Abstract
Background:
Although herbal medical products are still widely used in Kenya, many of the medicinal plants used by traditional medical practitioners (TMPs) have not been documented, despite several challenges that are now threatening the sustainability of the practice.
Objective:
To document the medicinal plants and healing methods used by TMPs in a region of Kenya with several recognized herbalists for potential research.
Materials and Methods:
Semi-structured interviews, group discussions, and direct observations were used to collect ethnopharmacological information. The participant's bio-data, clinical conditions treated, methods of treatment, medicinal plants used, methods of preparation and administration, and dosage forms were recorded.
Results:
A total of 99 medicinal plants and 12 complementary preparations employed in the treatment of 64 medical conditions were identified. The most widely used plant was Rotala tenella which was used to treat nine medicinal conditions; seven each for Aloe tweediae and Dovyalis abyssinica; and six each for Basella alba and Euclea divinorum. The plants belonged to 55 families with Fabaceae family being the most frequently used (10), followed by Apocynaceae and Solanaceae, each with six species, respectively. We identified plants used to determine the sex of an unborn baby and those used to treat several conditions including anthrax and cerebral malaria and herbs used to detoxify meat from an animal that has died from anthrax. Of special interest was R. tenella which is used to prevent muscle injury.
Conclusions:
We have documented several plants with potential therapeutic effects. Further research may be conducted to determine their efficacy.
SUMMARY
The medicinal plants used by traditional healers in a community which still practices herbal medicine in Kenya were documented. A total of 99 medicinal plants and 12 complementary preparations employed in the treatment of 64 medical conditions were identified. Further research may be carried out in order to determine their therapeutic efficacies.
Abbreviations Used: Fic: Informant consensus factor, Nur: Number of use reports in each category, Ns: Number of reported species, TMPs: Traditional medical practitioners.
Key words: Ethnopharmacology, Marakwet, medicinal plants, research, traditional medicine
INTRODUCTION
Like many other countries in Sub-Saharan Africa, traditional medical practice is still an important part of healthcare in Kenya, and herbal products are widely used especially in the rural areas.[1,2] Despite this, many of the traditional medicine products have not been documented.[3] The practice is currently facing a myriad of challenges arising mainly from lack of regulatory framework and wanton destruction of forests. In addition, the advent of modern medicine has largely relegated the practice so that young people now consider it primitive.[1] This further complicates the situation since knowledge on the practice is considered a family affair, which can only be passed to a close family member from the next generation who might not be interested. The practice has also been infiltrated by quacks who take advantage of the confusion to address the demands by the populace, especially in urban areas. In fact, most of the authentic herbalists are now of old age, mainly practicing within their localities whereby they are well known. Attempts should therefore be made to document these medicinal products before the knowledge on traditional medical practice is lost.[3] Marakwet district is one region in Kenya, whereby the practice of herbal medicine is still widespread, with several recognized practicing traditional medical practitioners (TMPs).
This study is a follow-up of the initial survey that we conducted in the whole district[4] and in the neighboring districts within the County.[5] In both studies, we found out that even in the same locality, TMPs use similar plants to treat different conditions. In addition, there were some medical conditions of interest, in which the TMPs were not willing to divulge the modes of treatment to us. Chief among these was herbs used to determine the sex of an unborn baby and those used to treat male infertility. This is mainly due to the fact that the practice is by and large a guarded family secret.[3,4] We therefore sought to conduct detailed research in two locations, whereby we had earlier identified TMPs who were willing to provide us with the information. Our lead TMP in Sangurur Mr. Josphat Kandie Simbolei is the father of JK, one of the authors who is a registered nurse who also practices as a TMP in her own right since she has been nominated to be her family's heir of the art as per tradition.[3] Her mother is also a renowned herbalist, and both of her parents are registered TMPs.
MATERIALS AND METHODS
Study area
The study was conducted in Sangurur Sublocation (0°54'0” N, 35°34'0” E), Koibarak Location, Marakwet District, Elgeyo Marakwet County, which lies at an altitude of approximately 2252 m above sea level [Figure 1].
Figure 1.
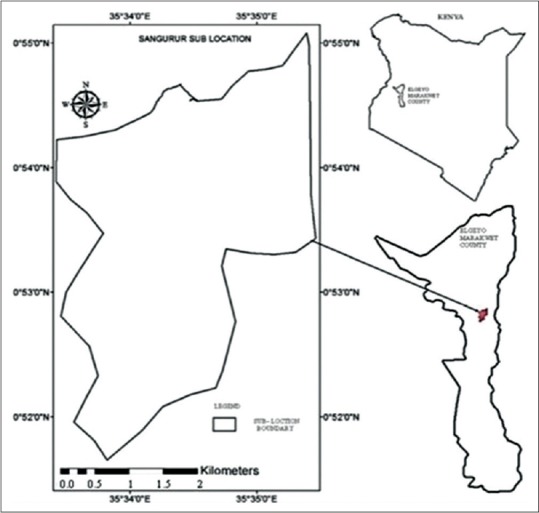
Map showing the position of Sangurur in Elgeyo Marakwet County and Kenya
Like many other parts of the County, the land mass stretches along the escarpment down to the valley with steep slopes separating the escarpment and lower region.[6] The area is largely inhabited by the Marakwet, a Kalenjin subtribe. The Kalenjins who are internationally renowned for their athletic prowess also reside in the neighboring Uasin Gishu, Nandi, Kericho, West Pokot, and Baringo Counties along the Rift Valley.[7,8,9]
Data collection
Ethnobotanical field survey was conducted between July 2014 and March 2015. The research team composed of professionals from the medical field and botany, including a clinical pharmacologist (GK), a nurse (JK), plant specialist (WK), taxonomist (BW), and a postgraduate student (BH) at the Department of Wildlife, School of Natural Resource Management. The lead TMP Mr. Simbolei always accompanied the team alone or with his spouse. This was either during the visit to his fellow colleagues or during the identification of the medicinal plants. His presence was crucial as he is a well-known and respected TMP in the location and therefore interacted easily with his colleagues, who in turn provided us the required information without hesitation. This was unlike the initial study whereby we did not have a lead TMP and had to conduct several reconnaissance visits across the districts to identify the herbalists and convince them to provide the necessary information.[4]
We used semi-structured interviews, group discussions, and direct observations to collect ethnopharmacological information.[10,11,12] The participant's bio-data, clinical conditions treated, methods of treatment, medicinal plants used, methods of preparation and administration, and dosage forms were recorded. They were also asked to explain how they made diagnosis, type of illnesses that they treated, and how they acquired the knowledge. At the end of each interview, the informants were requested to accompany the research team to the sites where they usually collected the plants and to assist in identification. Preliminary identification of the plants was then done by the team (WK and BW), and the plants and surrounding habitat were photographed. The voucher specimens were then collected using standard botanical procedures, and further identification and confirmation were done using the relevant taxonomic keys at the University of Eldoret Herbarium.[13,14] The specimen was then deposited at the same herbarium.
Data analysis
Descriptive statistics was used for statistical analysis. The data were summarized in means and frequencies, and prioritization of the medicinal plants was based on the frequency of its use. We used the number of medicinal plants as dependent variable and age, gender, and level of education as explanatory variables. Chi-square was used to test for significant difference between the responses, and multiple regression was employed to establish demographic factors that influenced TMPs.[15]
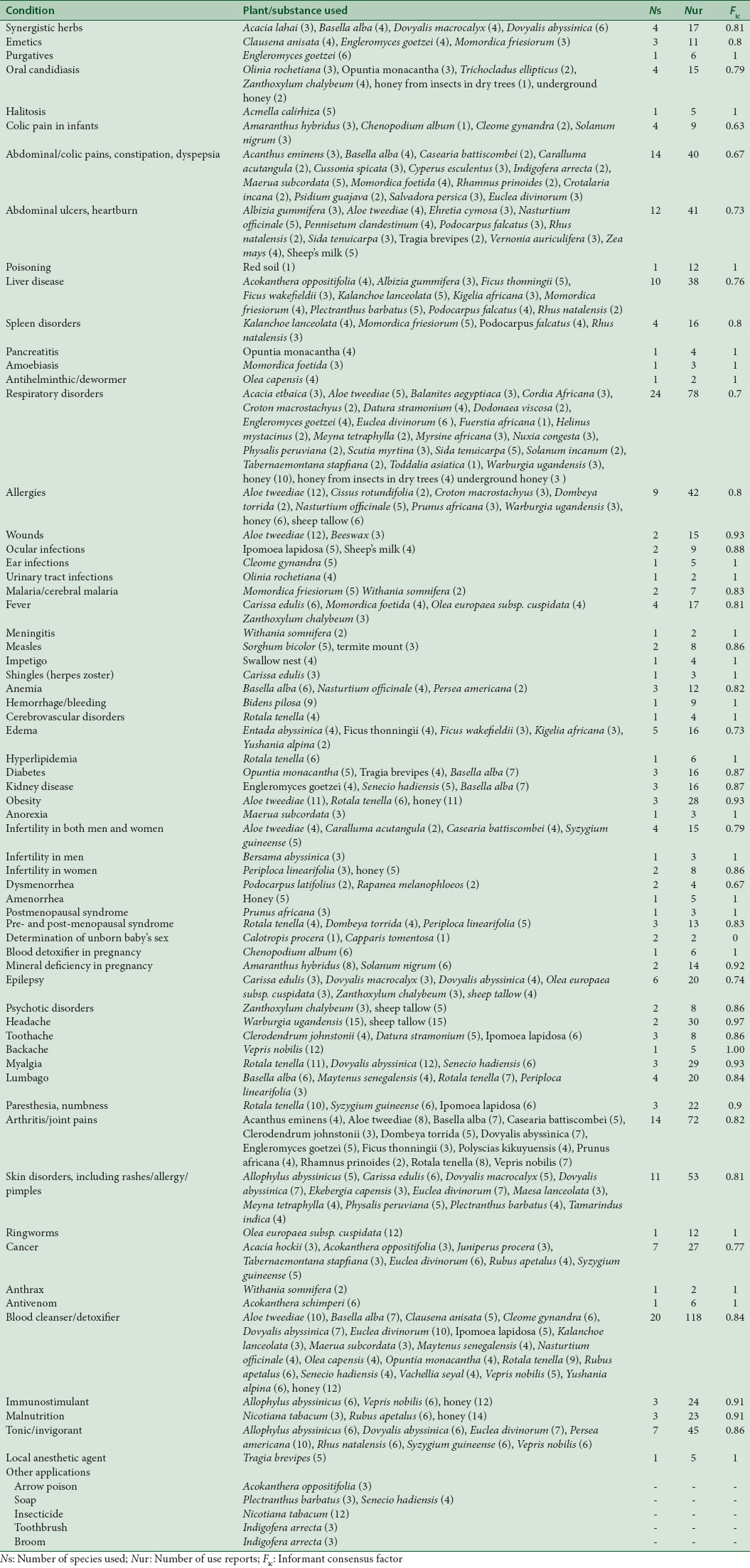
Informant consensus factor (Fic) was used to identify potentially effective plants according to the number of uses attributed each specific plant based on the information provided by the TMPs.[16,17,18] The medical conditions treated were categorized, and plants used for each condition as well as the number of use reports (citations) for each plant species were then recorded. Fic was determined by calculating the difference between the number of use reports in each category (Nur) and the number of reported species (Ns) divided by the number of use reports in each category minus one as per the following equation:

The Fic values vary between 0 and 1, whereby a high value implies that few plant species are used by a high proportion of TMPs to treat a particular ailment, whereas a low Fic suggests that the TMPs are not in agreement of the plant to be used for a specific condition. We included the identified extemporaneous preparations among the plant species as they were used concurrently.
RESULTS
Sociodemographic and practice details of the respondents
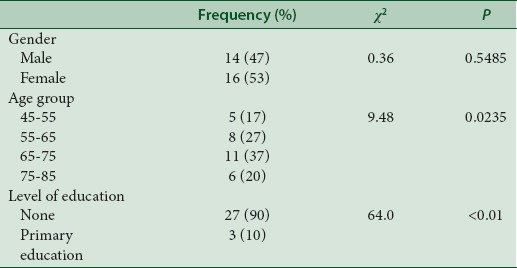
We interviewed 30 TMPs comprising 16 (53%) women and 14 (47%) men aged between 45 and 85 years. Most of them (90%) had no formal education or those who had gone to school had primary level education. The majority of the practitioners were over 55 years [Table 1]. There was a significant association between traditional medicine practice with gender (R2 = 2.32666, β = 32.099, P < 0.05) and age group (R2 = 29.2734, β = 13.86, P < 0.05). They all had acquired the knowledge from their parents or grandparents. Most of them conducted their practice from either their residence (23) or in nearby markets (7). Three of them regularly visited major centers within the county at least once in 3 months to sell their herbs to clients or fellow practitioners from other districts.
Table 1.
Sociodemographic characteristics of the respondents
They tended to specialize in the treatment of specific medical conditions, including infertility, infectious diseases, respiratory disorders, pediatric diseases, gynecologic disorders, arthritis, cancer, and psychotic disorders [Tables 2 and 3]. They were also more knowledgeable of the presenting symptoms and diagnosis of the conditions which they specialized in as compared to the TMPs we had met in our earlier studies.[3,4,5] In most cases, they used similar plants to treat the same conditions, hence the high Fic values [Table 3]. However, we also found out that they, in some instances, used similar plants to treat different conditions, and some even knew what ailments their counterparts treated using the same plant that they used for an unrelated condition. There were also those who highly specialized in their treatments, whereby the plants that they used were very secretive, an example being the herbs used for determination of an unborn baby's sex. The TMP who volunteered to reveal the plants provided with only two plants, thus giving an Fic value of 0.
Table 2.
Medicinal plant uses
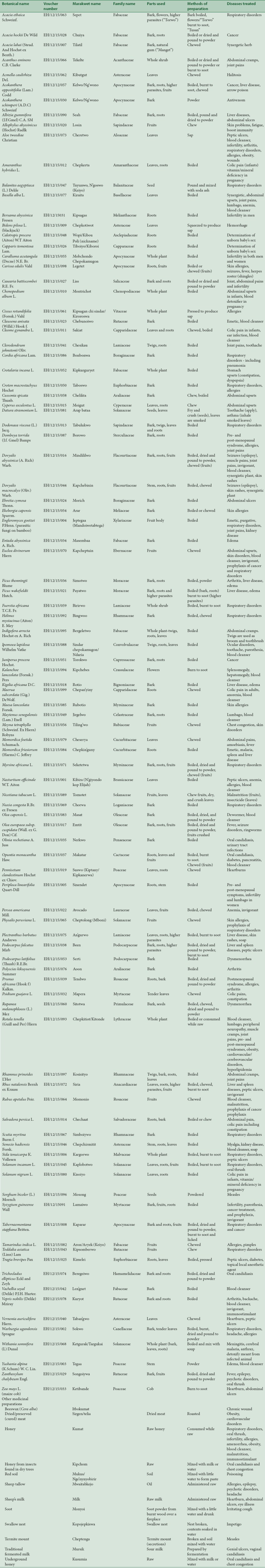
Table 3.
Fic values of the medicinal plants and complementary preparations used in treatment
Diversity of medicinal plants and uses
A total of 99 medicinal plants and 12 extemporaneous preparations were identified which were used in the treatment of 64 medical conditions [Tables 2 and 3]. The most widely used plant was Rotala tenella which was used to treat nine medicinal conditions; seven each for Aloe tweediae and Dovyalis abyssinica; and six each for Basella alba and Euclea divinorum. The most widely used medicinal preparations were honey (9) and oil from sheep tallow (4). The plants belonged to a total of 55 families with plants from Fabaceae family being the most frequently used (10), followed by Apocynaceae and Solanaceae each with six species, respectively.
Modes of preparation and administration
The parts used included bark, roots, leaves, sap, twigs, and stem. They also included higher parasites which the TMPs referred to as “Torwo.” These parasites usually grow on the twigs of trees, an example being those from Acacia etbaica, Acokanthera oppositifolia, and Ficus wakefieldii. Other preparations include fruit bodies, referred to as “Mondoiwo” or “Lobchon” in the lowland (valley) region, an example being those of Engleromyces goetzei, a parasitic fungus that grows on bamboo. The preparations used were by and large similar to those that we encountered in our earlier study within the county.[4,5] These included decoctions and concoctions mainly from boiled bark, roots, twigs, or even leaves in some instances. They could also be dried and pound to powder before administration and sometimes mixed with soup, especially for bitter plants. Other preparations include soot mainly from burnt twigs and leaves or flowers (“Tusan”), which is normally licked and natural gum (“Manget”) that is chewed. Underground honey (“Kusumia”), or honey from insects living in dry trees other than bees (“Kipchom”), as well as dried/preserved meat (“Sirgen”), was also used. Oil obtained from sheep's tallow (“Mwaitabkejo”) was also widely used. Combinations of several herbs were also used in many instances, and some plants were also used to provide additive or synergistic effects. Several plants were also used to cleanse or detoxify the blood. However, in this study, the TMPs had herbs used for prophylaxis of diseases including A. oppositifolia, E. divinorum, and Syzygium guineense used for prophylaxis of cancer and E. divinorum and Physalis peruviana for respiratory diseases.
Traditional fermented milk (“Mursik”)
Sour milk is part and parcel of Kalenjin culture and is usually drunk after every meal. Some have even hypothesized that their athletic prowess is associated with the use of “Mursik.”[19] In this study, we found out that the milk is used to treat genital ulcers and vaginal candidiasis. Its preparation involves the use of a gourd (“Sotet”), bow-shaped stick/s (“Sosiot”/“Sosik”) usually from palm trees, and charcoal from selected trees and shrubs (“Suteiywo”), the most common being Senna didymobotrya (Senetwo), Juniperus procera (Torokwo), Plectranthus barbatus (An'gurwet), Olea europaea (Emtit), and wattle trees. The sticks are used to grind embers of the charcoal by pressing against the walls of a gourd in a methodical, circular in and out movement of the hand until the inside of the gourd is evenly covered with fine dust. Boiled milk is then poured into the gourd and allowed to ferment in cool dry conditions. If a new gourd is used, then it has to be first “sweetened” to remove the bitter taste. This is done by the use of fresh bark from either Ozoroa insignis (Mutung'wo), Pappea capensis (Kibiryokwo), or Ficus thonningii (Simotwo). The bark is placed inside the gourd which is then filled with water and left to cure for 3 days.[20]
Treatment practices and plant uses
Synergistic herbs
The bark and natural gum of Acacia lahai are both chewed. Other preparations include boiled leaves of B. alba and stem or roots of Dovyalis macrocalyx mixed with those of D. abyssinica. The fruits of both plants are chewed.
Emetics
A decoction made from the boiled bark of Clausena anisata is used to induce vomiting. Boiled fruit bodies of E. goetzei (parasitic fungi growing on bamboo) and roots of Momordica friesiorum are also used.
Purgative
A decoction made from the boiled fruit bodies of E. goetzei is administered to evacuate the bowels.
Oral candidiasis
Several plants are used in the treatment of oral thrush. Fleshy leaves of Opuntia monacantha are burnt to soot (“Tusan”) and licked. The fruits Solanum incanum are also burnt and the soot applied on the lesions. Alternatively, the bark and roots of Trichocladus ellipticus or bark and fruits of Zanthoxylum chalybeum are boiled or dried and pound to powder before administration. A decoction made from the boiled bark of Olinia rochetiana is also used. Underground honey (“Kusumia”) or honey from insects living in dry trees (“Kipchom”) is also used. It is mixed with water and drunk and also smeared on the lesions.
Halitosis
The leaves of Acmella calirhiza are chewed to eliminate bad breath.
Colic pain/abdominal upsets in infants
A decoction made from the whole of Chenopodium album plant is used. Alternatively, the boiled leaves and roots of Amaranthus hybridus or Solanum nigrum may be used. The roots of Cleome gynandra are also chewed and administered. For older children, a decoction made from the boiled roots of the same plant is used.
Abdominal pains in adults
A concoction made from boiling the whole of Acanthus eminens, Caralluma acutangula, Crotalaria incana, Indigofera arrecta, or Rhamnus prinoides plants is used to treat abdominal pain. C. incana is used especially when the pain is accompanied by constipation. Boiled bark of Cussonia spicata, bark and roots of Casearia battiscombei and Salvadora persica, or leaves of B. alba may also be used. An alternative treatment involves chewing of the leaves of Momordica foetida or Psidium guajava, leaves and roots of Cyperus esculentus, roots of Maerua subcordata, bark of C. spicata, or the bark and roots of S. persica. The fruits of E. divinorum are chewed to prevent abdominal pains.
Peptic ulcers
Treatment involves administration of a concoction made from boiled bark of Ehretia cymosa, bark and roots of Albizia gummifera or Podocarpus falcatus, roots and leaves of either Rhus natalensis or Tragia brevipes, or the leaves of Nasturtium officinale. The sap obtained from crushing the leaves of A. tweediae may also be administered. Treatment also involves licking burnt soot made from burning the leaves or higher parasites from P. falcatus and R. natalensis or the whole of Sida tenuicarpa plant. The leaves of Vernonia auriculifera may also be chewed. Treatment of heartburn involves chewing the leaves and roots of Pennisetum clandestinum, licking soot obtained from burning a maize cob (Zea mays). They may also be relieved by drinking cold sheep's milk.
Poisoning
Red soil (“Mukus/Nge'nynyobirir”) is used in the management of poisoning. The soil is mixed with a little water to form a paste and administered to neutralize the effect of an orally administered poison.
Liver disease
There were six recorded plants used in the management of liver disorders. The bark and roots of A. oppositifolia, A. gummifera, F. thonningii, F. wakefieldii, P. barbatus, and P. falcatus are either boiled or dried and pound to powder before administration. The bark of Kigelia africana and roots of both M. friesiorum and R. natalensis are also boiled. Higher parasites from A. oppositifolia, F. wakefieldii, P. barbatus, and R. natalensis are burnt to soot and licked. The fruits of R. natalensis may also be used. For treatment of hepatomegaly (enlarged liver), the flowers of Kalanchoe lanceolata are burnt and licked.
Spleen disorders
The bark and roots of P. falcatus and roots of M. friesiorum are boiled and the resultant concoction administered. Higher parasites from P. falcatus and those from R. natalensis are burnt to soot and licked. Soot from burnt K. lanceolata flowers is used to treat an enlarged spleen (splenomegaly).
Pancreatitis
A concoction made from boiled leaves and roots of O. monacantha is used. Soot from the burnt leaves is also licked.
Amoebiasis
It is treated by chewing the leaves of M. foetida.
Helminthiasis
The bark of Olea capensis is used as an antihelminthic/dewormer. It is either boiled or dried and pound to powder.
Respiratory disorders
Formulations prepared from several plants are used to manage respiratory disorders, including sore throat, cough, influenza, chest pain, and running nose. They include a concoction made by boiling the whole of Dodonaea viscosa, Fuerstia africana, and S. tenuicarpa shrubs; leaves and roots of S. incanum; bark and roots of Myrsine africana and Tabernaemontana stapfiana; bark of A. etbaica, Croton macrostachyus, Helinus mystacinus, Nuxia congesta, Scutia myrtina, and Warburgia ugandensis; and fruit bodies of E. goetzei. Treatment also involves administration of sap obtained from crushing the leaves of A. tweediae and sniffing dried and burnt leaves of W. ugandensis. The powder obtained from drying and pounding the bark and roots of the same plant including those of M. africana and T. stapfiana may also be administered. Balanites aegyptiaca seed may also be pound and mixed with soda ash before administration. Other forms include licking soot made from burnt leaves of F. africana, S. tenuicarpa, S. incanum and fruits of T. stapfiana. It also involves chewing the fruits of M. africana and Toddalia asiatica; flower and higher parasites of A. etbaica; and the bark of H. mystacinus. Treatment also includes chewing of raw honey. Underground honey or honey obtained from insects living in dry trees other than bees may also be administered. It is mixed with milk or water and drunk. Soot obtained from powder from burnt wood over a fireplace (“Monyoi”) is used to treat irritating coughs. It is also mixed with a little water and drunk. A decoction prepared by boiling the bark of Cordia africana is included especially if pneumonia is involved. The fruits of E. divinorum and P. peruviana are chewed for prophylaxis of respiratory disorders.
Chest congestion
Management involves the smoking of rolled dry leaves of Datura stramonium. An alternative treatment involves chewing of Meyna tetraphylla fruits. Underground honey or honey from insects living in dry trees is also used. It is mixed with milk or water and drunk.
Allergies
Several herbal preparations are used in the management of allergies. They include a concoction made from boiled bark and roots of Dombeya torrida and Prunus africana; bark and leaves of W. ugandensis; bark of C. macrostachyus; and leaves of N. officinale. The bark and roots of D. torrida and P. africana as well as bark of W. ugandensis may also be dried, pound, and administered. In addition, the powder or burnt tender leaves of this plant are sniffed. Other treatment methods include administration of sap obtained from crushing the leaves of A. tweediae and use of the sap from Cissus rotundifolia. The whole of this plant is pressed and the sap produced rubbed on affected areas, for example, around the eyes to treat itchy eyes or on burning feet. It may also be mixed with water and used to wash the whole body. Raw honey and oil from sheep tallow are also administered to the patient, especially in the treatment of severe allergy.
Wounds
The sap obtained from the crushed leaves of A. tweediae is administered. The sap is also applied on fresh wounds to prevent scarring when healed. Beeswax (Cera alba) is used to dress the wound, especially chronic wounds.
Ocular disorders
A concoction made from the boiled twigs, roots, and leaves of Ipomoea lapidosa is administered. Raw sheep's milk is also applied on the affected eye. Human breast milk may also be used.
Ear infections
The leaves of C. gynandra are pressed and sap applied on the affected ear.
Urinary tract infections
A decoction made from the boiled bark of O. rochetiana is administered. Traditional fermented milk (“Mursik”) is drunk to hasten recovery in patients with vaginal candidiasis and genital ulcers.
Malaria
Treatment involves administration of a decoction made from the boiled roots of M. friesiorum. For cerebral malaria, the bark of Withania somnifera is boiled and decoction mixed with soup before administration.
Fever
A concoction made from the boiled bark of O. europaea subsp. cuspidata and that of Z. chalybeum is used. They may also be dried and pound to powder before administration. Alternative treatment involves chewing of raw fruits of Carissa edulis and leaves of M. foetida. A decoction made from the boiled roots of C. edulis may also be used.
Meningitis
A decoction made from the boiled bark of W. somnifera mixed with soup is used in the treatment.
Measles
The seeds of Sorghum bicolor are pound to powder and applied directly on rashes on the skin. An alternative treatment involves application of soil obtained a termite mount (“Cheptenga”) mixed with water on the rashes. The soil contains secretions from the termites.
Impetigo
Contents from a swallow nest (“Kopojepkiswa”) are applied on the affected areas. The nest is broken and contents are soaked in water.
Shingles (Herpes zoster)
It is treated by administration of a decoction made from boiled roots of C. edulis and chewing the fruits.
Anemia
It is treated by administration of a concoction made from boiled leaves of either B. alba, N. officinale, or Persea americana. Treatment also involves chewing the fruits of P. americana.
Hemorrhage/bleeding
The leaves of Bidens pilosa are squeezed and sap applied on a fresh cut or wound to stop bleeding.
Cardiovascular/cerebrovascular disorders
The whole of R. tenella plant is either boiled or consumed while raw/dried/preserved meat (“Sirgen”) is also consumed.
Edema
It is treated by administration of a concoction made from the boiled bark and roots of either F. thonningii or F. wakefieldii; bark of Entada abyssinica or K. africana; or stem of Yushania alpina. Powder obtained by drying and pounding to powder the bark and roots of F. thonningii or F. wakefieldii may also be used.
Hyperlipidemia
The whole of R. tenella plant is either boiled or consumed while raw.
Diabetes
The leaves and roots of T. brevipes or O. monacantha are boiled and administered. The leaves of this plant may also be burnt to soot and licked.
Kidney disease
A concoction made from the boiled fruit bodies of E. goetzei or stem, roots, and leaves of Senecio hadiensis is used.
Recuperating patients
A decoction made from boiled leaves of B. alba is combined with the herbs for treatment of diabetes or renal disease and administered to recuperating patients to speed up recovery.
Obesity
The whole of R. tenella plant is either boiled or consumed when raw. An alternative treatment involves consuming raw honey or administering sap obtained from crushing the leaves of A. tweediae. Dried/preserved meat is also consumed.
Anorexia
It is treated by chewing the roots of M. subcordata.
Infertility
A concoction made from boiling the whole of C. acutangula plant; bark, fruits, and roots of S. guineense; or bark and roots C. battiscombei is used in the treatment of infertility in both men and women. Other preparations include administration of dried and pound roots of C. battiscombei or sap obtained from crushing the leaves of A. tweediae.
For treatment of infertility in men, boiled roots of Bersama abyssinica are used, while a decoction made from the boiled roots and stem of Periploca linearifolia accompanied by consuming raw honey is used for the treatment of infertility in women.
Dysmenorrhea
Treatment is by administration of a decoction made from the boiled bark of either Podocarpus latifolius or Rapanea melanophloeos. The seeds of this plant may also be chewed or dried and pound to powder before administration.
Amenorrhea
It is treated by consuming raw honey.
Postmenopausal syndrome
The bark and roots of P. africana are boiled or dried and pound to powder before administration.
Both pre- and post-menopausal syndrome
The whole of R. tenella plant is either boiled or consumed as raw. Other preparations include the use of a concoction made from boiled stem and roots of P. linearifolia or bark and roots of D. torrida. Powder made by pounding the bark and roots of this plant may also be used.
Determination of the unborn baby's sex
A decoction made from the boiled roots of either Calotropis procera or/and Capparis tomentosa is used. It is administered before conception.
Blood detoxifier in pregnancy
The whole of C. album plant is cooked and consumed as vegetable.
Vitamin/mineral deficiency in pregnancy
A decoction made from the boiled leaves and roots of either A. hybridus or S. nigrum is used.
Epilepsy
Seizures including epilepsy are treated by the administration of a concoction made from boiled stem and roots of D. macrocalyx mixed with those of D. abyssinica or roots of C. edulis. The fruits of these plants are also chewed. An alternative treatment involves use of a concoction from the boiled bark and roots of O. europaea subsp. cuspidata or bark and fruits of Z. chalybeum. Powder obtained by drying and pounding of the same parts may also be used. Oil made from sheep tallow is also used.
Psychotic disorders
The bark and fruits of Z. chalybeum are either boiled or dried and pound to powder before administration. Oil made from sheep tallow is also administered.
Headache
A concoction made from the boiled bark and tender leaves of W. ugandensis is used. They may also be burnt and sniffed or dried and pound to powder before sniffing. Oil from sheep tallow is also used.
Toothache
A concoction made from boiled twigs, roots, and leaves of I. lapidosa or twigs and roots of Clerodendrum johnstonii is used. The seeds of D. stramonium may also be fried and pound before administration.
Backache
It is treated by administration of a concoction made from the boiled bark and roots of Vepris nobilis.
Myalgia
Treatment of muscle pains including cramps involves use of boiled stem, roots, and leaves of S. hadiensis or the whole of R. tenella plant. The plant may also be consumed when raw. We were informed by the TMPs that plant is very popular with athletes as it prevents muscle injury. An alternative treatment involves the use of the boiled bark and roots of D. abyssinica which may also be dried and pound and mixed with soup before administration. The fruits of the same plant are chewed.
Lumbago
Pain of the muscles and joints of lower back is treated by the use of a concoction made from either boiled leaves of B. alba, bark and roots of Maytenus senegalensis, or the whole of R. tenella plant, which may also be consumed while raw. Lumbago in women is treated by administration of boiled stem and roots of P. linearifolia.
Paresthesia
Peripheral neuropathy is treated by administration of a concoction made from boiled fruits, bark, roots of S. guineense or the whole of R. tenella which may also be consumed when raw. Numbness, especially of the feet, is treated by administration of a concoction made from boiled twigs, roots, and leaves of I. lapidosa.
Local anesthetic agent
The leaves of T. brevipes are used to provide local analgesic effect. They are pressed and rubbed on the affected sites.
Bone and connective tissue disorders
Arthritis and joint pains are treated by the use of several plants in different preparations. The boiled or dried and powder from the bark and roots of C. battiscombei, D. torrida, F. thonningii, P. africana, or D. abyssinica are used. The fruits of this plant are also chewed. An alternative preparation constitutes the boiled twigs, bark, roots, and leaves of R. prinoides, twigs and roots of C. johnstonii, bark and roots of V. nobilis, bark of Polyscias kikuyuensis, leaves of B. alba, or the whole of R. tenella plants. Boiled fruit bodies of E. goetzei are also used. Sap obtained from crushing the leaves of A. tweediae may also be administered. The whole of A. eminens plant is either boiled or dried and pound to powder. It may also be burnt to soot and licked.
Skin disorders
Skin conditions including rashes, allergy, and pimples are treated by a variety of plants. It includes chewing the fruits of the following plants: Allophylus abyssinicus, C. edulis, D. macrocalyx, D. abyssinica, E. divinorum, M. tetraphylla, P. peruviana, and Tamarindus indica. The bark of Ekebergia capensis and Maesa lanceolata is also chewed. In addition, a concoction made from the boiled stem and roots of D. macrocalyx mixed with those of D. abyssinica, roots of C. edulis and P. barbatus as well as bark of E. capensis is used. Ringworms are treated by application of oil obtained from crushing the fruits of O. europaea subsp. cuspidata on the affected areas.
Cancer
The treatment is by administration of a concoction made from boiled bark and roots of Acacia hockii, A. oppositifolia, J. procera, T. stapfiana, and S. guineense. The fruits of this plant may also be included. Other preparations include powder from dried and pound bark and roots of A. hockii, A. oppositifolia, and T. stapfiana. The higher parasites from A. oppositifolia are also burnt to powder and licked. In case there are any wounds arising from the disease, powder obtained from dried and pound bark and roots of A. oppositifolia is applied. For prophylaxis, roots of this plant and fruits of either E. divinorum or Rubus apetalus are chewed. A decoction made from the boiled roots of S. guineense may also be used.
Anthrax
A decoction made from the bark of W. somnifera mixed with soup is used to treat a patient with the viral disease. To detoxify meat from an animal which has died from anthrax, the meat is boiled with a decoction obtained from the bark of this plant after which it is considered edible. The sap from the leaves is applied to the lacerations on the skin of an animal with anthrax.
Antivenom
The powder obtained from dried and pound bark of Acokanthera schimperi is used in the management of snake bites. Incisions are made on the bitten area and powder applied to arrest movement of the venom.
Blood cleanser/detoxifier
Several plants are used as blood cleansers or detoxifiers to remove toxins from the body. These include a concoction made from the whole of R. tenella plant, bark and roots of D. abyssinica, Macaranga kilimandscharica, M. senegalensis, or V. nobilis as well as the bark of C. anisata, O. capensis, and Vachellia seyal. Other preparations include boiled twigs, roots, and leaves of I. lapidosa; stem, roots, and leaves of S. hadiensis; leaves of both B. alba and N. officinale; including the roots of C. gynandra. Also used is the powder made from the dried and pound stem of Y. alpina, bark of O. capensis, and bark and roots of D. abyssinica which is normally mixed with soup as it is bitter. In addition, the fruits of this plant are chewed. The fruits of E. divinorum and O. monacantha are also chewed as part of treatment. Also chewed are leaves of C. gynandra and roots of M. subcordata. Likewise, the whole of R. tenella plant and honey are consumed while raw, whereas the flowers of K. lanceolata are burnt and the soot licked. The sap obtained by squeezing the leaves of A. tweediae and fruits of R. apetalus is also administered for the same purpose.
Immunostimulants and related preparations
A decoction made from the boiled bark and roots of V. nobilis is used to stimulate immunity. In addition, the fruits of A. abyssinicus are chewed and raw honey was consumed.
Malnutrition
The sap made from crushing the fruits of R. apetalus is administered to add minerals and nutrients to the body, whereas those of Nicotiana tabacum are chewed for the same purpose. Honey is also used to treat malnutrition, to add minerals and vitamins to the body, as well as to strengthen bones and teeth.
Tonic/invigorant
Preparations made from several plants are used to restore vigor and vitality and reduce fatigue. They include a concoction made from boiled bark and roots of S. guineense, D. abyssinica, and V. nobilis; leaves, fruits, seeds of P. americana; or roots of R. natalensis. Leaves and higher parasites from this plant are also burnt to soot and licked. Other treatment methods include chewing the fruits of A. abyssinicus, D. abyssinica, E. divinorum, R. natalensis, and S. guineense or administration of the powder from the dried and pound bark and roots of D. abyssinica which is usually mixed with soup.
Other related preparations
Arrow poison
A decoction made from the roots of A. oppositifolia is used. The roots are boiled and allowed to settle and the sediment is then applied on the arrow heads.
Soap
The leaves of either S. hadiensis or P. barbatus are crushed and mixed with water, and the resultant froth is used as soap to wash babies.
Insecticide
The crushed leaves of N. tabacum are used as an insecticide. They are crushed and soaked in water and left for about 2 weeks. The liquid is then sprayed on vegetables. Alternatively, the leaves can be dried, pound, and mixed with water.
Toothbrush
The twigs of I. arrecta are used as toothbrushes. The young branches and leaves of this tree are also used as a broom.
DISCUSSION
Most of the plants used were those that we had identified in our earlier studies in the Marakwet, Keiyo, and Nandi studies.[4,5,21] However, the indications were different, and the TMPs tended to be very specific in their treatments. They were more knowledgeable of several medical conditions and offered specialized treatment of such conditions as infectious diseases and gynecological, pediatric, and abdominal disorders. For instance, we were for the first time informed of herbs used to determine the sex of unborn babies and those used in the treatment of male infertility. They could also treat anthrax, cerebral malaria, hyperlipidemia, obesity, anorexia, pre- and post-menopausal syndrome, dysmenorrhea, arthritis, and psychotic disorders. In addition, they had herbs used in the prophylaxis of some diseases such as cancer (A. oppositifolia, E. divinorum, R. apetalus, S. guineense) and respiratory disorders (E. divinorum, P. peruviana). To determine the sex of an unborn baby, a concoction made from the boiled roots of C. procera and C. tomentosa is used before conception. C. procera has been reported to inhibit implantation and therefore interfere with the estrous cycle in female rats,[22] while C. tomentosa has been used to treat infertility and impotence by some South African communities.[23] Most of the clients who required this service were families who had females in succession and wished to have a son. The Kalenjin, like most other Kenyan communities, still consider a son to be the heir of the family property and clan virtues as a daughter is considered as one who is to be married off to another clan, community, or even culture to start off a different family belonging to wherever she is married after payment of bridewealth.[24] Many of those without a son would therefore try all means including fathering several children in the hope that they would get a son or even marry another wife or wives. Indeed, we were informed by one TMP who specializes in that line that she receives clients from all over the country, including foreigners, and that they were all successful in their quest since they always came back to reward her handsomely.
It was interesting to note that some of the plants used in therapy had been deemed to be poisonous in our earlier studies. An example is A. oppositifolia which is employed in the treatment of cancer and liver disease. On searching the literature, we found out that the plant has indeed been demonstrated to possess antioxidant and moderate anticancer activity.[25,26] We also found out that W. somnifera, used in the management of cerebral malaria, meningitis, and anthrax, has been shown to possess antibacterial,[27] antifungal,[28] antimalarial,[29] and antiviral activities.[30,31] In addition, the TMPs informed us that they were able to detoxify meat from an animal that died from anthrax by boiling in a decoction obtained from the bark of this plant and then consumed.
There were several other recorded plants whose in vitro pharmacological effects have been investigated and found to correlate with the information provided by the TMPs. These include antibacterial and antifungal effects of O. rochetiana used in the management of urinary tract infections and oral candidiasis,[32] hypoglycemic/hepatoprotective effects of O. monacantha used in the treatment of diabetes and pancreatitis,[33,34] and spasmolytic effects of A. hybridus used to relieve colic pains and abdominal upsets.[35] Others include gastroprotective effects of N. officinale,[36] antimicrobial effects of Aloe, Cleome, and Ipomoea, spp.,[36,37,38] and hepatoprotective effects of Ficus, Kalanchoe, Momordica, and Rhus spp.[39,40,41,42]
Of specific interest is R. tenella which is used in the treatment of several conditions including lumbago, peripheral neuropathy, muscle cramps, joint pains, pre-and post-menopausal syndromes, obesity, cardiovascular/cerebrovascular disorders, and hyperlipidemia. It is also used as a blood cleanser. We were informed by the TMPs that plant is very popular among athletes as they believe that it contains nutrients which prevent muscle injury. In fact, we met three top athletes from Iten collecting the preparation from the residence of one of the TMPs. Iten, the County headquarters, which has been dubbed “The Home of Champions,” is literally the headquarters of athletics. Most the world's elite athletes including the current world Marathon champion train there.[43] There was scant information from the literature about the pharmacological or mineral contents of this plant and research on this plant may be worth consideration.
CONCLUSIONS
Local knowledge of medicinal plants used in the treatment of several medical conditions still exists in Sangurur location and forms an important role in primary healthcare. We identified plants used in the management of several conditions including anthrax, cerebral malaria, and herbs used to detoxify meat from an animal that has died from anthrax. Of specific interest are those plants used to determine the sex of an unborn baby and R. tenella which is used to prevent muscle injury among many other therapeutic indications. Further research should be conducted to determine the efficacy and pharmacological profiles of the listed medicinal plants. Attempts should also be made to document medicinal plants used by other Kenyan communities who still practice herbal medicine to create a database for future research and potential development of new drugs before the knowledge is lost.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Our sincere thanks go to Mr. Josphat Kandie Simbolei and his spouse Elizabeth Jemosop for the invaluable assistance in the identification of the recognized TMPs and medicinal plants. We also thank all the herbalists who participated in the study.
REFERENCES
- 1.Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):115–23. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. WHO Traditional Medicine Strategy: 2014-2023. 2013. [Lasd accessed on 2016 Mar 29]. Available from: http://www.apps.who.int/iris/bitstream/10665/92455/1/9789241506090_eng.pdf .
- 3.Kigen GK, Ronoh HK, Kipkore WK, JK R. Current trends of traditional herbal medicine practice in Kenya: A review. Afr J Pharmacol Ther. 2013;2:32–7. [Google Scholar]
- 4.Kipkore W, Wanjohi B, Rono H, Kigen G. A study of the medicinal plants used by the Marakwet Community in Kenya. J Ethnobiol Ethnomed. 2014;10:24. doi: 10.1186/1746-4269-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kigen G, Some F, Kibosia J, Rono H, Kiprop E, Wanjohi B, et al. Ethnomedicinal plants traditionally used by the Keiyo Community in Elgeyo Marakwet County, Kenya. J Biodivers Bioprospect Dev. 2014;1:132–43. [Google Scholar]
- 6.Sangurur Sub-location. [Last accessed on 2016 Mar 11]. Available from: http://wwwgetamapnet/maps/kenya/rift_valley/_sangurursublocation/
- 7.Wikipedia. Kalenjin People. [Last accessed on 2016 Apr 06]. Available from: https://www.en.wikipedia.org/wiki/Kalenjin_people .
- 8.Onywera VO, Scott RA, Boit MK, Pitsiladis YP. Demographic characteristics of elite Kenyan endurance runners. J Sports Sci. 2006;24:415–22. doi: 10.1080/02640410500189033. [DOI] [PubMed] [Google Scholar]
- 9.Manners J. Kenya's running tribe. Sports Hist. 1997;17:14–27. [Google Scholar]
- 10.Stepp JR. Advances in ethnobiological field methods. Field Methods. 2005;17:211–8. [Google Scholar]
- 11.Alexiades MN, Sheldon JW. Advances in economic botany. Selected Guidelines for Ethnobotanical Research: A Field Manual. Vol. 10. Bronx, NY, USA: New York Botanical Garden; 1996. pp. 53–94. [Google Scholar]
- 12.Martin GJ. Ethnobotany: A Methods Manual. edn.: Earthscan; 2004. [Google Scholar]
- 13.Beentje H, Adamson J, Bhanderi D. Kenya Trees, Shrubs, and Lianas. edn: National Museums of Kenya; 1994. [Google Scholar]
- 14.Agnew AD. Upland Kenya Wild Flowers and Fern. 3rd ed. Nairobi: Nature Kenya; The East Africa Natural History Society; 2013. [Google Scholar]
- 15.Pallant JF. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS. Sydney: Allen and Unwin; 2016. [Google Scholar]
- 16.Albuquerque UP, Lucena RF, Monteiro JM, Florentino AT, Cecília de Fátima C. Evaluating two quantitative ethnobotanical techniques. Ethnobotany Research and Applications. 2006;4:51–60. [Google Scholar]
- 17.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers' consensus and cultural importance. Soc Sci Med. 1998;47:1859–71. doi: 10.1016/s0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 18.Andrade-Cetto A, Heinrich M. From the field into the lab: Useful approaches to selecting species based on local knowledge. Front Pharmacol. 2011;2:20. doi: 10.3389/fphar.2011.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colón-Singh R. Mursik, Kenya's Secret Superfood: Kenyan Athletes are Famous for Winning Marathons and Competitions Around the World. Could Their Secret be a Little-known Super Food Known as ‘Mursik’? 2013. [Last accessed on 2016 Apr 15]. Available from: https://www.finedininglovers.com/stories/ash-yogurt-mursik-kenya-super-food/
- 20.Bett CK. Indigenous Milk Preservation Technology Among the Kalenjin of Kenya. 2011. [Last acessed on 2016 Jan 25]. Available from: http://www.agriculturesnetwork.org/magazines/eastafrica/63-regional-food-systems/indigenous-milk-preservation-kalenjin .
- 21.Kigen G, Maritim A, Some F, Kibosia J, Rono H, Chepkwony S, et al. Ethnopharmacological survey of the medicinal plants used in Tindiret, Nandi County, Kenya. Afr J Tradit Complement Altern Med. 2016;13:156–68. [Google Scholar]
- 22.Kamath JV, Rana AC. Preliminary study on antifertility activity of Calotropis procera roots in female rats. Fitoterapia. 2002;73:111–5. doi: 10.1016/s0367-326x(02)00005-9. [DOI] [PubMed] [Google Scholar]
- 23.Ndhlala AR, Ncube B, Okem A, Mulaudzi RB, Van Staden J. Toxicology of some important medicinal plants in Southern Africa. Food Chem Toxicol. 2013;62:609–21. doi: 10.1016/j.fct.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 24.Oboler R. Nandi and Other Kalenjin Peoples. Encyclopedia of World Cultures. 1996. [Last accessed on 2016 Apr 13]. Available from: http://www.encyclopedia.com/doc/1G2-3458001537.html .
- 25.Fouche G, Cragg GM, Pillay P, Kolesnikova N, Maharaj VJ, Senabe J. In vitro anticancer screening of South African plants. J Ethnopharmacol. 2008;119:455–61. doi: 10.1016/j.jep.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Adedapo AA, Jimoh FO, Afolayan AJ, Masika PJ. Antioxidant activities and phenolic contents of the methanol extracts of the stems of Acokanthera oppositifolia and Adenia gummifera. BMC Complement Altern Med. 2008;8:54. doi: 10.1186/1472-6882-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bisht P, Rawat V. Antibacterial activity of Withania somnifera against Gram-positive isolates from pus samples. Ayu. 2014;35:330–2. doi: 10.4103/0974-8520.153757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Girish KS, Machiah KD, Ushanandini S, Harish Kumar K, Nagaraju S, Govindappa M, et al. Antimicrobial properties of a non-toxic glycoprotein (WSG) from Withania somnifera (Ashwagandha) J Basic Microbiol. 2006;46:365–74. doi: 10.1002/jobm.200510108. [DOI] [PubMed] [Google Scholar]
- 29.Dikasso D, Makonnen E, Debella A, Abebe D, Urga K, Makonnen W, et al. Anti-malarial activity of Withania somnifera L. Dunal extracts in mice. Ethiop Med J. 2006;44:279–85. [PubMed] [Google Scholar]
- 30.Pant M, Ambwani T, Umapathi V. Antiviral activity of ashwagandha extract on infectious bursal disease virus replication. Indian J Sci Technol. 2012;5:2750–1. [Google Scholar]
- 31.Grover A, Agrawal V, Shandilya A, Bisaria VS, Sundar D. Non-nucleosidic inhibition of herpes simplex virus DNA polymerase: Mechanistic insights into the anti-herpetic mode of action of herbal drug withaferin A. BMC Bioinformatics. 2011;12(Suppl 13):S22. doi: 10.1186/1471-2105-12-S13-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tadeg H, Mohammed E, Asres K, Gebre-Mariam T. Antimicrobial activities of some selected traditional Ethiopian medicinal plants used in the treatment of skin disorders. J Ethnopharmacol. 2005;100:168–75. doi: 10.1016/j.jep.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 33.Yang N, Zhao M, Zhu B, Yang B, Chen C, Cui C, et al. Anti-diabetic effects of polysaccharides from Opuntia monacantha cladode in normal and streptozotocin-induced diabetic rats. Innov Food Sci Emerg Technol. 2008;9:570–4. [Google Scholar]
- 34.Saleem M, Irshad I, Baig MK, Naseer F. Evaluation of hepatoprotective effect of chloroform and methanol extracts of Opuntia monacantha in paracetamol-induced hepatotoxicity in rabbits. Banglad J Pharmacol. 2015;10:16–20. [Google Scholar]
- 35.Chaudhary MA, Imran I, Bashir S, Mehmood MH, Rehman NU, Gilani AH. Evaluation of gut modulatory and bronchodilator activities of Amaranthus spinosus Linn. BMC Complement Altern Med. 2012;12:166. doi: 10.1186/1472-6882-12-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Biglar M, Soltani K, Nabati F, Bazl R, Mojab F, Amanlou M. A preliminary investigation of the jack-bean urease inhibition by randomly selected traditionally used herbal medicine. Iran J Pharm Res. 2012;11:831–7. [PMC free article] [PubMed] [Google Scholar]
- 37.Gupta VK, Malhotra S. Pharmacological attribute of Aloe vera: Revalidation through experimental and clinical studies. Ayu. 2012;33:193–6. doi: 10.4103/0974-8520.105237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jana A, Biswas SM. Lactam nonanic acid, a new substance from Cleome viscosa with allelopathic and antimicrobial properties. J Biosci. 2011;36:27–35. doi: 10.1007/s12038-011-9001-9. [DOI] [PubMed] [Google Scholar]
- 39.Parameswari SA, Chetty CM, Chandrasekhar KB. Hepatoprotective activity of Ficus religiosa leaves against isoniazid rifampicin and paracetamol induced hepatotoxicity. Pharmacognosy Res. 2013;5:271–6. doi: 10.4103/0974-8490.118828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jain A, Soni M, Deb L, Jain A, Rout SP, Gupta VB, et al. Antioxidant and hepatoprotective activity of ethanolic and aqueous extracts of Momordica dioica Roxb. leaves. J Ethnopharmacol. 2008;115:61–6. doi: 10.1016/j.jep.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 41.Dudekula NK, Duza MB, Janardhan N, Duraivel S. Evaluation of the hepatoprotective activity of Rhus mysorensis in albino rats. Indian J Res Pharm Biotechnol. 2014;2:1010. [Google Scholar]
- 42.Yadav NP, Dixit VK. Hepatoprotective activity of leaves of Kalanchoe pinnata Pers. J Ethnopharmacol. 2003;86:197–202. doi: 10.1016/s0378-8741(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 43.Brands R. Iten, Home of Champions: Running in Iten. 2014. [Last accessed on 2016 Apr 08]. Available from: http://www.runninginiten.com/iten/


