Positron emission tomography (PET) using ligands targeting prostate-specific membrane antigen (PSMA) has evolved as a highly effective diagnostic tool for the assessment of patients suffering from prostate cancer.1 After noninvasive confirmation of tumoral PSMA expression by PET, novel therapeutic approaches using PSMA ligands labeled with beta- or alpha-emitting radioisotopes are increasingly applied in prostate cancer patients. Notably, PSMA is also overexpressed in brain tumors and correlates with World Health Organization (WHO) grade. In contrast to prostate cancer cells, PSMA expression is particularly found in the endothelial cells associated with neovascularization, with only a small portion in tumor cells or healthy brain.2
In patients with brain tumors, there are preliminary reports visualizing PSMA using PET: A case of a glioblastoma patient suggested a pronounced uptake especially in the contrast-enhancing tumor parts surrounding necrosis, and immunohistochemical PSMA staining revealed a predominant endothelial PSMA expression.3 Additionally, a small set of brain tumor patients without immunohistochemical workup showed pronounced uptake as well.4
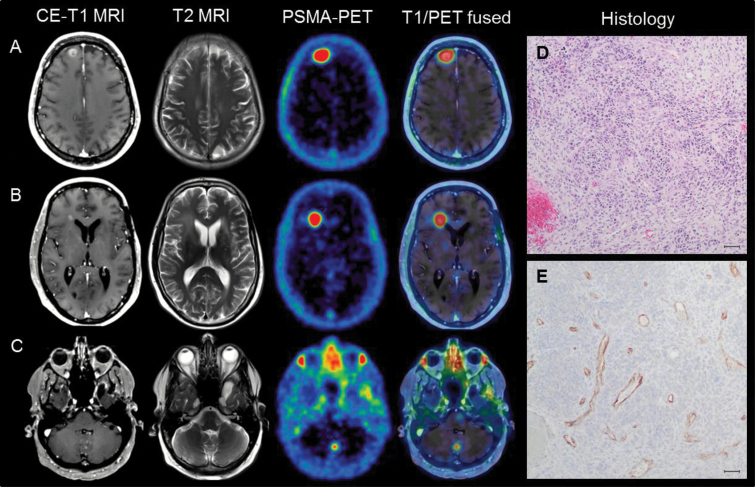
We report a case of a gliosarcoma patient (WHO grade IV; isocitrate dehydrogenase 1/2 wildtype, methylated O6-methylguanine-DNA methyltransferase promoter) with multiple brain lesions being examined with gallium-68 [68Ga]-PSMA-11 PET (196 MBq [68Ga]-PSMA-11, acquisition 60–80 min post-tracer injection) after multimodal treatment consisting of previous resection, radiochemotherapy, and bevacizumab/irinotecan chemotherapy. All lesions showed an extraordinarily high uptake (median maximal standardized uptake value of 3.43 [range, 2.22–5.27]; median maximal tumor-to-background ratio of 48.93 [range, 31.71–75.29] compared with healthy brain), as displayed in Fig. 1A–C. These parameters are even higher than those of the previously published report (ie, maximal tumor-to-background ratio of 4.07–37.2).4 Due to the high tracer binding, even lesions with a very small diameter in MRI could be detected (Fig. 1C). Histologically, gliosarcoma presented the characteristic biphasic growth pattern showing both glial and sarcomatous differentiation. Additional immunohistochemical stainings using an antibody against PSMA displayed strong PSMA expression in neovascular endothelial cells without any expression in the surrounding tumor tissue (see Fig. 1).
Fig. 1.
(A–C) Examples of the high uptake in PSMA PET; even a lesion in the cerebellum with a small diameter of 0.3 cm in MRI could be visualized by PSMA PET due to its extraordinarily high tumor-to-background ratio (TBR) contrast. (D) Gliosarcoma (WHO grade IV) showing high cellularity, pleomorphism, and microvascular proliferation. (E) Immunohistochemical PSMA staining revealed a strong PSMA expression throughout the tissue specimen, specifically in neovascular endothelial cells without any expression in solid tumor tissue (scale bar: 50 µm).
The extraordinarily high PSMA ligand binding in brain tumors may indicate potential novel diagnostic and therapeutic concepts in future. Since PSMA expression is restricted to the endothelium, PSMA PET might serve as a noninvasive imaging biomarker of neovascularization for assessment of anti-angiogenic therapies or PSMA-targeted drugs.5 This is of particular interest, since there is barely any uptake in the healthy brain leading to an outstanding contrast to the endothelial uptake. Moreover, therapeutic PSMA ligands might be of interest for glioma treatment, since therapeutic PSMA ligands provide a limited range of radiation of several millimeters; healthy brain could be spared from radiation, whereas high doses could be reached at the endothelium and the surrounding tissues.
Analogously to meningiomas, in which ligands targeting the somatostatin receptor are used for both diagnostics and radio-ligand therapy,6 PSMA ligands might offer new theranostic possibilities due to their rapidly spreading availability.
Funding
None.
Conflict of interest statement. None.
References
- 1. Haberkorn U, Kopka K, Hadaschik B. Positron emission tomography-computed tomography with prostate-specific membrane antigen ligands as a promising tool for imaging of prostate cancer. Eur Urol. 2016;69(3):397–399. [DOI] [PubMed] [Google Scholar]
- 2. Nomura N, Pastorino S, Jiang P et al. . Prostate specific membrane antigen (PSMA) expression in primary gliomas and breast cancer brain metastases. Cancer Cell Int. 2014;14(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schwenck J, Tabatabai G, Skardelly M et al. . In vivo visualization of prostate-specific membrane antigen in glioblastoma. Eur J Nucl Med Mol Imaging. 2015;42(1):170–171. [DOI] [PubMed] [Google Scholar]
- 4. Sasikumar A, Joy A, Pillai MR et al. . Diagnostic value of 68Ga PSMA-11 PET/CT imaging of brain tumors-preliminary analysis. Clin Nucl Med. 2017;42(1):e41–e48. [DOI] [PubMed] [Google Scholar]
- 5. Wernicke AG, Edgar MA, Lavi E et al. . Prostate-specific membrane antigen as a potential novel vascular target for treatment of glioblastoma multiforme. Arch Pathol Lab Med. 2011;135(11):1486–1489. [DOI] [PubMed] [Google Scholar]
- 6. Seystahl K, Stoecklein V, Schüller U et al. . Somatostatin receptor-targeted radionuclide therapy for progressive meningioma: benefit linked to 68Ga-DOTATATE/-TOC uptake. Neuro Oncol. 2016;18(11):1538–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]