solid gray).
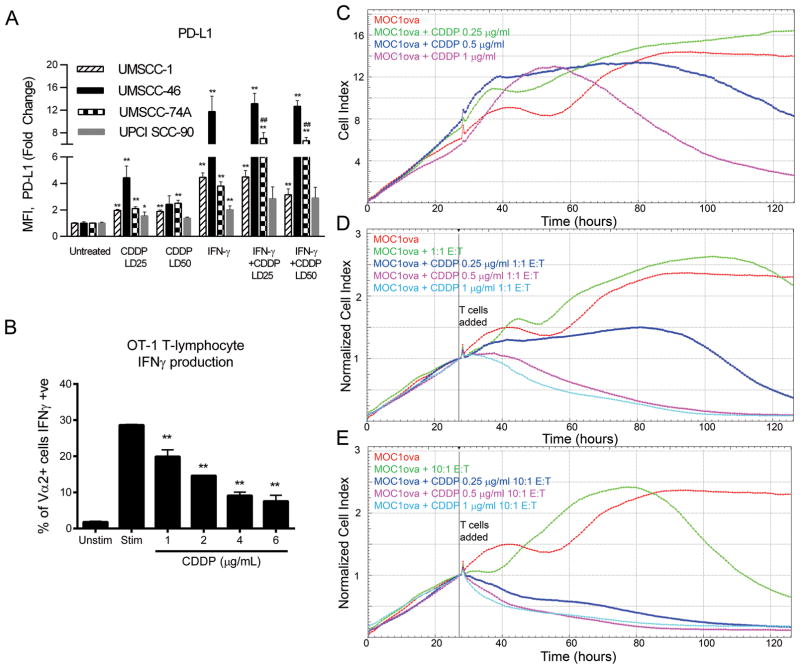
Cisplatin increases PD-L1 expression on HNSCC tumor cells and impacts T-cell function
Although cisplatin-induced increases in APM component expression may enhance antitumor immunity, we hypothesized that it may also impair antitumor immunity in other ways, such as upregulation of immune checkpoints or impairment of T-cell function. HNSCC cell lines treated with the LD25 or LD50 of cisplatin (or IFNγ as a positive control) for 48 hours showed increased surface expression of PD-L1 (Fig. 2A). To investigate T-cell function, antigen-specific IFNγ production by OT-1 T cells was measured after stimulation by pulsing with SIINFEKL peptide in the presence or absence of cisplatin, with doses chosen based on the plasma concentrations of cisplatin (2–6 μg/ml) following a standard-of-care dose of cisplatin (100 mg/m2) in the clinical setting (27). Although the lower doses of cisplatin did not drastically impair IFNγ production, the doses reflecting peak serum concentrations (4–6 μg/ml) significantly reduced IFNγ production by stimulated T cells (Fig. 2B). Tumor cell killing by CTLs was investigated using an antigen-specific, impedance-based assay with MOC1 cells expressing ovalbumin and OT-1 T cells. Low doses of cisplatin or T cells when used alone did not induce tumor cell killing. However, when used together, sublethal doses of cisplatin (determined by prior XTT assays) enhanced tumor cell killing by antigen-specific CTLs (Fig. 2C–E). The T cells in these experiments were cocultured with cisplatin along with the tumor cells, but they were not added to the treatment wells until 24 hours after the tumor cells. To determine whether the cytotoxic T-cell function might be dampened if T cells were treated with cisplatin at the same time as tumor cells, we repeated the experiments but pretreated the T cells with cisplatin prior to adding to the impedance plates with the tumor cells. The results were similar (Supplementary Fig. S1). These results suggest that low doses of cisplatin may upregulate PD-L1 on tumor cells but have only modest effects on T-cell IFNγ production and may enhance antigen-specific T-cell killing of tumor cells.
Figure 2. Cisplatin upregulates PD-L1 on tumor cells, impairs T-cell IFNγ production in a dose-dependent manner, and enhances antigen-specific T-cell killing.
A, HNSCC cells were treated with cisplatin and/or IFNγ and cell surface PD-L1 was measured by flow cytometry. Cell lines: UMSCC-1 (striped), UMSCC-46 (solid black), UMSCC-74A (bricked), and UPCI SCC90 (solid gray). Data are mean + SEM from at least two independent experiments performed in triplicate, * p <0.05, ** p <0.01 vs. untreated, ## p <0.01 vs. IFNγ or CDDP alone, by one-way ANOVA with post-hoc Tukey’s multiple comparison test. B, OT-1 T cells were cultured with or without varying concentrations of cisplatin, then left unstimulated or pulsed with SIINFEKL peptide. A flow cytometry-based IFNγ capture assay was then used to measure production of IFNγ by antigen-specific T cells. Data are mean + SEM from one triplicate experiment, ** p <0.01 vs. stimulated without prior cisplatin by one-way ANOVA with post-hoc Tukey’s multiple comparison test. C–E, Ovalbumin-expressing MOC1 tumor cells (MOC1ova) were allowed to grow in 96-well plates in the presence or absence of cisplatin for 24 hours prior to adding antigen-specific OT-1 T cells (T: target MOC1ova cells and E: effector OT-1 T cells). Impedance measurements were taken over time to determine tumor cell viability. Graphs are representative of two independent experiments done in triplicate. Different doses of CDDP are indicated by color. D and E, Impedance lines are graphed as averages of 3 replicates that have been normalized to a cell index of 1.0 at 26 hours when CTLs were added. CTLs were exposed to cisplatin along with MOC1ova cells starting at 26 hours but were not pretreated with cisplatin.
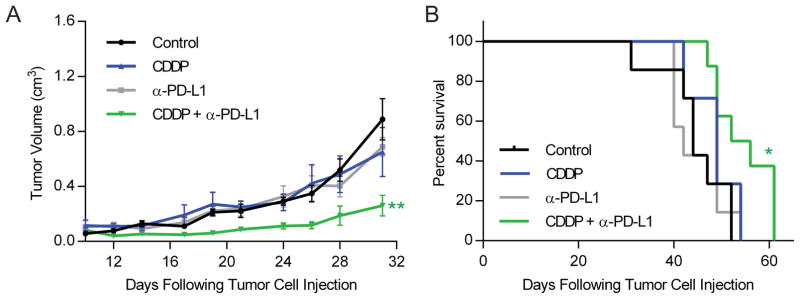
Concurrent treatment with cisplatin and PD-L1/PD-1 blockade delays tumor growth in vivo
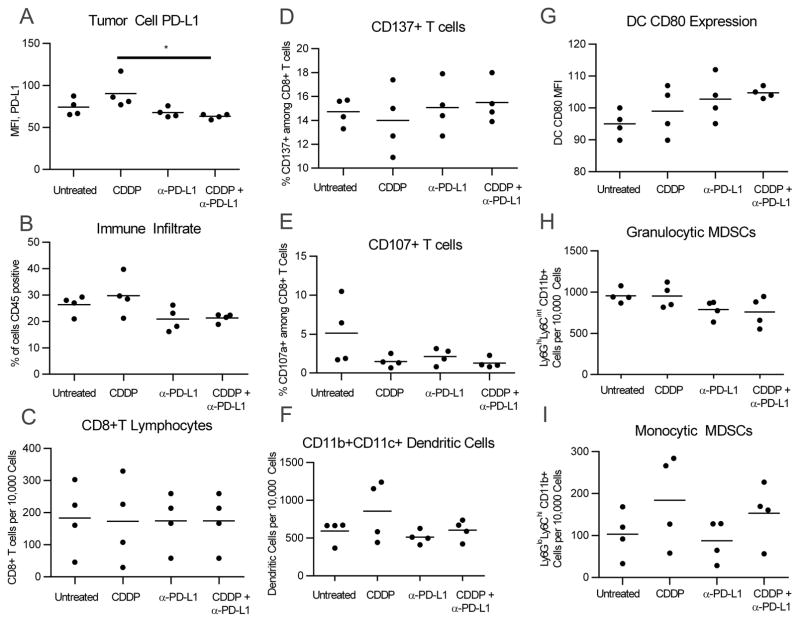
Taken together, the immune-enhancing effects and increased PD-L1 noted with cisplatin in vitro provide a rationale for combined use of cisplatin and PD-L1/PD-1 blockade in vivo. We explored this possibility in mice bearing MOC1 tumors, which typically induce immune responses and respond to immunotherapies, whereas MOC2 tumors, which are aggressive, do not typically induce immune responses and do not respond well to immunotherapies (16, 17, 22, 28). In MOC1-bearing mice, cisplatin (5 mg/kg/week) and anti–PD-L1 did not delay tumor growth when used alone but provided a significant tumor growth delay and prolonged survival when used concurrently (Fig. 3). The tumor growth delay was less pronounced when anti–PD-L1 was combined with a lower dose of cisplatin (3 mg/kg/week; Supplementary Fig. S2). Flow cytometry of tumors from a subset of animals showed that cisplatin did increase tumor cell expression of PD-L1 but did not alter the numbers of CD8+ T cells or other intratumoral immune stimulatory or suppressor cells previously defined in this model (Fig. 4). In contrast, treatment of mice bearing non-immunogenic MOC2 cells with cisplatin induced only a slight and short-lived tumor growth delay with no improvement in survival, and anti–PD-L1 with or without cisplatin did not significantly delay tumor growth (Supplementary Fig. S3), supporting the idea that an underlying antitumor immune response is required for efficacy of cisplatin and anti–PD-L1.
Figure 3. Cisplatin and anti–PD-L1 blockade in combination delayed tumor growth and prolonged survival in MOC1 tumor-bearing mice.
Mice were injected with 5 × 106 MOC1 tumor cells in the right flank. After 11 days, mice with palpable tumors were randomized and treated concurrently with cisplatin (5 mg/kg/week × 4 weeks) and/or anti–PD-L1 antibody (200 mcg twice/week × 3 doses). Black line: control; Blue line: CDDP only; Gray line: anti–PD-L1; Green line: combination. A, Tumor volume over time. Data are mean ± SEM, n = 7–8 mice per group. *p<0.05, **p<0.01 vs. control by linear regression curve comparison B, Kaplan-Meier survival plot. *p<0.05 by log rank (Mantel-Cox) test.
Figure 4. Cisplatin may increase tumor cell PD-L1 expression but does not reduce numbers of CD8+ T lymphocytes in vivo.
Tumors were harvested from a subset of MOC1 tumor-bearing mice at day 25 after tumor cell injection (n = 4 mice per group), five days after the third dose of anti–PD-L1 antibody, and four days following the second weekly dose of cisplatin. Tumor cells and intratumoral immune cells were analyzed by flow cytometry. Data from individual animals and mean are shown. * p <0.05 by two-way ANOVA and post-hoc Tukey’s multiple comparison test.
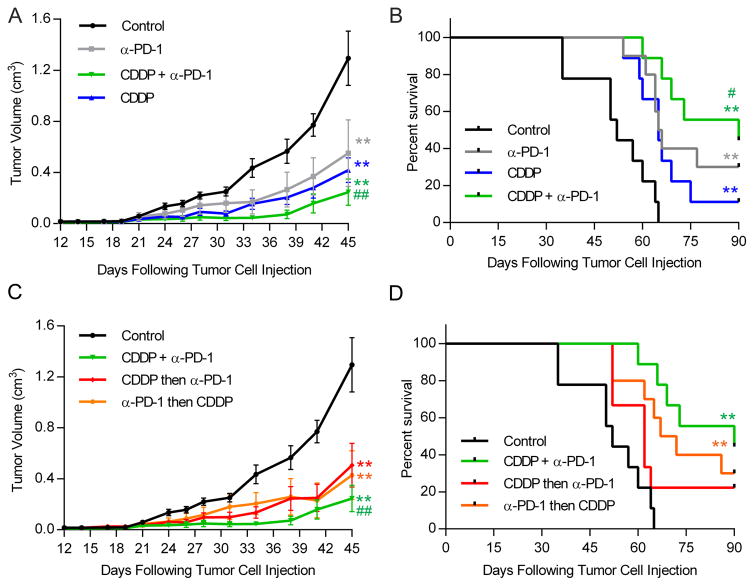
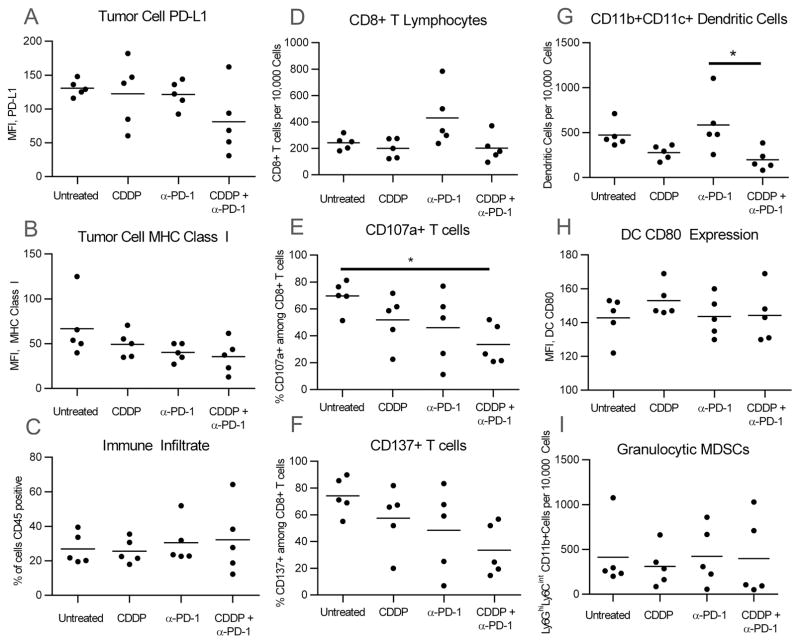
Although combination cisplatin and anti–PD-L1 provided a delay in tumor growth, only three anti–PD-L1 doses could be used to avoid toxicity, and the tumors eventually resumed growing. To see if long-term treatment would be more effective, we treated MOC1-bearing mice with cisplatin and/or an antibody to PD-1, which was better tolerated for up to several weeks in preliminary experiments. A delay in tumor growth when cisplatin and anti–PD-1 were used concurrently was similar to that seen with cisplatin and anti–PD-L1 (Fig. 5A and B), consistent with the limited expression of PD-L2 seen in MOC1 tumors (29). To determine whether the sequence of drug administration would affect tumor growth, additional groups were treated with cisplatin followed by anti–PD-1 one day later, or vice versa, which was not as effective as concurrent use (Fig. 5C and D). Tumors eventually resumed growth toward the end of the treatment period, suggesting that either the anti–PD-1 of heterologous rat origin may be inactivated after a certain number of doses, or the tumors develop resistance mechanisms to cisplatin and/or anti–PD-1 over time. In contrast to tumors analyzed at four days after the second dose of cisplatin, tumors from these experiments analyzed at two days following cisplatin did not show increased PD-L1 (Fig. 6A). As before, the numbers of CD8+ T cells and other intratumoral immune cells did not decrease with cisplatin (Fig. 6). The overall numbers of intratumoral CD8+ T cells and CD11b+ CD11c+ cells (presumed to be dendritic cells) were not decreased in animals treated with cisplatin with or without anti–PD-1 versus controls, but the trend toward increased CD8+ and CD11b+ CD11c+ cells seen with anti–PD-1 alone was lost when cisplatin was added (Fig. 6D and G). Fewer CD8+ T cells were positive for CD107a (Fig. 6E), a marker of functional activation, suggesting some degree of impaired antitumor immunity when cisplatin was added to anti–PD-1.
Figure 5. Concurrent cisplatin and anti–PD-1 blockade delayed tumor growth and prolonged survival in MOC1 tumor-bearing mice.
Mice were injected with 5 × 106 MOC1 tumor cells in the right flank. After 12 days, mice with palpable tumors were randomized and treated concurrently with cisplatin (5 mg/kg/week × 6 weeks) and/or anti–PD-1 antibody (200 mcg twice/week × 6 weeks). A, Tumor volume and B, survival of mice administered cisplatin and anti–PD-1 on the same day. C, Tumor volume and D, survival of mice given cisplatin and anti–PD-1 either started on the same day (Green line) or given in sequence with one day between administrations of the two drugs (Red/Orange lines). Data in A and C are mean ± SEM, n = 9=10 mice per group. **p <0.01 vs. control, #p <0.05 vs. cisplatin treatment alone, ##p <0.01 vs. single-treatment or sequenced treatment groups (vs. concurrent) by linear regression curve comparison for tumor growth and by log rank (Mantel-Cox) test for survival. Data are all from the same experiment and were separated into multiple graphs for clarity.
Figure 6. Cisplatin does not reduce numbers of CD8+ T lymphocytes but may reduce intratumoral dendritic cells in vivo.
Tumors were harvested from a subset of MOC1 tumor-bearing mice (n = 5 mice per group) at day 20 after tumor cell injection, two days after the third dose of anti–PD-1 antibody, and second weekly dose of cisplatin. Tumor cells and intratumoral immune cells were analyzed by flow cytometry. Data from individual animals and mean are shown. *p <0.05 by two-way ANOVA with Tukey’s multiple comparison test.
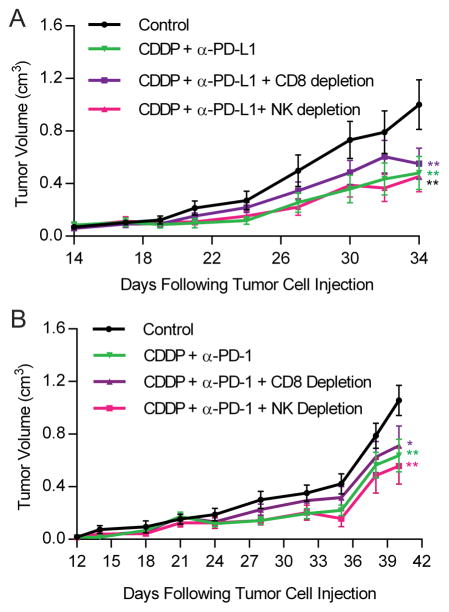
Tumor growth delay by cisplatin and anti-PD-L1/PD-1 involves mechanisms other than CD8+ and NK cells
To elucidate the mechanisms by which cisplatin and PD-L1/PD-1 blockade induce a tumor growth delay in MOC1 tumors in vivo, MOC1-bearing mice were treated with concurrent cisplatin and anti–PD-L1 or anti–PD-1, in addition to antibodies to deplete CD8+ T cells or NK cells. The delay in tumor growth seen with cisplatin and anti–PD-L1 was not significantly altered by depleting CD8+ T cells or NK cells (p = 0.13 for cisplatin plus anti–PD-L1 alone vs. with CD8 depletion; Fig. 7A). When the experiment was repeated using anti–PD-1 instead of PD-L1 antibody, the difference between growth of tumors treated with combination therapy with and without CD8+ T-cell depletion was minimal and, again, not statistically significant (p = 0.28 for cisplatin + anti–PD-1 alone vs. with CD8 depletion; Fig. 7B), but remained significantly different from the control group. Taken together, these results suggest that the antitumor efficacy of cisplatin and PD-L1/PD-1 blockade in this preclinical model depends on mechanisms independent of CD8+ T cells and NK cells.
Figure 7. Antitumor activity of cisplatin and anti–PD-1/PD-L1 may depend in part on CD8+ T cells, but not NK cells.
Mice were injected with 5 × 106 MOC1 tumor cells in the right flank. After 12–14 days, mice with palpable tumors were randomized and treated concurrently with cisplatin (5 mg/kg/week) and either A, anti–PD-L1 or B, anti–PD-1 (200 mcg twice/week). Additional groups were treated with antibodies to deplete CD8+ T cells or NK cells (200 mcg twice/week). Black line: control; Green line: CDDP + anti–PD-L1/PD-1; Purple line: CDDP + anti–PD-L1/PD-1 + CD8 depletion; Fuchsia line: CDDP + anti–PD-L1/PD-1 + NK cell depletion. Data are mean ± SEM. *p <0.05, **p <0.01 vs. control by linear regression curve comparison.
PD-L1/PD-1 blockade does not exacerbate cisplatin-induced toxicities
Cisplatin is known to induce clinically significant toxicity to the inner ear and kidney in susceptible individuals, and this has been reproduced in preclinical animal models (24, 30). Given that cisplatin-induced ototoxicity and nephrotoxicity may involve inflammatory cytokines (30), the use of immunotherapy could theoretically worsen these toxicities seen frequently with cisplatin. To investigate this possibility, kidney histology following 6 weeks of treatment in MOC1-bearing mice was compared across treatment groups, and none of the kidneys exhibited histologic signs of cisplatin toxicity (Supplementary Fig. S4A). Hearing tests performed on mice treated with 6 weekly doses of cisplatin showed no evidence of hearing impairment compared with untreated mice of the same age (Supplementary Fig. S4B and C).
DISCUSSION
An expanding series of studies suggest that cytotoxic chemotherapy may be immunogenic. It has been suggested that cisplatin may enhance host immunity in several tumor types by upregulating MHC class I and other components of the antigen processing machinery by inducing components of immunogenic cell death and by increasing the ratio of immune effector to immunosuppressive cells in the tumor microenvironment (7, 8, 31). However, cisplatin is known to reduce numbers of circulating immune cells, suggesting it can be directly toxic to immune cells. Tumor cells treated with cytotoxic drugs may upregulate immune checkpoint ligands as a form of immune escape (11, 12). In the current study, we employed preclinical models of head and neck cancer to show that cisplatin may enhance antitumor adaptive immunity by upregulating antigen processing machinery and enhancing tumor cell killing by CD8+ T cells without decreasing T-cell numbers. However, consistent with findings in other tumor types treated with cytotoxic drugs, we found that exposure to cisplatin caused tumor cells to upregulate surface levels of PD-L1. This PD-L1 increase occurred in vitro after 48 hours but was only seen in vivo after four days; PD-L1 was not increased in tumors from cisplatin-treated animals after two days.
Our data suggest that the balance of immune-enhancing and immunosuppressive effects of cisplatin in HNSCC may be dose-dependent. The increase in several APM components examined was seen at sublethal doses in vitro, and these doses are all below the peak serum concentration seen in patients treated with cisplatin at a high dose of 100 mg/m2 (27). The APM changes included increases in both HLA-ABC/MHC class I and multiple chaperone proteins, which are critical for antigen processing and presentation to T cells. There were additive increases in APM components in one cell line treated with both IFNγ and cisplatin, suggesting that cisplatin may enhance IFNγ-induced antigen processing in some situations. Increases in TAP1/2 were only noted in the cell line with wildtype TP53, but not in HPV-positive cells or HPV-negative cells with mutated TP53. Dependence of TAP1 expression on functional p53 has been reported (32). Because the majority of tumors harbor TP53 mutations or HPV oncoproteins, which inactivate p53 (33), this finding suggests that the inability to increase TAP1/2 may be a form of immune escape in HNSCC. Cisplatin treatment of HNSCC cells also activates STAT1 (34), which may also be needed for maximized expression of APM components in addition to p53 (32, 35–37). Thus, differences in p53 and STAT1 expression may, in part, explain the variability in APM component expression following cisplatin treatment in different HNSCC tumors or cell lines.
Although increases in PD-L1 were also noted at relatively low doses, substantial impairment of IFNγ production by T cells was seen at higher doses, which are achieved only briefly in the plasma of patients treated with the highest dose used for HNSCC (100 mg/m2) (3, 4, 27). In our mouse experiments, we noted that the maximum tolerated dose of cisplatin (5 mg/kg/week, based on prior experiments) provided a more pronounced tumor growth delay when paired with anti–PD-L1 than a lower dose (3 mg/kg/week). Although the higher dose did not reduce numbers of CD8+ T cells compared with untreated animals, tumors from animals treated with cisplatin and anti–PD-1 did not show robust increases in CD8+ T cells that we have previously seen animals treated with anti–PD-1 alone. A similar effect on CD107+ T cells was seen with combined cisplatin and anti–PD-L1/PD-1, suggesting that T-cell degranulation may be impaired as well. Taken together, these data suggest that there may be an optimal dose of cisplatin that enhances antigen presentation and T-cell activation without inducing untoward effects on T-cell numbers or function. However, our in vivo depletion studies suggest that the effects of the combination are to some degree dependent on mechanisms other than CD8+ T cells in this chemically induced HNSCC model. Another study in a syngeneic mouse model of HPV-related HNSCC found a delay in tumor growth with cisplatin that was not seen in Rag-1 mice lacking functional T and B cells (38), suggesting that T cells may be important for the maximal response to cisplatin chemotherapy in that model.
It is possible that cisplatin may enhance antitumor immunity in other ways, such as by inducing immunogenic cell death (ICD) or by reducing the number or function of immunosuppressive cells in the tumor microenvironment. Although cisplatin is thought to be a poor inducer of ICD compared with oxaliplatin and other chemotherapy drugs (39), data from our laboratory suggest that cisplatin induces all of the classic markers of ICD in preclinical models of HSNCC (40). A prior study with murine and human data showed that chemotherapy (carboplatin and paclitaxel) reduces numbers of immunosuppressive MDSCs in cervical cancer (41). Although the MOC1 model is largely driven by MDSCs (28), we did not see any differences in MDSC numbers in tumors from cisplatin-treated mice in our study, though we did not look at multiple time points or perform functional studies.
A study published while our experiments were underway explored immune effects of cisplatin in combination with a different checkpoint inhibitor, anti–CTLA-4, in HPV-transformed lung and embryonic cell models that are far more sensitive to cisplatin monotherapy (31). The authors found that the tumor growth delay induced by cisplatin alone was largely attenuated by depleting CD8+ T cells, a relationship that was not clearly seen in our study. The authors also noted that the effects of cisplatin were highly dependent on activation of dendritic cells, with cisplatin inducing increases in CD70, CD80, and CD86 on myeloid cells; cisplatin was also less effective in animals lacking these costimulatory molecules (31). In our study, we saw a trend toward increased CD80 on dendritic cells with cisplatin, but this did not reach statistical significance. The authors were able to clear tumors in mice when cisplatin was combined with blockade of CTLA-4. The effects of PD-1/PD-L1 blockade were not investigated in that study (31). CTLA-4 has been noted to play a greater role in blocking development of new T-cell responses, whereas PD-L1 promotes exhaustion of established responses (42, 43). Together, these studies suggest that combinations of cisplatin with PD-L1/PD-1 and CTLA-4 immune checkpoint inhibitors merit further investigation.
The findings in our study are timely and pertinent, due to the FDA approval of anti–PD-1 antibodies and paradigm shifts in dosing of cisplatin in the treatment of HNSCC. The traditional regimen for treatment of both nonsurgical and surgical HNSCC patients was to administer cisplatin doses of 100 mg/m2 every three weeks for a total of three doses with concurrent radiation, based on large clinical trials showing that cisplatin given in this fashion improves survival (3, 4). However, providers have begun to administer weekly doses of 40 mg/m2 for a total of 6–7 doses, despite the lack of large, prospective clinical trials comparing the efficacy of this regimen to the more traditional regimen (44, 45). Retrospective trials suggest that the low-dose, weekly regimen may be equivalent and better tolerated, and many centers around the world have shifted to this regimen (44, 45). It is unclear which of these cisplatin dosing strategies might be more immunogenic. Our in vivo data suggest that concurrent administration of these agents may be more effective than administering cisplatin prior to checkpoint inhibitors or vice versa. Several clinical trials combining cisplatin with checkpoint inhibitors for HNSCC are underway. Correlative immune studies and toxicity data from these trials could help elucidate the best way to combine these agents in order to maximize antitumor immunity without excess toxicity.
This study has several limitations, including our inability to detect subtle changes in numbers and phenotype of immune cells of the tumor microenvironment by flow cytometry of tumors from a relatively small number of animals. It is also unclear how the doses of cisplatin and anti–PD-1/PD-L1 that we used compare to doses used clinically, as we were unable to find good pharmacokinetic data for cisplatin-treated mice. However, we did perform preliminary experiments to establish a dose of cisplatin that is relatively well tolerated when given weekly over several weeks as is done in HNSCC patients, and we used doses of anti–PD-1/PD-L1 that have been established to dampen PD-1 responses. We also attempted to determine whether known toxicities of cisplatin to the inner ear and kidney would be worsened by PD-1 blockade, which could theoretically exacerbate the inflammatory changes seen in these toxicities. Our cisplatin treatment paradigm, however, did not induce any hearing loss or detectable changes in kidney histology. Experiments are currently underway in a mouse model known to cause cisplatin-induced hearing loss (24), in order to determine whether the inner ear toxicity may be exacerbated by adding twice-weekly anti–PD-1 antibody.
In summary, cisplatin chemotherapy given at an optimal dose may enhance adaptive antitumor immunity with minimal effects on the numbers or function of effector immune cells in the tumor microenvironment or cisplatin-related toxicities. Cisplatin may also cause upregulation of tumor cell PD-L1, which may in part explain the additive antitumor activity of cisplatin and PD-L1/PD-1 blockade. This information will help in interpreting results of ongoing clinical trials combining these agents, and for comparison of potential future therapeutic combinations for the treatment of head and neck cancer.
Supplementary Material
Acknowledgments
Financial Support: Supported (in part) by the Intramural Research Program of the NIH, NIDCD, projects ZIA-DC-DC000087, ZIA-DC-DC000090, and ZIC DC000080.
The authors would like to acknowledge Christopher Silvin for flow cytometry assistance, Megan Morisada for technical assistance with figures, and Jeffrey Schlom, James Hodge, and Zhong Chen for feedback on the project and manuscript.
Footnotes
Conflict of Interest Disclosure: Dr. Van Waes and Dr. Schmitt have received research funding from Astex Pharmaceuticals.
References
- 1.Moy JD, Moskovitz JM, Ferris RL. Biological mechanisms of immune escape and implications for immunotherapy in head and neck squamous cell carcinoma. Eur J Cancer. 2017;76:152–66. doi: 10.1016/j.ejca.2016.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferris RL. Immunology and Immunotherapy of Head and Neck Cancer. J Clin Oncol. 2015;33:3293–304. doi: 10.1200/JCO.2015.61.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernier J, Domenge C, Ozsahin M, Matuszewska M, Lefebvre J, Greiner R, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350:1945–52. doi: 10.1056/NEJMoa032641. [DOI] [PubMed] [Google Scholar]
- 4.JSC, TFP, AAF, JJ, BHC, SVS, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350:1937–44. doi: 10.1056/NEJMoa032646. [DOI] [PubMed] [Google Scholar]
- 5.Ferris RL, Blumenschein G, Jr, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2016;375:1856–67. doi: 10.1056/NEJMoa1602252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, Eder JP, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. The Lancet Oncology. 2016;17:956–65. doi: 10.1016/S1470-2045(16)30066-3. [DOI] [PubMed] [Google Scholar]
- 7.de Biasi AR, Villena-Vargas J, Adusumilli PS. Cisplatin-induced antitumor immunomodulation: a review of preclinical and clinical evidence. Clin Cancer Res. 2014;20:5384–91. doi: 10.1158/1078-0432.CCR-14-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hato SV, Khong A, de Vries IJ, Lesterhuis WJ. Molecular pathways: the immunogenic effects of platinum-based chemotherapeutics. Clin Cancer Res. 2014;20:2831–7. doi: 10.1158/1078-0432.CCR-13-3141. [DOI] [PubMed] [Google Scholar]
- 9.Gelbard A, Garnett CT, Abrams SI, Patel V, Gutkind JS, Palena C, et al. Combination chemotherapy and radiation of human squamous cell carcinoma of the head and neck augments CTL-mediated lysis. Clin Cancer Res. 2006;12:1897–905. doi: 10.1158/1078-0432.CCR-05-1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hodge JW, Garnett CT, Farsaci B, Palena C, Tsang KY, Ferrone S, et al. Chemotherapy-induced immunogenic modulation of tumor cells enhances killing by cytotoxic T lymphocytes and is distinct from immunogenic cell death. Int J Cancer. 2013;133:624–36. doi: 10.1002/ijc.28070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peng J, Hamanishi J, Matsumura N, Abiko K, Murat K, Baba T, et al. Chemotherapy Induces Programmed Cell Death-Ligand 1 Overexpression via the Nuclear Factor-kappaB to Foster an Immunosuppressive Tumor Microenvironment in Ovarian Cancer. Cancer Res. 2015;75:5034–45. doi: 10.1158/0008-5472.CAN-14-3098. [DOI] [PubMed] [Google Scholar]
- 12.Van Der Kraak L, Goel G, Ramanan K, Kaltenmeier C, Zhang L, Normolle DP, et al. 5-Fluorouracil upregulates cell surface B7-H1 (PD-L1) expression in gastrointestinal cancers. J Immunother Cancer. 2016;4:65. doi: 10.1186/s40425-016-0163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brenner JC, Graham MP, Kumar B, Saunders LM, Kupfer R, Lyons RH, et al. Genotyping of 73 UM-SCC head and neck squamous cell carcinoma cell lines. Head Neck. 2010;32:417–26. doi: 10.1002/hed.21198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gollin SM. Cytogenetic alterations and their molecular genetic correlates in head and neck squamous cell carcinoma: a next generation window to the biology of disease. Genes Chromosomes Cancer. 2014;53:972–90. doi: 10.1002/gcc.22214. [DOI] [PubMed] [Google Scholar]
- 15.White JS, Weissfeld JL, Ragin CC, Rossie KM, Martin CL, Shuster M, et al. The influence of clinical and demographic risk factors on the establishment of head and neck squamous cell carcinoma cell lines. Oral Oncol. 2007;43:701–12. doi: 10.1016/j.oraloncology.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cash H, Shah S, Moore E, Caruso A, Uppaluri R, Van Waes C, et al. mTOR and MEK1/2 inhibition differentially modulate tumor growth and the immune microenvironment in syngeneic models of oral cavity cancer. Oncotarget. 2015;6:36400–17. doi: 10.18632/oncotarget.5063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore E, Clavijo PE, Davis R, Cash H, Van Waes C, Kim Y, et al. Established T Cell-Inflamed Tumors Rejected after Adaptive Resistance Was Reversed by Combination STING Activation and PD-1 Pathway Blockade. Cancer Immunol Res. 2016;4:1061–71. doi: 10.1158/2326-6066.CIR-16-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moynihan KD, Opel CF, Szeto GL, Tzeng A, Zhu EF, Engreitz JM, et al. Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses. Nat Med. 2016;22:1402–10. doi: 10.1038/nm.4200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duraiswamy J, Freeman GJ, Coukos G. Therapeutic PD-1 pathway blockade augments with other modalities of immunotherapy T-cell function to prevent immune decline in ovarian cancer. Cancer Res. 2013;73:6900–12. doi: 10.1158/0008-5472.CAN-13-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guillerey C, Ferrari de Andrade L, Vuckovic S, Miles K, Ngiow SF, Yong MC, et al. Immunosurveillance and therapy of multiple myeloma are CD226 dependent. J Clin Invest. 2015;125:2077–89. doi: 10.1172/JCI77181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L, Gajewski TF, Kline J. PD-1/PD-L1 interactions inhibit antitumor immune responses in a murine acute myeloid leukemia model. Blood. 2009;114:1545–52. doi: 10.1182/blood-2009-03-206672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore EC, Cash HA, Caruso AM, Uppaluri R, Hodge JW, Van Waes C, et al. Enhanced Tumor Control with Combination mTOR and PD-L1 Inhibition in Syngeneic Oral Cavity Cancers. Cancer Immunol Res. 2016;4:611–20. doi: 10.1158/2326-6066.CIR-15-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Francis SP, Kramarenko II, Brandon CS, Lee FS, Baker TG, Cunningham LL. Celastrol inhibits aminoglycoside-induced ototoxicity via heat shock protein 32. Cell Death Dis. 2011;2:e195. doi: 10.1038/cddis.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roy S, Ryals MM, Van den Bruele AB, Fitzgerald TS, Cunningham LL. Sound preconditioning therapy inhibits ototoxic hearing loss in mice. J Clin Invest. 2013;123:4945–9. doi: 10.1172/JCI71353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradford CR, Zhu S, Ogawa H, Ogawa T, Ubell M, Narayan A, et al. P53 mutation correlates with cisplatin sensitivity in head and neck squamous cell carcinoma lines. Head Neck. 2003;25:654–61. doi: 10.1002/hed.10274. [DOI] [PubMed] [Google Scholar]
- 26.Zhu K, Wang J, Zhu J, Jiang J, Shou J, Chen X. p53 induces TAP1 and enhances the transport of MHC class I peptides. Oncogene. 1999;18:7710–47. doi: 10.1038/sj.onc.1203235. [DOI] [PubMed] [Google Scholar]
- 27.Go R, Adjei A. Review of the comparative pharmacology and clinical activity of cisplatin and carboplatin. J Clin Oncol. 1999;17:409–22. doi: 10.1200/JCO.1999.17.1.409. [DOI] [PubMed] [Google Scholar]
- 28.Davis RJ, Moore EC, Clavijo PE, Friedman J, Cash HA, Chen Z, et al. Anti-PD-L1 efficacy can be enhanced by inhibition of myeloid derived suppressor cells with a selective inhibitor of PI3Kdelta/gamma. Cancer Res. 2017 doi: 10.1158/0008-5472.CAN-16-2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah S, Caruso A, Cash H, Waes CV, Allen CT. Pools of programmed death-ligand within the oral cavity tumor microenvironment: Variable alteration by targeted therapies. Head Neck. 2016;38:1176–86. doi: 10.1002/hed.24269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmitt NC, Rubel EW. Osteopontin does not mitigate cisplatin ototoxicity or nephrotoxicity in adult mice. Otolaryngol Head Neck Surg. 2013;149:614–20. doi: 10.1177/0194599813498218. [DOI] [PubMed] [Google Scholar]
- 31.Beyranvand Nejad E, van der Sluis TC, van Duikeren S, Yagita H, Janssen GM, van Veelen PA, et al. Tumor Eradication by Cisplatin Is Sustained by CD80/86-Mediated Costimulation of CD8+ T Cells. Cancer Res. 2016;76:6017–29. doi: 10.1158/0008-5472.CAN-16-0881. [DOI] [PubMed] [Google Scholar]
- 32.Zhu K, Wang J, Zhu J, Jiang J, Shou J, Chen X. p53 induces TAP1 and enhances the transport of MHC class I peptides. Oncogene. 1999;18:7740–7. doi: 10.1038/sj.onc.1203235. [DOI] [PubMed] [Google Scholar]
- 33.Cancer Genome Atlas N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature. 2015;517:576–82. doi: 10.1038/nature14129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmitt NC, Trivedi S, Ferris RL. STAT1 Activation Is Enhanced by Cisplatin and Variably Affected by EGFR Inhibition in HNSCC Cells. Mol Cancer Ther. 2015;14:2103–11. doi: 10.1158/1535-7163.MCT-15-0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leibowitz MS, Andrade Filho PA, Ferrone S, Ferris RL. Deficiency of activated STAT1 in head and neck cancer cells mediates TAP1-dependent escape from cytotoxic T lymphocytes. Cancer Immunol Immunother. 2011;60:525–35. doi: 10.1007/s00262-010-0961-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leibowitz MS, Srivastava RM, Andrade Filho PA, Egloff AM, Wang L, Seethala RR, et al. SHP2 is overexpressed and inhibits pSTAT1-mediated APM component expression, T-cell attracting chemokine secretion, and CTL recognition in head and neck cancer cells. Clin Cancer Res. 2013;19:798–808. doi: 10.1158/1078-0432.CCR-12-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Srivastava RM, Trivedi S, Concha-Benavente F, Hyun-Bae J, Wang L, Seethala RR, et al. STAT1-Induced HLA Class I Upregulation Enhances Immunogenicity and Clinical Response to Anti-EGFR mAb Cetuximab Therapy in HNC Patients. Cancer Immunol Res. 2015;3:936–45. doi: 10.1158/2326-6066.CIR-15-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spanos WC, Nowicki P, Lee DW, Hoover A, Hostager B, Gupta A, et al. Immune response during therapy with cisplatin or radiation for humnan papillomavirus-related head and neck cancer. Arch Otolaryngol Head Neck Surg. 2009;135:1137–46. doi: 10.1001/archoto.2009.159. [DOI] [PubMed] [Google Scholar]
- 39.Terenzi A, Pirker C, Keppler BK, Berger W. Anticancer metal drugs and immunogenic cell death. J Inorg Biochem. 2016;165:71–9. doi: 10.1016/j.jinorgbio.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 40.Park SJ, Tran L, Xiao R, Van Waes C, Schmitt NC. Cisplatin induces immunogenic cell death in preclinical models of head and neck squamous cell carcinoma. Annual Meeting of the Society for Immunotherapy of Cancer; National Harbor, MD. 2017. Abstract P377. [Google Scholar]
- 41.Welters MJ, van der Sluis TC, van Meir H, Loof NM, van Ham VJ, van Duikeren S, et al. Vaccination during myeloid cell depletion by cancer chemotherapy fosters robust T cell responses. Sci Transl Med. 2016;13:334ra52. doi: 10.1126/scitranslmed.aad8307. [DOI] [PubMed] [Google Scholar]
- 42.Ott PA, Hodi FS, Kaufman HL, Wigginton JM, Wolchok JD. Combination immunotherapy: a road map. J Immunother Cancer. 2017;5:16. doi: 10.1186/s40425-017-0218-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Driessen CM, Uijen MJ, van der Graaf WT, van Opstal CC, Kaanders JH, Nijenhuis T, et al. Degree of nephrotoxicity after intermediate- or high-dose cisplatin-based chemoradiotherapy in patients with locally advanced head and neck cancer. Head Neck. 2016;38(Suppl 1):E1575–81. doi: 10.1002/hed.24281. [DOI] [PubMed] [Google Scholar]
- 45.Osman N, Elamin YY, Rafee S, O’Brien C, Stassen LF, Timon C, et al. Weekly cisplatin concurrently with radiotherapy in head and neck squamous cell cancer: a retrospective analysis of a tertiary institute experience. Eur Arch Otorhinolaryngol. 2014;271:2253–9. doi: 10.1007/s00405-013-2749-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.