Abstract
Background
To describe and examine the distribution, disability, and treatment associated with comorbid cardiovascular disease and major depressive disorder (CVD/MDD) among middle-aged and older ethnic/racial groups in the United States.
Methods
Cross-sectional data from a national probability sample of household resident adults (18 years and older; N = 16,423) living in the 48 coterminous United States were analyzed. We defined comorbid CVD/MDD as the presence of CVD (e.g. diabetes, hypertension, heart disease, and stroke) among adults who met MDD criteria at or after age 50 years.
Results
Two-thirds of middle-aged and older American adults meeting criteria major depression at or after age 50 years also reported a diagnosis of comorbid CVD. Blacks were most likely to meet our comorbid CVD/MDD (74.4%) criteria. The disease burden of depression was also highest among Black respondents. Differences in treatment due to race/ethnicity and comorbidity were not statistically significant.
Conclusions
Our findings indicate that among middle-aged and older US adults meeting MDD criteria more than half would also report a comorbid CVD. Comorbid CVD/MDD rates varied between the considered ethnic/race groups. Functional impairment associated with comorbid CVD/MDD was higher than MDD alone; however, depression care rates did not differ remarkably. Among middle-aged and older adults meeting MDD criteria, comorbid CVD may be the rule rather than the exception.
Keywords: major depressive disorder, depression, epidemiology, cardiovascular disease, heart disease, stroke
Introduction
Major depression often coexists with a variety of chronic health problems and cardiovascular disease (CVD; Goodwin et al., 2009). It has been posited that CVD can “predispose, precipitate, or perpetuate a depressive syndrome in older adults (Alexopoulos, 2006, p. 1304).” Depression is found in roughly half of all patients following stroke, which often complicates rehabilitation and negatively impacts the individual’s quality of life (Whyte and Mulsant, 2002). While it is likely that the depression is an emotional response to life changes associated with chronic health problems or acute and subacute cardiovascular and cerebrovascular disease (George, 1994). It has been suggested that those biological changes may also directly contribute to depressive symptoms (Frasure-Smith et al., 1993). Regardless of the causal or temporal relationship between CVD and major depressive disorder (MDD), both disorders are chronic, common, and disabling, and pose additional challenges to patients and care providers. Furthermore, the disease burden associated with comorbid CVD and MDD would be expected to be higher than either condition acting independently.
Cardiovascular disease (i.e. diabetes, hypertension, reported heart disease, and stroke) and MDD are major public health problems in the United States (Roger et al., 2011). Yet, limited epidemiologic information is available about the prevalence of comorbid CVD and MDD (Goodwin et al., 2009). Furthermore, since CVD emerges in middle age, the one general adult population estimate may be relative to middle-aged and older adults meeting major depression criteria. Additionally, since CVD is reportedly disproportionately higher among ethnic/racial minorities, understanding CVD and MDD comorbidity distributions among diverse groups of Americans assumes importance. Second, if the comorbid CVD and MDD vary markedly between ethnic/racial groups, we could anticipate disability differences between groups. In this study, we describe and examine the distribution of comorbid CVD and MDD among middle-aged and older ethnic/racial groups in the United States. To do so, we use publically available data from a nationally representative psychiatric survey.
Methods
Data
We used data from the National Institute of Mental Health Collaborative Psychiatric Epidemiology Surveys (CPES). The CPES sample combines three national surveys with common sampling designs and objectives: the National Comorbidity Survey Replication (NCS-R), the National Study of American Life (NSAL), and the National Latino and Asian American Study of Mental Health (NLAAS). Briefly, the survey items by design and to the extent possible were “harmonized” to ensure sample comparability. Detailed methods and procedures used to integrate the individual CPES studies can be found elsewhere (Hartley, 1974; Heeringa et al., 2004; Pennell et al., 2004). The CPES included detailed national information on mental health disorders and their associated disease burden among ethnic and racial adult populations in the United States. The final CPES sample included a complex multistage area probability design with sampling weights to correct for unequal probability of selection and non-response bias and allow for appropriate population-level inferences. The CPES data were collected between February 2001 and November 2003 using face-to-face interviews. The final CPES response rate was 72.3%.
Analyses of ethnic/racial groups
The main foci of this study were to examine and describe the distribution of comorbid CVD/MDD, particularly among ethnic/racial minorities, and associated disability among US adults 50 years and older. All analytic procedures and estimated parameters for the subpopulations of interest were derived using survey sampling specific techniques in the Stata 11.2 statistical software. Wayne State University’s institutional review board approved the analysis of this de-identified, publicly available dataset.
Measures
Ethnicity/race was based on respondents’ self-classification into one of five groupings including: Cuban, Puerto Rican, Mexican, Black (African American or Caribbean-origin), and non-Latino Whites.
Comorbid CVD/MDD
Our main interest was in comorbid CVD/MDD occurring at or after the age of 50 years. We chose 50 years since many risk factors for CVD and acute CVD reportedly emerge during midlife (Cutler et al., 2008). Depressive disorders were assessed using Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV), World Mental Health (WMH)-Composite International Diagnostic Interview (CIDI) criteria (American Psychiatric Association, 2000). Depression recency was measured using self-reported age (in years) of the most recent major depressive episode.
A comorbid CVD/MDD classification was benchmarked using two conditions including: (1) meeting criteria for a lifetime MDD with a depressive episode occurring at age 50 years or older; and (2) self-reported medical diagnoses of one or more cerebrovascular disease risk factor including diabetes, hypertension or disease, specifically heart disease or stroke.
A trichotomous indicator was generated to identify three groups of interest. Our first category included respondents not meeting criteria for MDD at or after the age of 50 years. A second category included respondents that met criteria for mid-and late-life depression without the CVD (i.e. specified above). Finally, a third category included all individuals meeting criteria for comorbid CVD/MDD (i.e. age 50 years and older).
Days of functional impairment
To quantify functional impairment, we used the World Health Organization Disability Assessment Scale (WHODAS-II), which is a global measure of disability that combines self-reported 30-day impairment across five functional domains (World Health Organization, 2001). The WHODAS-II is based on the self-reported number of days out of role in: (1) overall role impairment, (2) cognition, (3) mobility, (4) self-care, and (5) social impairment (World Health Organization, 2001). Given the common metric of the WHODAS-II domains, an average disability score was calculated by summing the reported impairment days across the individual domains and dividing by the number of domains considered. The range of the resulting index was between 0 and 30.
Depression care
We examined three measures of treatment including pharmacotherapy, psychotherapy, and any therapy (i.e. either pharmacotherapy or psychotherapy). All three measures were coded dichotomously to distinguish treated and untreated respondents. Pharmacological treatment was assessed using registries of generic and trade name prescriptions collected during the interviews and respondents’ reports of prescribing sources. Coding for antidepressant drug use was done following a detailed review and verification process of the collected prescription registries by two board-certified psychiatrists and a psychiatric nurse specialist. Assessment of psychotherapy was based on respondents’ self-reports of treatment by a mental health professional including by a psychiatrist, psychologist, counselor, or social worker.
Other variables
Because age and sex proportions vary by ethnicity/race, we included them as covariates in the multivariate models. Both age (0 = 50–64, 1 = 65+) and sex (0 = Female, 1 = Male) were measured as dichotomous indicators.
Statistical approach
Our analysis was conducted using version 11.2 of the Stata statistical software package. We used a Taylor Series Linearization approach to variance estimation in Stata’s complex survey procedures to generate corrected standard errors and ensure appropriate population inferences. All analysis appropriately considered the CPES’ probability weights to allow for adequate representation of the population of interest.
First, we presented univariate descriptive statistics of the demographic characteristics of the study’s subpopulation. Second, we generated ethnic/racial group-specific prevalence estimates of mid- and late-life depression and comorbid CVD/MDD. Survey adjusted χ2 tests were subsequently calculated to test for overall independence between depression classification and ethnicity/race. Third, we used logistic regression models to test the odds of comorbid CVD/MDD classification among ethnic/racial groups relative to non-Latino Whites controlling for age and sex. Fourth, we modeled impairment rates as a function of ethnicity/race and depression grouping controlling for age and sex. Given that the outcome represents a count of days impaired, distributional functions appropriate for non-negatively skewed outcomes are considered. To avoid the possible violation of the stringent assumption of conditional equidispersion imposed by the Poisson distribution (Cameron and Trivedi, 2010), we use a negative binomial regression model to test the main and interaction effects of comorbid CVD/MDD and ethnicity/race on impairment days adjusting for age and sex. To facilitate the interpretation of model parameters, we present the incidence rate ratios and their 95% confidence intervals (CI), and graph ethnic/race and depression-type specific estimated counts of days impaired and their CI. Fifth, we used logistic regressions to model the relationship between treatment type, ethnicity/race and comorbidity controlling for age and sex, and present the odds ratios (OR) of treatment and their 95% CI. Survey-adjusted Wald tests were used to test all linear hypotheses on the multivariate regression coefficients. To safeguard against the risk of finding incidental significance, Bonferroni adjustments were used when post hoc multiple hypotheses testing were conducted. The analytical sample consisted of 4,281 respondents with 528 individuals meeting criteria for a major depressive episode occurring at or over the age of 50 years. Of these 528 respondents, 29 cases had missing observations on the impairment indicators and were excluded from the corresponding analysis.
Results
Descriptive statistics
Sample characteristics for the ethnic/race subpopulations of interest are presented in Table 1. Among the ethnic/racial groups considered, Blacks had the lowest proportion of males; however, the overall group proportions did not differ significantly. Cubans and non-Latino Whites were older relative to the other groups. Puerto Ricans presented the highest prevalence of MDD, while Black respondents were least likely to meet MDD criteria. There were significant differences in the self-reported CVD factors examined in this study (Table 1), except for heart disease. Diabetes was reportedly higher among Puerto Ricans, Mexican Americans, and Blacks, respectively. Hypertension was highest among Black and Cuban respondents, respectively. Stroke was reportedly highest among Blacks. Overall, Black respondents had the highest CVD morbidity levels with close to two-thirds (65.4%) reporting one or more of the CVD factors considered herein.
Table 1.
Sample characteristics of respondents 50 years and older by ethnic/race grouping
| CUBANS %(SE)a | PUERTO RI CANS %(SE)a | MEXICANS %(SE)a | BLACKS %(SE)a | WHITES %(SE)a | TOTAL %(SE)a | ||
|---|---|---|---|---|---|---|---|
| Male | 50.91(2.58) | 51.23(2.77) | 48.8(5.31) | 43.48(1.45) | 45.18(2.16) | 45.24(1.83) | p = 0.5121 |
| Age (years) | |||||||
| 50–64 | 52.41(3.69) | 66.41(7.79) | 64.66(4.66) | 61.48(1.45) | 54.95(2.35) | 56.04(1.99) | p = 0.0288 |
| 65+ | 47.59(3.69) | 33.59(7.79) | 35.34(4.66) | 38.52(1.45) | 45.05(2.35) | 43.96(1.99) | |
| Middle-aged and older MDDb | 13.47(1.19) | 20.23(4.47) | 10.54(2.59) | 6.50(0.65) | 10.31(0.92) | 10.03(0.79) | p < 0.01 |
| Self-reported cardiovascular disease and risk factors | |||||||
| Diabetes | 14.6(3.31) | 29.05(5.63) | 24.73(4.01) | 22.49(1.12) | 12.47(0.97) | 14.04(0.84) | p < 0.01 |
| Hypertension | 52.76(2.66) | 48.20(3.65) | 43.02(4.39) | 62.05(1.67) | 42.55(1.14) | 44.51(0.99) | p < 0.01 |
| Heart disease | 17.87(2.57) | 22.12(3.68) | 11.69(3.38) | 16.36(1.36) | 15.04(1.48) | 15.11(1.30) | p = 0.3721 |
| Stroke | 0.63(0.47) | 1.07(0.66) | 4.27(1.18) | 7.46(0.91) | 5.21(0.72) | 5.32(0.62) | p = 0.0186 |
| Any CVD | 60.62(2.59) | 58.17(4.76) | 52.33(5.03) | 65.43(1.39) | 52.9(1.32) | 54.2(1.14) | p < 0.01 |
Weighted prevalence and survey design adjusted standard errors.
Meeting criteria for lifetime major depression, based on World Mental Health Composite International Diagnostic Interviews, with a depressive episode occurring at age 50 years or older.
Results are from the Collaborative Psychiatric Epidemiology Study.
Comorbid CVD and MDD
Among middle-aged and older adults, we found significant overall differences in the distribution of depression types across ethnic/race groups (p < 0.01). The proportion of middle-aged and older adults meeting MDD criteria without CVD was highest among Puerto Ricans (10.7%), and lowest among Blacks (1.6%) (Table 2). Comorbid CVD/MDD was most common among the Latino ethnicities, Cubans (8.9%), Puerto Ricans (6.5%), and Mexicans (6.62%). Black respondents (4.7%) were least likely to have met our criteria for comorbid CVD and MDD. Among middle-aged and older adults meeting MDD criteria, Black respondents were most likely to have met our criteria for a comorbid CVD/MDD (74.4%).
Table 2.
Prevalence of comorbid cardiovascular disease (i.e. broadly defined as risk factors for cardiovascular, heart attack and stroke) and major depression among ethnic/race group respondents 50 years and older in the United States
| CUBAN | PUERTO RICANS | MEXICANS | BLACKS | WHITES | TOTAL | ||
|---|---|---|---|---|---|---|---|
| All middle-aged and older adults | |||||||
| No depression | %c | 87.13 | 80.81 | 90.05 | 93.68 | 90.34 | 90.56 |
| SEd | 1.15 | 4.07 | 2.48 | 0.64 | 0.85 | 0.74 | |
| N | 236 | 111 | 172 | 1599 | 1635 | 3753 | |
| MDDa | % | 3.95 | 10.69 | 3.33 | 1.62 | 3.91 | 3.72 |
| SE | 0.89 | 3.92 | 1.37 | 0.25 | 0.40 | 0.35 | |
| N | 12 | 15 | 12 | 35 | 134 | 208 | |
| Comorbid CVD/MDDb | % | 8.93 | 8.50 | 6.62 | 4.70 | 5.75 | 5.73 |
| SE | 1.33 | 1.71 | 1.63 | 0.58 | 0.73 | 0.62 | |
| N | 28 | 14 | 17 | 87 | 174 | 320 | |
| p <0.001 | |||||||
| Middle-aged and older adults meeting MDD criteria | |||||||
| MDD alonea | % | 30.66 | 55.69 | 33.49 | 25.57 | 40.48 | 39.35 |
| SE | 7.02 | 10.84 | 8.76 | 3.69 | 3.86 | 3.30 | |
| N | 12 | 15 | 12 | 35 | 134 | 208 | |
| Comorbid CVD/MDDb | % | 69.34 | 44.31 | 66.51 | 74.43 | 59.52 | 60.65 |
| SE | 7.02 | 10.84 | 8.76 | 3.69 | 3.86 | 3.30 | |
| N | 28 | 14 | 17 | 87 | 174 | 320 | |
| p = 0.077 | |||||||
Meeting criteria for lifetime major depression, based on World Mental Health Composite International Diagnostic Interviews at age 50 years or older.
Meeting criteria for a lifetime major depressive disorder (MDD) with a depressive episode occurring at age 50 years or older, and self-reported medical diagnoses of one or more cerebrovascular disease (including diabetes, hypertension, heart disease, or stroke).
Weighted prevalence rates.
Survey design adjusted standard errors.
Results are from the Collaborative Psychiatric Epidemiology Surveys.
Multivariate results
Table 3 shows the results from multivariate logistic regression models. Compared to non-Latino Whites and controlling for age and sex, the odds of meeting criteria for comorbid CVD/MDD were significantly increased for Blacks respondents. Cubans and Mexicans also presented higher OR compared to non-Latino Whites; however, these odds did not reach statistical significance levels. The odds of comorbid CVD/MDD were twice as high for both males relative to females (OR = 2.16; 95% CI = 1.28–3.62) and adults 65 years and older compared to those in 50 to 64 years group (OR = 2.05; 95% CI = 1.29–3.24).
Table 3.
Correlates of comorbid CVD/MDDa among middle-aged and older adults (50 years and older) meeting criteria for major depression
| MODEL 1b
|
MODEL 2c
|
MODEL 3d
|
MODEL 4e
|
|||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% C I | OR | 95% C I | OR | 95% C I | OR | 95% C I | |
| Ethnicity/race | ||||||||
| Non-Latino Whites | Ref | Ref | Ref | Ref | ||||
| Cubans | 1.54 | 0.74–3.18 | 1.51 | 0.71–3.21 | 1.41 | 0.67–2.94 | 1.35 | 0.63–2.94 |
| Puerto Ricans | 0.54 | 0.21–1.37 | 0.52 | 0.21–1.33 | 0.56 | 0.23–1.34 | 0.54 | 0.22–1.30 |
| Mexicans | 1.35 | 0.57–3.21 | 1.27 | 0.54–3.03 | 1.35 | 0.56–3.25 | 1.24 | 0.52–2.96 |
| Blacks | 1.98*** | 1.18–3.31 | 1.95** | 1.13–3.35 | 2.12*** | 1.25–3.59 | 2.11*** | 1.21–3.70 |
| Sex | ||||||||
| Female | Ref | Ref | ||||||
| Male | 1.99** | 1.16–3.39 | 2.16*** | 1.28–3.62 | ||||
| Age | ||||||||
| 50–64 | Ref | Ref | ||||||
| 65+ | 1.89*** | 1.17–3.03 | 2.05*** | 1.29–3.24 | ||||
Outcome is depression type (two categories) with non-comorbid depression set as the reference. Odds ratios are of comorbid CVD/MDD relative to uncomplicated. Depression alone is defined as meeting criteria for lifetime major depression, based on World Mental Health Composite International Diagnostic Interviews, with a depressive episode occurring at age 50 years or older and no reported cerebrovascular diseases. Comorbid CVD/MDD is defined as meeting criteria for a lifetime major depressive disorder (MDD) with a depressive episode occurring at age 50 years or older, and self-reported medical diagnoses of one or more cerebrovascular disease (including diabetes, hypertension, heart disease, or stroke).
Model 1: Unadjusted.
Model 2: Adjusted for sex.
Model 3: Adjusted for age.
Model 4: Adjusted for sex and age.
p < 0.10.
p < 0.05.
p < 0.01.
Results are from logistic regression models using data from the Collaborative Psychiatric Epidemiology Surveys.
Days of functional impairment
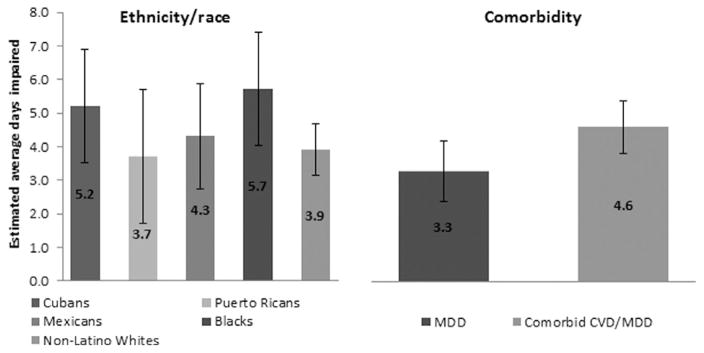
Our negative binomial regression model estimates indicated that controlling for comorbidity, sex, and age, Blacks reported significantly more days of impairment relative to non-Latino Whites (Table 4). Cuban and Mexican respondents also reported more impairment days, but the differences relative to non-Latino Whites were not statistically significant. Meeting criteria for comorbid CVD/MDD was associated with more days of impairment relative to MDD alone. Model-derived estimates of average impairment days and their CI by race/ethnic grouping and comorbidity status were calculated and graphed in Figure 1. Tests of interactions between ethnic/race grouping and comorbidity status did not evidence any statistically significant relationships suggesting similar disease burden for comorbidity among middle-aged and older adults irrespective of ethnic/racial background. Finally, age and sex were not statistically linked to average impairment days.
Table 4.
Correlates of WHODAS-II average functional impairmenta among middle-aged and older adults (50 years and older) meeting major depression criteria
| IRR b | 95% CI | |
|---|---|---|
| Ethnicity/race | ||
| Non-Latino Whites | Ref | n/a |
| Cubans | 1.33 | 0.90–1.96 |
| Puerto Ricans | 0.94 | 0.52–1.71 |
| Mexicans | 1.10 | 0.70–1.72 |
| Blacks | 1.46* | 1.01–2.12 |
| Depression type | ||
| MDDc | Ref | n/a |
| Comorbid CVD/MDDd | 1.40* | 1.05–1.86 |
| Sex | ||
| Female | Ref | n/a |
| Male | 0.94 | 0.68–1.31 |
| Age | ||
| 50–64 | Ref | n/a |
| 65+ | 0.74 | 0.51–1.07 |
Based on average number of days impaired across five functional domains based on the World Health Organization Disability Assessment Scale (WHODAS-II) including self-reported number of days out of role in: (1) overall role impairment; (2) cognition; (3) mobility; (4) self-care; and (5) social impairment. Estimates are sex and age adjusted.
Incidence rate ratio.
Meeting criteria for lifetime major depression, based on World Mental Health Composite International Diagnostic Interviews, with a depressive episode occurring at age 50 years or older and no reported cerebrovascular diseases.
Meeting criteria for a lifetime major depressive disorder (MDD) with a depressive episode occurring at age 50 years or older, and self-reported medical diagnoses of one or more cerebrovascular disease (including diabetes, hypertension, heart disease, or stroke).
p < 0.05.
Results are from a negative binomial regression model using data from the Collaborative Psychiatric Epidemiology Surveys.
Figure 1.
Estimated average days impaireda (adjusted for sex and age) by ethnic/race group and depression typeb,c among middle-aged and older adults (50 years and older) meeting major depression criteria. Results are from a negative binomial regression model using CPES data.
aImpairment is calculated as average impairment days across five functional domains based on the World Health Organization Disability Assessment Scale (WHODAS-II) including self-reported number of days out of role in: (1) overall role impairment, (2) cognition, (3) mobility, (4) self-care, and (5) social impairment.
bMeeting criteria for lifetime major based on World Mental Health Composite International Diagnostic Interviews, with a depressive episode occurring at age 50 years or older and no reported cerebrovascular diseases (including diabetes, hypertension, heart disease, or stroke).
cMeeting criteria for a lifetime major depressive disorder with a depressive episode occurring at age 50 years or older, and self-reported medical diagnoses of one or more cerebrovascular disease.
Depression treatment
Multivariate logistic regression models showed that neither comorbid CVD/MDD status nor ethnicity/race were statistically linked to depression treatment (Table 5). The lack of statistical evidence was common to all three treatment types considered. Older age was statistically associated with lower odds of both psychotherapy and any therapy use.
Table 5.
Correlates of depression treatment among middle-aged and older adults (50 years and older) meeting major depression criteria
| PHARMACOTHERAPYa
|
PSYCHOTHERAPYb
|
ANY THERAPYc
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Ethnicity/race | ||||||
| Non-Latino Whites | Ref | n/a | Ref | n/a | Ref | n/a |
| Cubans | 0.85 | 0.54–1.33 | 1.28 | 0.78–2.10 | 0.88 | 0.50–1.56 |
| Puerto Ricans | 0.64 | 0.23–1.78 | 0.94 | 0.39–2.28 | 0.98 | 0.45–2.13 |
| Mexicans | 0.38 | 0.11–1.38 | 0.79 | 0.35–1.76 | 0.47 | 0.21–1.03 |
| Blacks | 0.68 | 0.39–1.17 | 1.41 | 0.85–2.33 | 0.97 | 0.60–1.59 |
| Depression type | ||||||
| MDDd | Ref | n/a | Ref | n/a | Ref | n/a |
| Comorbid CVD/MDDe | 0.74 | 0.40–1.36 | 0.93 | 0.53–1.63 | 0.87 | 0.52–1.48 |
| Sex | ||||||
| Female | Ref | n/a | Ref | n/a | Ref | n/a |
| Male | 1.22 | 0.61–2.45 | 1.35 | 0.66–2.76 | 1.11 | 0.57–2.18 |
| Age | ||||||
| 50–64 | Ref | n/a | Ref | n/a | Ref | n/a |
| 65+ | 0.72 | 0.39–1.31 | 0.36*** | 0.20–0.64 | 0.51** | 0.28–0.92 |
Antidepressant prescription drug use based on respondent report and pill bottle inventory reviews.
Self-reported treatment by a mental health professional including by a psychiatrist, psychologist, counselor, or social worker.
Either pharmacotherapy or psychotherapy.
Meeting criteria for lifetime major depression, based on World Mental Health Composite International Diagnostic Interviews, with a depressive episode occurring at age 50 years or older and no reported cerebrovascular diseases.
Meeting criteria for a lifetime major depressive disorder (MDD) with a depressive episode occurring at age 50 years or older, and self-reported medical diagnoses of one or more cerebrovascular disease (including diabetes, hypertension, heart disease, or stroke).
p < 0.05.
p < 0.01.
Results are from logistic regressions using data from the Collaborative Psychiatric Epidemiology Surveys.
Discussion
We found that two-thirds of middle-aged and older American adults meeting criteria major depression also reported a diagnosis of comorbid CVD. The proportion of comorbid CVD/MDD was highest for Blacks (74.4%), which was followed by Cubans (69.3%) and Mexican Americans (66.5%), respectively. Older age and males were at increased risk for comorbid CVD/MDD. As was expected, comorbid CVD/MDD was associated with a higher number of days of functional impairment relative to uncomplicated MDD, and Blacks reported markedly higher disability compared to Whites. However, past-year pharmacotherapy and psychotherapy use rates were not remarkably higher for those meeting our comorbid CVD/MDD criteria. Our findings indicate that the majority of middle-aged and older patients meeting major depression criteria would also present with a comorbid CVD. While we were unable to provide explanations for the high prevalence of comorbid CVD/MDD; however, our findings suggest that it is associated with increased disease burden without higher treatment rates in the United States.
To our knowledge, our study provides the first estimates of comorbid CVD and MDD specific to middle-aged and older ethnic/racial groups in the United States. For clinicians serving ethnically and racially diverse groups of middle-aged and older adults with MDD, our findings indicate that a comorbid CVD may be thought of as the norm rather than the exception. Furthermore, for Blacks, Cubans and Mexican Americans meeting MDD criteria, the base rates approach 75%. MDD can present challenges for clinicians and patients since preventing CVD progression depends heavily on lifestyle modifications for middle-aged and older patients who may have been sedentary for much of their adult lives (Katon, 1996). Additionally, therapy choices for patient benefit and safety may be guided, but limited within the context of comorbid CVD and MDD. Regardless of temporal etiologic relationship between CVD and MDD, our findings indicate that the two are common conditions that practitioners are likely to encounter regularly among ethnically/racially diverse patients and treat today.
Our general US adult population estimate was more than double that reported by Goodwin and colleagues (2009). The differences in estimates are likely attributable to our focus on middle-aged and older adults and ethnic/racial group who would be expected to have higher rates of CVD in contrast to the general US population of adults 18 years and older (Roger et al., 2011; Flegal et al., 2012). Among middle-aged and older adults meeting CVD and MDD criteria in this study, we found that older age was associated with the increased likelihood of comorbid CVD/MDD. Second, although previous studies have consistently found that women are at increased risk for major depression (Kessler et al., 2003; Williams et al., 2007; González et al., 2010), the risk of comorbid CVD/MDD was more than double for men 50 years and older in our study. This unusual finding may be explained by the generally higher rates of CVD among this age cohort of men. Recent population trends in CVD risk factors, especially among ethnic/racial minority women, suggest that the gender differences we observed may shift in coming years (Flegal et al., 2012).
More days of role impairment were reported by middle-aged and older respondents meeting criteria for comorbid CVD/MDD than respondents with MDD alone. While not surprising, the additional disease burden we observed suggests that CVD and MDD may be interacting at more fundamental, biological levels. While we were unable delve deeper into the causes of the higher role impairment we observed in respondents with comorbid CVD/MDD, our findings were consistent with previous work that has examined the biological substrates of CVD and MDD (Krishnan and McDonald, 1995; Steffens et al., 2002). Black respondents, along with Cubans to a lesser extent, who met our comorbid CVD/MDD criteria reported the highest number of days out of role. Our results offer a plausible biological explanation for the findings of Williams and colleagues (2007) that while Blacks may have a lower prevalence of MDD, they reported increased disability MDD than other ethnic/racial groups (Williams et al., 2007). Despite the excess role impairment associated with comorbid CVD/MDD, we did not find concomitantly increased depression care rates, regardless of ethnicity/race. Examining the reasons for the low rate of depression care among respondents meeting comorbid CVD/MDD criteria was not possible in our study.
Several study limitations should be considered when evaluating our findings. First, we relied on survey data for our national estimates. In-depth clinical and medical history information from records was not available. Therefore, we must assume that survey respondents provided accurate medical history information (e.g. heart disease). Furthermore, it is possible that ethnic/racial differences in CVD self-reporting accuracy and reliability may exist and could have affected our estimates. Second, CPES data did not include homeless or institutionalized persons, which could have affected our estimates. Third, although it was possible to disaggregate Black ethnicity in CPES, the limited number of Caribbean Black MDD cases precluded reliable and stable estimates for this group. Similarly, the limited number of Asians meeting our CVD/MDD criteria limited our capacity to generate reliable estimates. Additionally, non-Latino White groups were not distinguished in the study sampling design. Consequently, reliable ethnic-specific CVD/MDD estimates of/for Blacks, Asians, and non-Latino Whites were not possible. Fourth, the test characteristics reported for WMH-CIDI indicate that it is modestly sensitive to detecting “true” psychiatric disorders (e.g. major depression) among respondents (Kessler et al., 2003). As such, “true cases” of MDD may have been missed. In addition, the test characteristics of the WMH-CIDI may have been influenced by the presence of CVD. Without appropriate psychometric information available, our results must be interpreted with precaution.
Conclusions
Our findings indicate that among middle-aged and older US adults meeting MDD criteria more than half would also report a comorbid CVD. Comorbid CVD/MDD varied markedly by ethnicity/race, herein. Functional impairment associated with comorbid CVD/MDD was higher than MDD alone; however, depression care rates did not differ remarkably. Among middle-aged and older adults meeting MDD criteria, comorbid CVD may be the rule rather than the exception.
Acknowledgments
This work was supported by the National Institutes of Health, National Institute of Mental Health (MH 84994), and the National Heart Lung Blood Institute (HC 65233). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors are grateful to Jamie M. Abelson for sharing her valuable insights about our findings, and to Dr Joseph J. Gallo for reviewing an early draft of this manuscript.
Footnotes
Conflict of interest
None.
Description of authors’ roles
Drs González and Tarraf were responsible for the study concept, design, and preparation of manuscript. Dr Tarraf was responsible for data acquisition, management, analyses, and interpretation.
References
- Alexopoulos GS. The vascular depression hypothesis: 10 years later. Biological Psychiatry. 2006;60:1304–1305. doi: 10.1016/j.biopsych.2006.09.006. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. revised. [Google Scholar]
- Cameron CA, Trivedi PK. Microeconometrics Using Stata (Revised Edition) College Station, Texas, USA: Stata Press; 2010. [Google Scholar]
- Cutler JA, Sorlie PD, Wolz L, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- George LK. Diagnosis and treatment of late life depression. In: Schneider LS, Friedhoff AJ, Reynolds CF, Lebowitz BD, editors. Depression In Late Life. Washington, DC: American Psychiatric Publishing; 1994. pp. 131–153. [Google Scholar]
- González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. Journal of Psychiatric Research. 2010;44:1043–1051. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Davidson KW, Keyes K. Mental disorders and cardiovascular disease among adults in the United States. Journal of Psychiatric Research. 2009;43:239–246. doi: 10.1016/j.jpsychires.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley HO. Multiple frame methodology and selected applications. Sankhya, Series C. 1974;36:99–118. [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W. The impact of major depression on chronic medical illness. General Hospital Psychiatry. 1996;18:215–219. doi: 10.1016/0163-8343(96)00065-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Krishnan KR, McDonald WM. Arteriosclerotic depression. Medical Hypotheses. 1995;44:111–115. doi: 10.1016/0306-9877(95)90081-0. [DOI] [PubMed] [Google Scholar]
- Pennell BE, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. International Journal of Methods in Psychiatric Research. 2004;13:241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger VL, et al. Heart disease and stroke statistics—2011 update. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffens DC, Bosworth HB, Provenzale JM, MacFall JR. Subcortical white matter lesions and functional impairment in geriatric depression. Depression and Anxiety. 2002;15:23–28. doi: 10.1002/da.1081. [DOI] [PubMed] [Google Scholar]
- Whyte EM, Mulsant BH. Post-stroke depression: epidemiology, pathophysiology, and biological treatment. Biological Psychiatry. 2002;52:253–264. doi: 10.1016/s0006-3223(02)01424-5. [DOI] [PubMed] [Google Scholar]
- Williams DR, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) World Health Organization Disability Assessment Schedule II (WHODAS II) Geneva: World Health Organization; 2001. [Google Scholar]