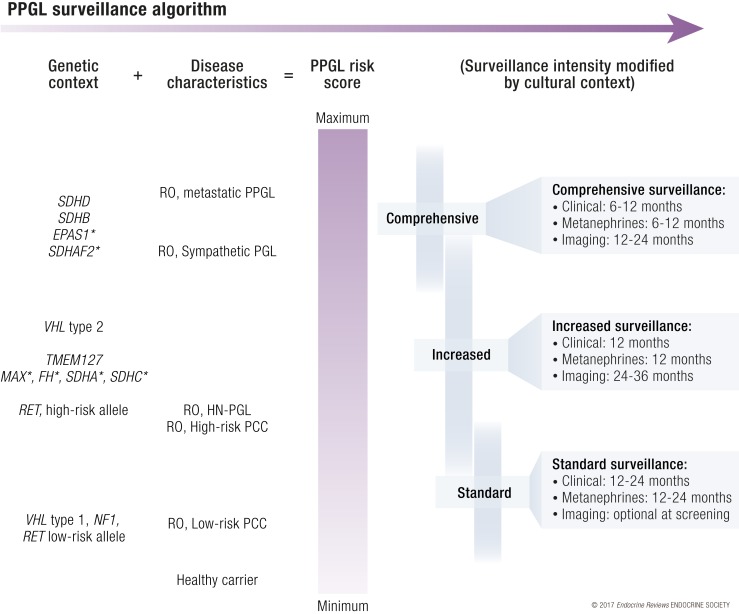
Figure 4.
Algorithm for personalized follow-up of pheochromocytoma and paraganglioma patients where risk from genetic subtype is added to disease characteristics (healthy carriers assigned zero risk) to estimate a PPGL risk score that incorporates risk of new PPGL events and frequency of metastatic disease. In addition, family history of metastatic PPGL and presentation at a young age may warrant increased surveillance of other members of that particular family, especially in patients with SDHx. Proposed definition of high-risk PCC: diameter >5 cm, 3–3.5 cm for SDHB carriers, young age at diagnosis, or moderately to poorly differentiated PPGL accordingly to GAPP classification system. Detailed description of surveillance, clinical; patient history and clinical investigation to cover symptoms of catecholamine secretion in addition to relevant information for the particular genetic syndrome. Metanephrines: selection of biochemical tests can be guided by mutation subtype as well as PPGL secretory profile of that particular patient. 3-methoxytyramine is recommended for SDHx patients only. Chromogranin A is optional. Imaging should include MRI or ultrasound of relevant anatomical sites; CT scan can be used too, based on MRI results, a radiologist’s advice, or a physician’s recommendation after detailed patient evaluation. R0, absence of residual PPGL after treatment. *, indicates high uncertainties in assumption of PPGL risk score.