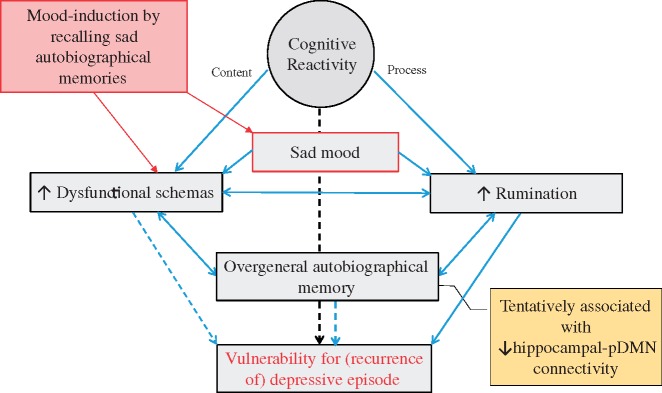
Fig. 3.
Proposed relations between recalling sad autobiographical memories, cognitive risk factors and risk of recurrence in remitted MDD. Lines and arrows indicate directions of relations, dotted lines represent directions for which evidence is not unequivocal. Recalling sad autobiographical memories leads to induction of sad mood, which increases dysfunctional schemas and activates rumination [cognitive reactivity (CR); Koster et al., 2011; Lau et al., 2004]. As negative autobiographical memories fit with dysfunctional schemas, sad autobiographical memory recall itself also leads to increase in dysfunctional schemas (Raes et al., 2012). The activation of dysfunctional schemas facilitates a ruminative-state: individuals are unable to disengage from negative, ruminative thoughts, as these are congruent with activated schemas (Koster et al., 2011). Rumination is a causal factor of Over-general autobiographical memory (OAM): it interferes with the retrieval of specific memories (Sumner, 2012). OAM can also strengthen rumination (Sumner, 2012). Further, OAM, aggravated by rumination, reinforces the completion of thinking patterns by abstract representations, as dysfunctional schemas (Belzung et al., 2015). CR refers to both the content of thoughts (dysfunctional schema's) as well as the process (rumination) invoked by sad mood (Lau et al., 2004; Raes et al., 2012). CR and dysfunctional schema's have been identified as risk-factors for recurrence, although evidence is mixed (Figueroa et al., 2015, van Rijsbergen et al., 2013). Rumination has been identified as an important risk-factor for recurrence (Michalak et al., 2011). OAM has been associated with new episodes (Sumner, 2012) though reports of OAM as a risk-factor for recurrence vary (Spinhoven et al., 2006). We hypothesize that all these processes act together, and are associated with abberant hippocampal-DMN connectivity, to increase risk of depressive recurrence.